Chapter: Obstetrics and Gynecology: Sexually Transmitted Diseases
Genital Herpes
Genital Herpes
Genital
herpes is caused by infection with the herpes sim-plex
virus (HSV), a DNA virus. This condition affects more than 50 million persons
in the United States, and as many as 75% of primary infections go unrecognized
by either patient or provider. Herpes simplex infections are highly contagious.
There are two types of HSV—HSV-1, which is associated with cold sore lesions of
the mouth but may also cause genital lesions, and HSV-2. Most HSV genital
infections are caused by HSV-2, but genital HSV-1 infec-tions are becoming
increasingly common, particularly among adolescent and young women. Up to 80% of new gen-ital infections among
women may be due to HSV-1, with the highest rates occurring in adolescents and
young adults. Womeninfected with HSV-1 remain at risk for acquiring HSV-2
infection.
Box 27.3
Suggested Criteria for Hospitalization for Pelvic
Inflammatory Disease
·
Surgical
emergencies (e.g., appendicitis) cannot be excluded.
·
The
patient is pregnant.
·
The
patient does not response clinically to oral antimicrobial therapy.
·
The
patient is unable to follow or tolerate an outpatient oral regimen.
·
The
patient has a severe illness, nausea and vomiting, or high fever.
·
The
patient has a tuboovarian abscess.
Workowski
KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55 (RR-11):1–94. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5511a1.htm. Accessed October 20, 2008.
DIAGNOSIS
First episode infections, which
represent new acquisition of HSV, usually are most severe, and recurrent
infections may be milder. First episode
infections often are accompanied by sys-temic symptoms, including a prominent
flu-like syndrome and frequent neurologic involvement, which occur within 2 to
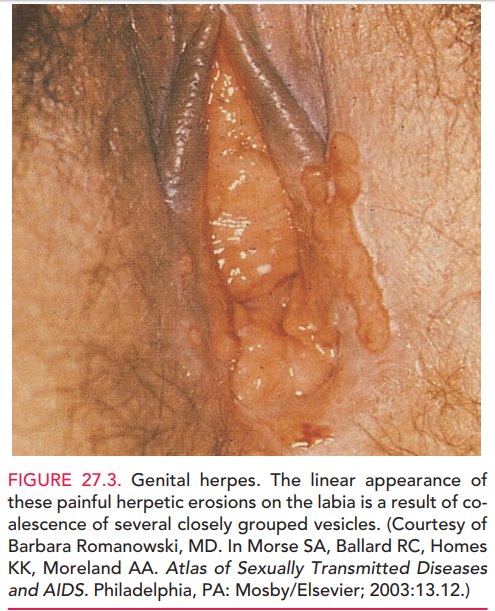
3 days following infection. Painful vesicular and ulcerated lesionsappear
on the vulva, vagina, cervix, or perineal and perianal skin, often extending
onto the buttocks, 3 to 7 days after exposure and usually resolving in
approximately 1 week (Fig. 27.3). These vesicles lyse and progress to shallow,
painful ulcers with a red border. The lesions of herpes sim-plex infections are
distinguishable from the ulcers found in chancroid, syphilis, or granuloma
inguinale by their appear-ance and extreme tenderness. Dysuria caused by vulvar
lesions or urethral and bladder involvement may lead to uri-nary retention.
Patients with primary lesions may require hospitalization for pain control or
management of urinary complications. Aseptic meningitis with fever, headache,
and meningismus occurs in some patients 5 to 7 days after the appearance of the
genital lesions.
After primary infection, the HSV
migrates via nerve fibers to remain dormant in the dorsal root ganglia.
Recurrences are triggered by unknown stimuli, resulting in the virus traveling
down the nerve fiber to the affected area. Recurrent
lesions are usually milder in severity than lesions asso-ciated with primary
infection and persist for a shorter duration, generally lasting 2 to 5 days. Recurrent
lesions may be unilat-eral rather than bilateral and present as fissures or
vulvar irritation, as opposed to being vesicular in appearance. Infections with
HSV-1 are less likely to cause recurrences than HSV-2, a fact that should be
considered when a patient is considering suppressive therapy.
