Chapter: Essentials of Psychiatry: Social Psychology
Social Psychology: Social Cognition
Social Cognition
Social cognition – the ways social events are
interpreted, analyzed and mentally represented – provides an
information-processing framework for understanding how construals of self and
others affect social discourse and psychological life (Fiske and Taylor, 1991).
Social cognition concepts have influenced traditional areas of social
psychological theory and research, including attribution processes, person perception,
and attitude formation and change. Over time, the information processing
emphasis of social cogni-tion has been integrated with concepts of motivation
and emotion to create a fuller view of the individual in relation to the social
world (Taylor, 1998).
Attribution Processes
Attribution processes refer to causal explanations
generated by an individual to account for why a particular event or set of
out-comes has occurred. People use attributions to make sense of their own
behavior and that of others, and, therefore, attribution processes influence
individual actions, affective experiences and
interpersonal behavior (Weiner and Graham, 1999).
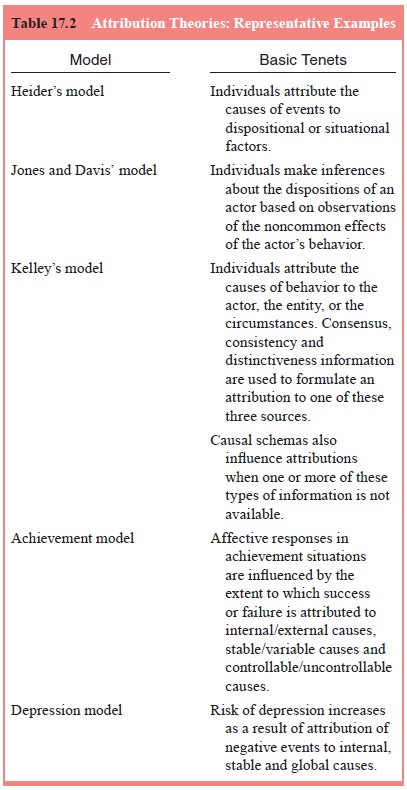
Attribution theory (Table 17.2) and research has been a mainstay of social
psychology and has led to important clinical mental health ap-plications
(Bell-Dolan and Anderson, 1999; Forsterling, 2001; Graham and Folkes, 1990).
Attribution Biases
Based on the proliferation of research stimulated
in the 1970s by social psychological models of causal attribution, three major
types of attribution biases in everyday social interactions were illuminated:
the fundamental attribution error (Ross, 1977), the actor–observer bias (Jones
and Nisbett, 1971) and the self-serving (hedonic) attribution bias (Bradley,
1978) (Table 17.3).
The fundamental attribution error – a bias toward
at-tributing behavior to dispositional factors in the actor while
underestimating the influence of situational variables – typically occurs in
the context of understanding the behavior of others.
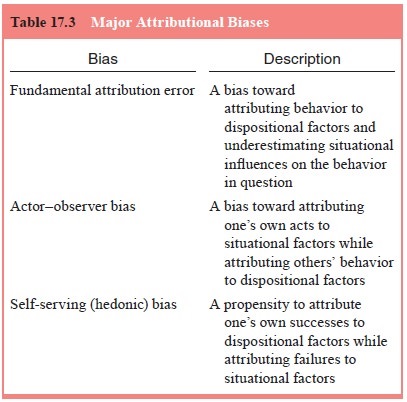
The actor–observer bias refers to instances in
which individuals attribute their own acts to situational factors and minimize
the role of dispositional qualities, attributing the others’ behavior to
dispo-sitional factors. Actor–observer differences may be a function of greater
self-knowledge than knowledge of others, or related to dif-fering perspectives
between actors and observers that lead to dif-ferent causal interpretations.
The self-serving (hedonic) attribution bias involves a propensity to attribute
one’s successes to disposi-tional factors and one’s failures to situational
causes. Specifically, the self-serving bias reflects a wish to present oneself
in the best possible light. People tend to extend this attribution bias to
impor-tant others in their interpersonal sphere (e.g., spouse). Multiple
ex-planations have been offered in the literature regarding the causal
underpinnings of these attribution biases (Forsterling, 2001).
Attributions in Health and Illness
Given that attribution processes tend to be
activated by negative, unanticipated, or ambiguous events, it is logical to
assume that attribution theory would have a useful role in conceptualizing how
people come to understand the causes of their illness as well as processes of
stress and coping with illness (Amirkhan, 1990; Salovey et al., 1998). Empirical evidence supports this view, as
exemplified in a recent meta-analytic study that suggested that attributions
influence illness-related coping and adjust-ment (Roesch and Weiner, 2001).
