Chapter: Clinical Dermatology: The function and structure of the skin
Skin Dermis
Dermis
The
dermis lies between the epidermis and the sub-cutaneous fat. It supports the
epidermis structurally and nutritionally. Its thickness varies, being greatest
in the palms and soles and least in the eyelids and penis. In old age, the
dermis thins and loses its elasticity.
The
dermis interdigitates with the epidermis (Fig. 2.1) so that upward projections
of the dermis, the dermal papillae, interlock with downward ridges of the
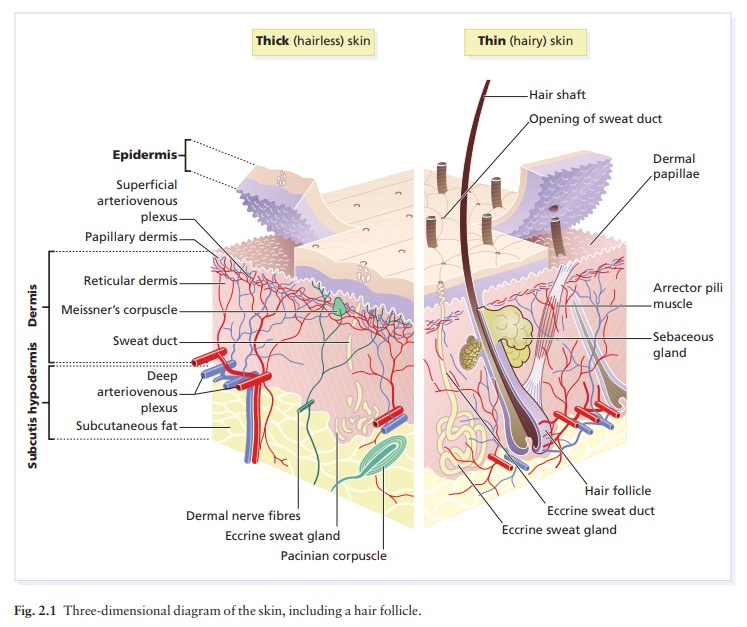
This interdigitation is respons-ible for the ridges seen most
readily on the fingertips (as fingerprints). It is important in the adhesion
between epidermis and dermis as it increases the area of con-tact between them.
Like
all connective tissues the dermis has three com-ponents: cells, fibres and
amorphous ground substance.
Cells of the dermis
The
main cells of the dermis are fibroblasts, but there are also small numbers of
resident and transitory mono-nuclear phagocytes, lymphocytes, Langerhans cells
and mast cells. Other blood cells, e.g. polymorphs, are seen during
inflammation.
Fibres of the dermis
The
dermis is largely made up of interwoven fibres, principally of collagen, packed
in bundles. Those in the papillary dermis are finer than those in the deeper
reticular dermis. When the skin is stretched, collagen, with its high tensile
strength, prevents tearing, and the elastic fibres, intermingled with the
collagen, later return it to the unstretched state.
Collagen
makes up 70–80% of the dry weight of the dermis. Its fibres are composed of
thinner fibrils, which are in turn made up of microfibrils built from
indi-vidual collagen molecules. These molecules consist of three polypeptide
chains (molecular weight 150 kDa) forming a triple helix with a non-helical
segment at both ends. The alignment of the chains is stabilized by covalent
cross-links involving lysine and hydroxylysine. Collagen is an unusual protein
as it contains a high proportion of proline and hydroxyproline and many glycine
residues; the spacing of glycine as every third amino acid is a prerequisite
for the formation of a triple helix. Defects in the enzymes needed for collagen
syn-thesis are responsible for some skin diseases, including the Ehlers–Danlos
syndrome, and con-ditions involving other systems, including lathyrism
(fragility of skin and other connective tissues) and osteogenesis imperfecta
(fragility of bones).
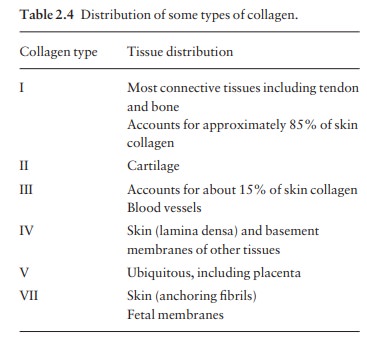
There
are many, genetically distinct, collagen pro-teins, all with triple helical
molecules, and all rich in hydroxyproline and hydroxylysine. The distribution
of some of them is summarized in Table 2.4.