Most HSV-1 and HSV-2 infections
are asymptomatic in women. The classic
presentation of a painful cluster of vesi-cles and ulcers occurs in a small
proportion of women, and most women will have atypical lesions, such as
abrasions, fissures, or itching without obvious lesions. Viral shedding can
occur forup to 3 weeks after lesions appear. Definitive diagnosis must be
confirmed with reliable laboratory testing.
The laboratory test used most
often has been viral culture. Culture is highly specific; however, it is not
very sensitive, with a false-negative rate of 25% with primary infection and as
high as 50% in a recurrent infection. PCR testing has a higher sensitivity and
will most likely replace culture in the future as the definitive test for HSV
infec-tion. In addition to viral detection methods, the detection of
type-specific antibodies to HSV-1 and HSV-2 also can help to establish the
diagnosis. These tests may yield false-negative test results when administered
in the early stages of infection, as the median time from infection to
serocon-version is 22 days. Approximately 20% of patients may remain
seronegative after 3 months, particularly if they have received antiviral
therapy. Type-specific testing may be useful in the following scenarios: (1)
recurrent genital or atypical symptoms with negative HSV cultures, (2)
clin-ical diagnosis of genital herpes in the absence of labora-tory diagnosis,
and (3) a partner with genital herpes.
TREATMENT
Antiviral
drugs are the mainstay of treatment. Oral med-ication can
reduce the duration of viral shedding and shorten the initial symptomatic
disease course, but it does not affect the long-term course of the disease.
Treatments for first episode genital herpes include acyclovir, famciclovir, or
valacyclovir. Treatment is usually prescribed for 7 to 10 days, but can be
given longer if new lesions persist. These therapies do not decrease the
likelihood of recurrence. Lesions should be kept clean and dry. In addition,
anal-gesics should be provided as needed (e.g., acetaminophen or ibuprofen).
Warm water baths often are helpful during the first few days. Topical lidocaine
also is occasionally beneficial, but it can result in local allergic reactions.
Severe episodes may require hospitalization for parenteral analgesia and
intravenous antiviral therapy. Such therapy is generally recommended for
immunosuppressed or other-wise compromised patients.
Recurrences may also be treated
with oral antiviral therapy. Episodic therapydecreases the duration of the episode(lesion, pain, and viral shedding)
and is most effective when the patient initiates the therapy at prodrome, or at
the beginning of the episode. Treatment regimens for recurrences are usu-ally
of a shorter duration than those administered for first episodes (3 to 5 days).
Episodic therapy is recommended for patients with infrequent symptomatic
recurrences. Suppressive therapy for
genital herpes (in which the medica-tion is taken daily) prevents approximately
80% of recurrences and results in a 48% reduction in viral transmission between
sexual partners as a result of decreased viral shedding. It may be most
effective for patients with frequent occurrences. It shouldalso be
recommended for women with HSV-2 whose sex-ual partner does not have HSV or who
has HSV-1 infec-tion. Such discordant couples should also be advised that
consistent use of condoms decreases, but does not elimi-nate the risk of
transmission.
Pregnant women with a history of
genital herpes should be carefully screened throughout the prenatal course for
evi-dence of outbreaks. Cesarean delivery
is indicated for womenwith active lesions or a typical herpetic prodrome at the
time of delivery to prevent neonatal transmission.
Human Papillomavirus
Human papillomavirus (HPV) is extremely common,occurring in up to 80% of sexually active women by age 50. Transmission occurs through contact with infected genital skin, mucous membranes, or body fluids from a partner with either overt or subclinical HPV infections. HPV is species-specific and only infects humans. Most infections are transient, but the proportion of women whose infec-tions resolve decreases with age. Unlike other STDs, seque-lae of HPV infection may take years to develop. More than 100 HPV subtypes have been identified, with at least 40 identified in genital infections. HPV viral types are rou-tinely classified into low-risk and high-risk categories. Low-risk subtypes, such as 6 and 11, are typically associated with genital condyloma. High-risk subtypes, such as 16, 18, 31, 33, and 45, are so classified because of their association with cervical dysplasia and cervical cancer. Of the high-risk subtypes, HPV16 and 18 together account for approximately two-thirds of cervical cancer cases, whereas low-risk HPV subtypes rarely lead to cancer.
CONDYLOMA ACUMINATA
Condyloma
acuminata (genital or venereal warts) aresoft, fleshy growths
that may arise from the vulva, vagina, cervix, urethral meatus, perineum, and
anus (Fig. 27.4). They may occasionally also be found on the tongue or oral cavity.