Attributions influence one’s self-definitions in relation to the illness, as
well as one’s percep-tions of control over illness-related contingencies and
outcomes. However, associations between specific attributions and illness
should not be interpreted to mean that certain attribution patterns cause
illness, but rather that they may be among a complex set of factors affecting
responses to illness.
It is clear that causal attributions are important
in facilitat-ing health promotion and positive health practices (Rodin and
Salovey, 1989; Salovey et al., 1998).
To the extent possible, treat-ment interventions with medically ill persons
should incorporate a focus upon enhancing the individual perceptions of control
over health and treatment regimens with the aim of increasing adher-ence to
medical regimens and improving adjustment to medical procedures and conditions.
Existing research also underscores the importance of considering locus,
stability and controlla-bility dimensions of the attribution process in
understanding illness-related attribution processes and their role in
predicting patient perceptions of medical treatment (Amirkhan, 1990).
Mental Health Implications: Attribution Processes
Theoretical models and research have significant
implications for mental health treatment (Bell-Dolan and Anderson, 1999;
Forsterling, 2001; Weiner and Graham, 1999). Presumably, at-tribution models
can be instructive for designing interventions that target causal inferences
associated with problematic emo-tion states (e.g., guilt), moods (e.g.,
depression) and behavioral constellations (e.g., social avoidance) (Bell-Dolan
and Anderson, 1999). The application of attribution models to depression is
illustrative of this point.
Hopelessness Theory of Depression
The use of attribution concepts, including the
notion of attribu-tional style, in understanding learned helplessness and
depression led to the formulation that the presence of a pessimistic
attribu-tional style increased the risk that an individual would experi-ence
helplessness, hopelessness and depression (Abramson et al., 1978). This attribution dimension was later incorporated as
a key component of the hopelessness theory of depression (Abramson et al., 1989; Gotlib and Abramson, 1999).
This model predicts that an
individual is at risk for hopelessness depression to the extent that negative
events are attributed to internal, stable and global causes, and that these
causes are perceived as both likely to prompt other negative consequences and
to be reflective of deficiencies or shortcomings of self. The model also posits
that a given individual’s causal attributions are a function of both
situational factors and individual differences in attributional style. Further,
cognitive vulnerability to hopelessness depression is conceptualized as a
function of individual differences in at-tributional style as well as the
propensity to infer negative consequences and negative self-evaluation in
response to adverse events (Gotlib and Abramson, 1999).
Person Perception and Implicit Personality Theories
Person perception, also referred to as social
perception, pertains to the ways in which people formulate impressions of
others (Leyens and Fiske, 1994). Person perception can be conceptu-alized broadly
as involving three sequential processes: 1) the identification of meaningful
acts by observation of overt actions based on the actor’s intentions or traits;
2) the formation of attri-butions about the acts; and 3) the integration of
attribution infer-ences into a unified impression of an individual (Gilbert,
1998). Social psychologists have long suggested that people formulate implicit
personality theories that consist of general beliefs about human
characteristics and patterns of covariation among person-ality traits
(Schneider, 1973). These knowledge systems facili-tate rapid formation of
inferences about the enduring personality qualities of other people in everyday
life by using assumptions about interrelationships among dispositional
qualities to draw conclusions about observed behavior. More recently, schema
concepts in social cognition have been investigated in order to specify
cognitive processes through which individuals organize and represent coherent
and meaningful impressions of others (Leyens and Fiske, 1994).
Although person perception variables per se have
not been explicitly discussed in the context of health issues, one particularly
useful application of this literature is in understand-ing relationships
between patients and their health care provid-ers. The doctor–patient
relationship is influenced in part by the affective and cognitive evaluations
that each make regarding the other. These person perception variables affect
interaction styles between physicians and their patients which, in turn, may
influence the nature and quality of medical care. Patients’ perceptions of
their physicians as paternalistic, interested in mutuality in decision-making
regarding care, or expecting them (the patient) to have primary responsibility
for decision-making will contribute to differential doctor–patient interaction
dynam-ics (Shelton, 1998). Similarly, the degree to which the physician’s
impression of the patient is that of a passive novice, informed part-ner, or
the consumer in charge of care will affect doctor–patient interactions.
Person perception has clinical relevance for the
cognitive interpretation of interpersonal situations. Many of the cognitive
distortions (e.g., overgeneralization, magnification and minimi-zation)
observed in depressed persons (Beck et al.,
1979), anxious individuals (Beck et al.,
1985), and people with personality disorders (Beck and Freeman, 1990) influence
person perception in a maladaptive fashion. Thus, while person perception
research has demonstrated a normative tendency to make rapid evalua-tions of
others and interpersonal situations based on limited information, this process
is apt to become problematic when cognitive distortions are operative. For
example, the depressed person with low self-esteem and a pessimistic
attributional style who, based on a few experiences of being criticized,
perceives others as judgmental in virtually every interpersonal interac-tion is
overgeneralizing based upon limited data (i.e., “others are always critical of
me”). This is likely to interfere with the development of trusting
relationships.