Reticulin
fibres are fine collagen fibres, seen in fetalskin and
around the blood vessels and appendages of adult skin.
Elastic fibres
account for about 2% of the dry weightof adult dermis. They have two distinct
protein com-ponents: an amorphous elastin core and a surround-ing ‘elastic
tissue microfibrillar component’. Elastin (molecular weight 72 kDa) is made up
of polypeptides (rich in glycine, desmosine and valine) linked to the microfibrillar
component through their desmosine residues. Abnormalities in the elastic tissue
cause cutis laxa (sagging inelastic skin) and pseudoxanthoma elasticum.
Ground substance of the dermis
The
amorphous ground substance of the dermis con-sists largely of two
glycosaminoglycans (hyaluronic acid and dermatan sulphate) with smaller amounts
of heparan sulphate and chondroitin sulphate. The glycosaminoglycans are
complexed to core protein and exist as proteoglycans.
The
ground substance has several important functions:
•
it binds water, allowing nutrients,
hormones and waste products to pass through the dermis;
•
it acts as a lubricant between the
collagen and elastic fibre networks during skin movement; and
•
it provides bulk, allowing the
dermis to act as a shock absorber.
Muscles
Both
smooth and striated muscle are found in the skin. The smooth arrector pili
muscles (see Fig. 13.1) are used by animals to raise their fur and so protect
them from the cold. They are vestigial in humans, but may help to express
sebum. Smooth muscle is also responsible for ‘goose pimples’ (bumps) from cold,
nipple erection, and the raising of the scrotum by the dartos muscle. Striated
fibres (e.g. the platysma) and some of the muscles of facial expression, are
also found in the dermis.
Blood vessels
Although
the skin consumes little oxygen, its abund-ant blood supply regulates body
temperature. The blood vessels lie in two main horizontal layers (Fig. 2.10).
The deep plexus is just above the subcutaneous fat,
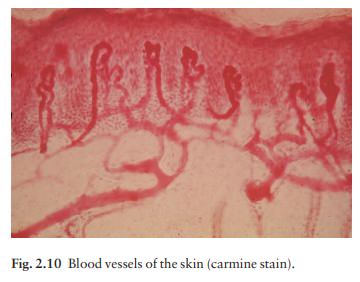
The superficial
plexus is in the papillary dermis and arterioles from it become capillary loops
in the dermal papillae. An arteriole arising in the deep dermis supplies an
inverted cone of tissue, with its base at the epidermis.
The
blood vessels in the skin are important in thermoregulation. Under sympathetic
nervous control, arteriovenous anastamoses at the level of the deep plexus can
shunt blood to the venous plexus at the expense of the capillary loops, thereby
reducing sur-face heat loss by convection.
Cutaneous lymphatics
Afferent
lymphatics begin as blind-ended capillaries in the dermal papilla and pass to a
superficial lymphatic plexus in the papillary dermis. There are also two deeper
horizontal plexuses, and collecting lymphatics from the deeper one run with the
veins in the super-ficial fascia.
Nerves
The
skin is liberally supplied with an estimated one million nerve fibres. Most are
found in the face and extremities. Their cell bodies lie in the dorsal root
ganglia. Both myelinated and non-myelinated fibres exist, with the latter
making up an increasing pro-portion peripherally. Most free sensory nerves end
in the dermis; however, a few non-myelinated nerve endings penetrate into the
epidermis. Some of these are associated with Merkel cells. Free nerve endings
detect the potentially damaging stimuli of heat and pain (nocioceptors), while
specialized end organs in the dermis, Pacinian and Meissner corpuscles,
register deformation of the skin caused by pressure (mechanoreceptors) as well
as vibration and touch. Autonomic nerves supply the blood vessels, sweat glands
and arrector pili muscles.
Itching
is an important feature of many skin diseases. It follows the stimulation of
fine free nerve endings lying close to the dermo-epidermal junction. Areas with
a high density of such endings (itch spots) are especially sensitive to
itch-provoking stimuli. Impulses from these free endings pass centrally in two
ways: quickly along myelinated A fibres, and more slowly along non-myelinated C
fibres. As a result, itch has two components: a quick localized pricking
sensation followed by a slow burning diffuse itching.
Many
stimuli can induce itching (electrical, chemical and mechanical). In itchy skin
diseases, pruritogenic chemicals such as histamine and proteolytic enzymes are
liberated close to the dermoepidermal junction. The detailed pharmacology of
individual diseases is still poorly understood but prostaglandins potenti-ate
chemically induced itching in inflammatory skin diseases.
Related Topics