These distinctive lesions may be single or multiple and generally cause few
symptoms. They are often accom-panied by other STDs. Because HPV is spread by
direct skin-to-skin contact, symmetrical lesions across the mid-line are
common.
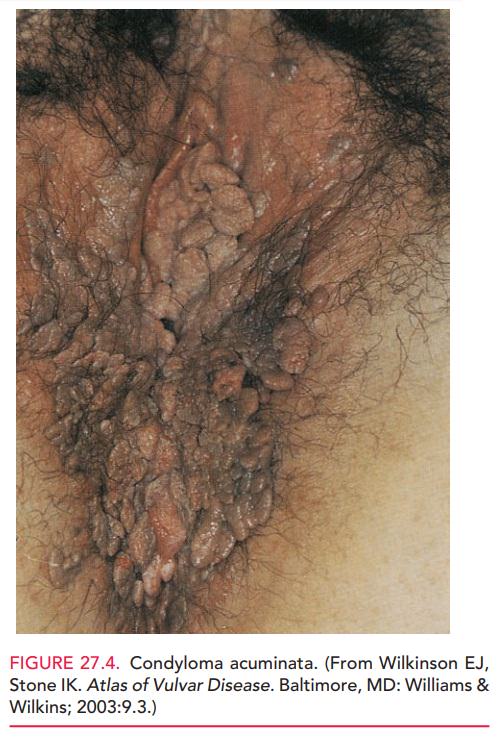
The diagnosis of condyloma acuminata is based on physical examination, but may be confirmed through biopsy of the warts.
Thorough inspection of the external genitalia and anogenital region
should be performed during the routine gynecologic examination, especially in
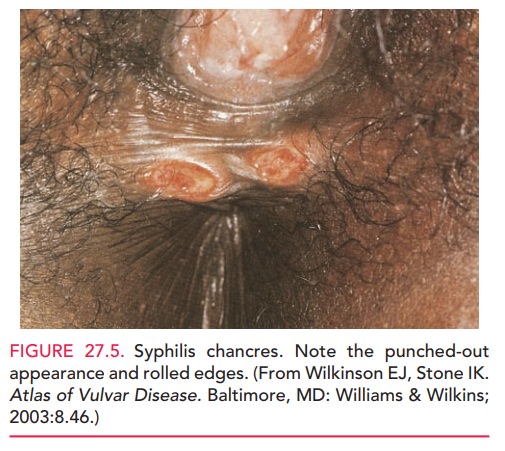
patients with known cervical or vaginal lesions. Because the condyloma lata of
syphilis may be confused with gen-ital warts, the clinician must be able to
distinguish the two types of lesions in patients at high risk for both
infections (see Fig. 27.5 photo of syphilis).
Management options include
chemical treatments, cautery, and immunologic treatments. Patient-applied
products include podofilox and imiquimod; these treat-ments should not be used
during pregnancy. Treatments that are administered by a healthcare provider
include application of trichloroacetic acid, application of podo-phyllin resin
in tincture of benzoin, cryosurgery, surgical excision, laser surgery, or
intralesional interferon injec-tions. Lesions exceeding 2 cm respond best to
cryother-apy, cautery, or laser treatment.
Lesions are more resistant to
therapy in patients who are pregnant, have diabetes, smoke, or are
immunosup-pressed. In patients with extensive vaginal or vulvar lesions,
delivery via cesarean section may be required, to avoid extensive vaginal
lacerations and problems with suturing tissues with these lesions. Cesarean
delivery also decreases the possibility of transmission to the infant, which
can cause subsequent development of laryngeal papillomata, although the risk is
small and is not considered an indica-tion for cesarean delivery.
CERVICAL DYSPLASIA
The
relationship between infection by high-risk subtypes and cervical dysplasia and
cancer is now well-established. A
quadri-valent HPV vaccine protects
against HPV genotypes 6, 11, 16, and 18 (the strains of HPV that cause 90% of
genital warts and 70% of cervical cancers). Additional vaccines are also
beinginvestigated.
ACOG
currently recommends that all girls and women aged 9 to 26 years be immunized
against HPV. The vaccine isa protective tool and is not a
substitute for cancer screen-ing; women should be advised to follow current
cervical cytologic screening guidelines regardless of their vaccina-tion
status.
Related Topics