Implicit personality theories and schemas in social
cognition are clinically applicable to understanding chronically maladap-tive
person perception processes. This may have particular rel-evance for the
clinical understanding of personality disorders. For example, the patient with
paranoid personality disorder may hold a pervasive view of others as
potentially attacking, blaming and controlling (Benjamin, 1996). The patient
with borderline personality disorder may perceive others as simultaneously
rejecting, abandoning and needing dependent others (Benjamin, 1996). The
patient with obsessive–compulsive personality dis-order may believe that others
expect perfection regardless of the individual’s own wants and needs (Benjamin,
1996). To address these maladaptive implicit personality theories, schemas and
associated interaction patterns, effective psychotherapy helps patients
identify dysfunctional person perceptions, develop an affective and cognitive
awareness of the etiology of these beliefs and the functions they serve, and
form more adaptive schemas of self in relation to others (Benjamin, 1996).
Additionally, thera-pists’ awareness of problematic schemas and implicit
personality theories early in treatment can assist in assessment and
identifi-cation of interpersonal patterns that are likely to be enacted in the
therapeutic relationship.
Attitudes
Attitudes refer to evaluations made by people along
a contin-uum from positive to negative about specific entities called at-titude
objects (e.g., ideas, concrete things, life events, social groups, classes of
behavior, persons) (Eagly and Chaiken, 1998). Individual attitudes consist of
three elements: cognitive (beliefs about attitude objects), affective (emotions
elicited by attitude ob-jects) and behavioral (action intentions or overt
behavior directed toward attitude objects). Additionally, individual attitudes
may be associatively or logically linked to form broader inter-attitu-dinal
structures consisting of two or more attitudes (Eagly and Chaiken, 1998).
Attitudes provide a framework for rapid appraisal and evaluative interpretation
of one’s world, thereby allowing one to formulate responses to the complexities
and ambiguities of daily living in an economical fashion, often without the
need for deliberate, conscious processing (Cooper and Aronson, 1992).
Fundamentally, attitudes serve an important adaptive function by virtue of
their evaluative properties involving distinctions of good stimuli presumed to
enhance well-being from bad stimuli that could endanger well-being (Eagly and
Chaiken, 1998).
Attitude Theories
Attitude theory and research has a rich history as
one of the great areas of inquiry within social psychology (Eagly and Chaiken,
1998; Petty and Wegener, 1998). However, this voluminous and intricate
literature can be encapsulated only briefly here. Theo-retical frameworks
developed in the 1950s, 1960s and 1970s that laid the foundation for later
social psychological inquiries into attitudes (Table 17.4).
Learning and reinforcement theories of attitude
formation and change, founded on principles of behaviorism, were derived
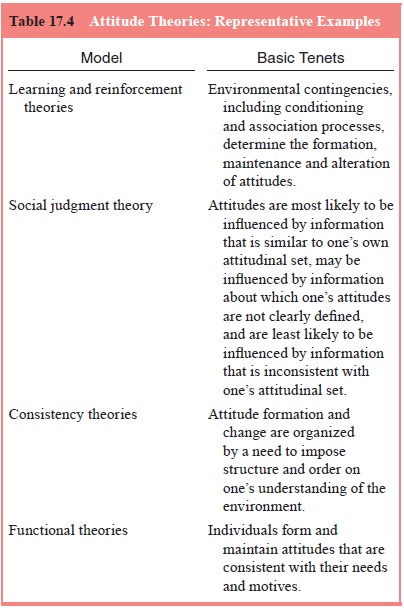
from basic experimental psychology. Two major
examples are conditioning (Staats and Staats, 1958) and associationist
(stimulus–response) (Hovland et al.,
1953) perspectives. These approaches emphasize the influence of stimulus
pairing and stimulus–response patterns in attitude formation (Eagly and
Chaiken, 1998).
Social judgment theory emphasizes the interplay of
cogni-tive and affective attitudinal components and posits that percep-tions
and judgments mediate attitude change (Sherif et al., 1965). According to this approach, attitudes are most
likely to be influ-enced by information that is similar to one’s existing
attitudinal set (i.e., latitude of acceptance), may be influenced by
informa-tion about which one’s attitudinal set is not clearly defined and
affectively neutral (i.e., latitude of noncommitment), and least likely to be
influenced by information that is inconsistent with one’s attitudinal set
(i.e., latitude of rejection).
