Chapter: Obstetrics and Gynecology: Sexually Transmitted Diseases
Pelvic Inflammatory Disease
Pelvic Inflammatory Disease
Pelvic
inflammatory disease (PID) represents the mostserious
form of sexually transmitted disease. It involves infection of the upper
genital tract (endometrium, fallopian tubes, ovaries, and pelvic peritoneum) as
a result of direct spread of pathogenic organisms along mucosal surfaces after
initial infection of the cervix. The predominant organ-isms responsible for PID
are C. trachomatis and N. gonor-rhoeae. Other organisms that
have been isolated from thefallopian tubes of patients with PID include Mycoplasma,Streptococcus, Staphylococcus,
Haemophilus, Escherichia coli, bac-teroides, Peptostreptococcus, Clostridium, and Actinomyces.
Timing of cervical infection in
relation to the menstrual cycle is important; the endocervical mucus resists
upward spread, especially during the progesterone-dominant part of the cycle.
Oral contraceptives mimic this effect, which explains in part their action in
limiting PID. The presence of motile sperm or strings from intrauterine
contraceptives (IUC) can allow penetration of organisms through this
pro-tective barrier. Tubal ligation usually provides a barrier to spread,
although in some cases small micro-channels facil-itate continued spread. The
relative mobility of the fallo-pian tube probably contributes to the rapid and
widespread extension of infection.
RISK FACTORS
The greatest
risk factor for PID is prior PID. Adolescence,having multiple
sexual partners, not using condoms, and infection with any of the causative
organisms are impor-tant risk factors. Between 10% and 40% of women with
untreated chlamydial or gonorrheal infections of the cervix will develop acute
PID. The importance of early diag-nosis
and treatment of PID lies in its prevention of infertility and ectopic
pregnancy. Infertility results from scarring ofdamaged fallopian tubes and
intraperitoneal adhesions, and occurs in approximately 15% of patients after a
single episode of salpingitis, increasing to 75% after three or more episodes.
The risk of ectopic pregnancy is increased 7 to 10 times in women with a
history of salpingitis.
DIAGNOSIS
Findings in PID are often
nonspecific, and patients pre-senting with these symptoms should be
differentiated from those with ectopic pregnancy, septic incomplete abortions,
acute appendicitis, diverticular abscesses, and adnexal tor-sion. Patients with
PID may also present with only mild, nonspecific symptoms, such as vaginal
discharge or inter-mittent vaginal bleeding. More pronounced signs and symptoms
include muscular guarding, cervical motion ten-derness, or rebound tenderness.
A purulent cervical dis-charge is often seen, and the adnexa are usually
moderately to exquisitely tender with a mass or fullness potentially pal-pable.
Fever or chills may also be present and the white blood cell count is usually
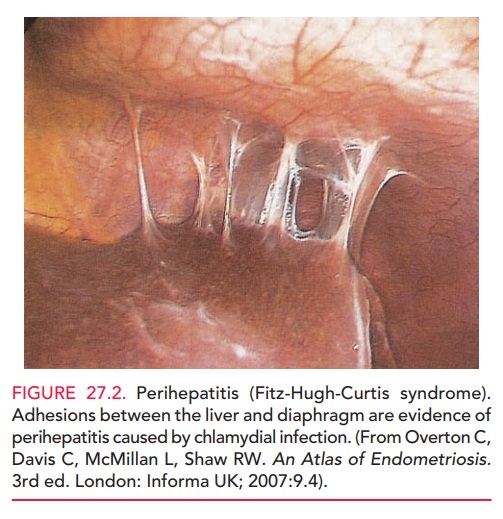
elevated (Box 27.2). Peritoneal involvement can also include perihepatitis (Fitz-Hugh-Curtis syndrome). Perihepatitis consists of
inflammationleading to localized fibrosis and scarring of the anterior surface
of the liver and adjacent peritoneum. It is probably caused by chlamydial
infection more often than by gonor-rheal infection, with which it was
originally described
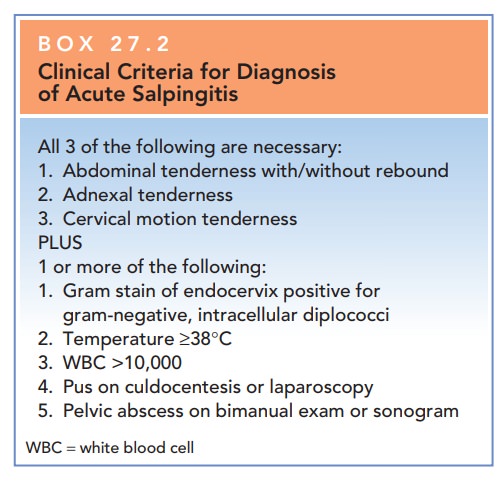
Box 27.2
Clinical Criteria for Diagnosis of Acute Salpingitis
All
3 of the following are necessary:
·
Abdominal
tenderness with/without rebound
·
Adnexal
tenderness
·
Cervical
motion tenderness
PLUS
·
1
or more of the following:
·
Gram
stain of endocervix positive for gram-negative, intracellular diplococci
·
Temperature
>=38°C
·
WBC
>10,000
·
Pus
on culdocentesis or laparoscopy
·
Pelvic
abscess on bimanual exam or sonogram
WBC
= white blood cell
In severe cases or in
patients with one or more prior episodes of PID, tuboovarian abscesses (TOA) may form. Patients with TOA are acutely
ill, often present-ing with high fever, tachycardia, severe pelvic and
abdom-inal pain, and nausea and vomiting.
Because PID may not be associated with specific signs and symptoms, empiric treatment for PID is recommended for sex-ually active young women who appear to have no other cause of illness and who are found to have uterine tenderness, adnexal tenderness, or cervical motion tenderness on pelvic examination. Women who are diagnosed with PID should also undergo testing for chlamydial, HIV, or gonorrheal infection.
TREATMENT
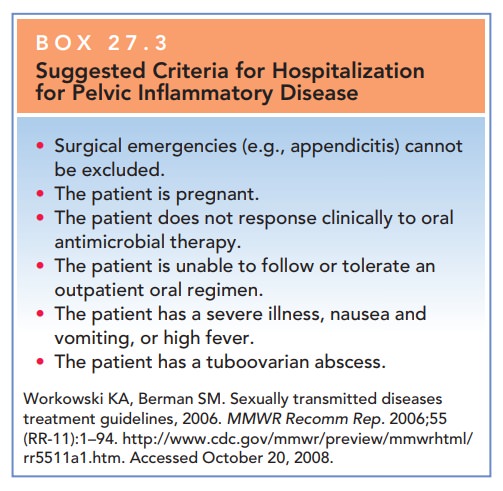
Patients with mild or moderate
cases of PID can be man-aged with an oral antibiotic regimen; however, many
pa-tients require hospitalization for adequate care. The decision for
hospitalization should be individualized and based on certain criteria (Box
27.3). Hospitalization allows for the administration of high-dose intravenous
antibiotic therapy with an antimicrobial spectrum that covers aero-bic and
anaerobic organisms. In the case of TOA, surgical drainage or even
hysterectomy, depending on the repro-ductive status and desires of the patient,
may be warranted in patients who do not respond to an aggressive course of
parenteral antibiotics. Rupture of a TOA with septic shock is a
life-threatening complication with mortality approach-ing 10%. These patients
must be treated surgically.
Related Topics