Consistency theories posit that attitude formation
and change are organized by a need to impose structure and order on one’s
understanding of the environment. Cognitive dissonance theory (Festinger, 1957)
posited that discrepancies between simultaneously held attitudinal cognitions
(dissonance) produced psychological tension, requiring attitudinal changes to
reestablish consistency (consonance). The degree to which this dissonance
causes psychological tension is a function of the per-sonal importance of the
cognitions and the number of dissonant cognitions relative to consonant
cognitions.
An alternative approach that proposed to account
for re-search findings regarding dissonance was self-perception theory (Bem,
1972). According to this perspective, individuals infer their attitudes through
observing their own behavioral responses and the conditions under which they
occur. From this view, at-titudes are formed on the basis of self-attributions
(Cooper and Aronson, 1992).
The final group of attitude theories – functional
theories – hold that individuals form and maintain attitudes consistent with
their needs and motives (Katz, 1960; Kelman, 1961; Smith et al., 1956). For example, particular attitudes may be adopted for
adjustment, instrumental, or utilitarian purposes, as they maximize rewards and
minimize punishments. Attitudes also may serve a value expression function.
Ego-defensive or ex-ternalizing functions of attitudes allow for maintenance of
de-sired views of self and the world, while protecting the individual from
acknowledgement of unpleasant realities. Attitudes serving a knowledge function
assist people in formulating meaning about events in their world. Functional
models suggest a complex interplay among different attitudinal beliefs,
necessitating dif-ferent change strategies based upon the function of the
attitude being targeted for change (Eagly and Chaiken, 1998).
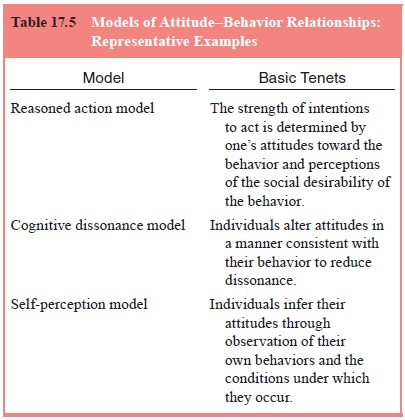
Interest in enhancing precision in the prediction
of behav-ioral responses from attitudinal beliefs prompted efforts to de-velop
models of the attitude–behavior relationship (Table 17.5). Two broad types of
models include those focusing on attitudes toward targets of behavior and those
focusing on attitudes toward behavior (Eagly and Chaiken, 1998).
Attitudes in Health and Illness
People’s attitudes affect whether or not they practice adap-tive or maladaptive health behaviors. Accordingly, it has been suggested that information aimed at promoting behaviors that reduce health risk should focus on attitudinal and normative beliefs influencing the behavior in question. The goal of such interventions is to bolster intentions to engage in or abstain from the target behavior.
Although not an attitude theory per se, the health
belief model (Rosenstock et al.,
1988; Strecher et al., 1997) is a
well-known social psychological model explicitly formulated to understand
health-related behavior practices. The health be-lief model posits that
individuals are motivated to respond to perceived threats of illness, with
threat defined in terms of per-ceptions regarding seriousness of and personal
susceptibility to an illness. Behavioral responses to health-related threats
are influenced by expectations regarding the ability to minimize such a threat,
including perceived benefits and problems associated with a given response
pattern. Sociocultural and demographic factors as well as personal and
environmental cues regarding ap-propriate courses of action also are considered
in the model. The model predicts that people are likely to take steps to
minimize the risk of contracting a medical problem if the following condi-tions
occur: 1) they view themselves as vulnerable to a particular health condition;
2) they deem the condition to be personally con-sequential; 3) they believe
that a specific course of action would minimize vulnerability to the condition
and that limitations as-sociated with such actions are outweighed by the
potential ben-efits to be accrued; and 4) they perceive themselves as capable
of performing these actions (i.e., self-efficacy). Researchers have examined
the utility of the health belief model in informing pre-vention and
intervention approaches for medically ill individuals and those at risk for
specific illnesses (Salovey et al.,
1998).
Attitudes can have an important impact on
psychological outlook and functioning. Whereas individuals who evidence
positive mental health possess flexible attitudes that are adaptive to the
context, persons with psychological difficulties evidence rigidly held
maladaptive attitudes that impair their capacity to cope effectively with
life’s challenges. This suggests that helping patients identify and modify
maladaptive attitudes about self and others can be an important component of
psychotherapeutic intervention (Cooper and Aronson, 1992).
Related Topics