Chapter: Medical Surgical Nursing: End-of-Life Care
Settings for End-of-Life Care: Hospice Care
HOSPICE
CARE
Hospice in the United States is not a place, but a concept of care in
which the end of life is viewed as a developmental stage. The root of the word
hospice is hospes, meaning “host.”
Historically, hospice has referred to a shelter or way station for weary
travelers on a pilgrimage (Bennahum, 1996). In the years that followed
Kübler-Ross’s groundbreaking work, the concept of hospice care as an
alternative to depersonalized death in institutions began as a grassroots
movement. Her work, and the development of the con-cept of hospice in England
by Dr. Cicely Saunders, resulted in recognition of gaps in the existing system
of care for the terminally ill (Amenta, 1986). Hospice care began in response
to “noticeable gaps . . . (1) between treating the disease and treating the
person, (2) between
technological research and psycho-social support, and
(3) between
the general denial of the fact of death in our society and the acceptance of
death by those who face it”. According to Saunders, who founded the
world-renowned St. Christopher’s Hospice in London (Bennahum, 1996), the
principles underlying hospice are as follows:
·
Death
must be accepted.
·
The patient’s
total care is best managed by an interdisciplinary team whose members
communicate regularly with each other.
·
Pain
and other symptoms of terminal illness must be managed.
·
The
patient and family should be viewed as a single unit of care.
·
Home
care of the dying is necessary.
·
Bereavement
care must be provided to family members.
·
Research
and education should be ongoing.
Hospice Care in the United States
Although the concept dates to ancient times, hospice as a way of caring
for those at the end of life did not emerge in the United States until the
1960s (Hospice Association of America, 2001). The hospice movement in the
United States is based on the be-lief that meaningful living is achievable
during terminal illness, and that it is best supported in the home, free from
technologi-cal interventions to prolong physiologic dying (Amenta, 1986). After
the first U.S. hospice was founded in Connecticut in 1974, the concept quickly
spread and the number of hospice programs in the United States has grown
dramatically. In the years between 1984 and 1996, which followed the creation
of the Medicare Hospice Benefit, there was a 70-fold increase in the number of
hospices participating in Medicare (Hospice Association of America, 2001).
Despite more than 25 years of existence in the United States, hospice
remains an option for end-of-life care that has not been fully integrated into
mainstream health care. Although hospice care is available to persons with any
life-limiting condition, it has primarily been used by patients with advanced
cancer, where the disease staging and trajectory lend themselves to more
reliableprediction about the end of life (Boling & Lynn, 1998; Christakis
Lamont, 2000). Many reasons have been proposed for the re-luctance of
physicians to refer patients to hospice and the reluc-tance of patients to
accept this form of care. These include the difficulties in making a terminal
prognosis, the strong association of hospice with death, advances in “curative”
treatment options in late-stage illness, and financial pressures on health care
providers that may cause them to retain rather than refer hospice-eligible
patients. The result is that patients who could benefit from the comprehensive,
interdisciplinary support offered by hospice pro-grams frequently do not enter
hospice care until their final days (or hours) of life (Christakis &
Lamont, 2000).
Hospice is a coordinated program of interdisciplinary services provided
by professional caregivers and trained volunteers to pa-tients with serious,
progressive illnesses that are not responsive to cure. In hospice settings, the
patient and family together are the unit of care. The goal of hospice care is
to enable the patient to remain at home, surrounded by the people and objects
that have been important to him or her throughout life. Hospice care does not
seek to hasten death, nor does it encourage the prolongation of life through
artificial means. Hospice care hinges on the com-petent patient’s full or
“open” awareness of dying; it embraces a realism about death, such that the
patient and family are assisted to understand the dying process and can live
each moment as fully as possible.
Although most hospice care is provided in the patient’s own home, some
hospice programs have developed inpatient facilities or residences where
terminally ill patients without family support or those who desire inpatient
care may receive hospice services.
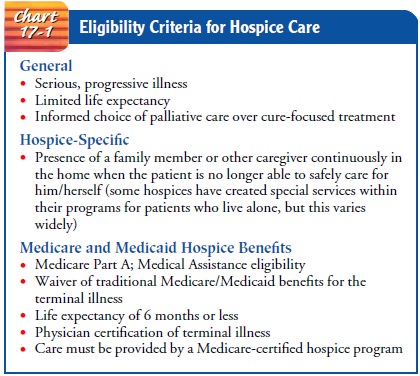
Eligibility criteria for
hospice vary depending on the hospice program, but generally patients must have
a progressive, irre-versible illness and limited life expectancy and have opted
for pal-liative care rather than cure-focused treatment. Although hospices have
historically served cancer patients, patients with any life-limiting illness
are eligible.
Medicare Hospice Benefit
In 1983, the Medicare Hospice Benefit was implemented to cover hospice
care for Medicare beneficiaries. State Medical Assistance (Medicaid) also
provides coverage for hospice care, as do most com-mercial insurers. Federal
reimbursement for hospice care ushered in a new era in hospice in which program
standards developed and published by the federal government codified what had
formerly been a grassroots, loosely organized and defined ideal for care at the
end of life. To receive Medicare dollars for hospice services, pro-grams are
required to comply with conditions of participation pro-mulgated by the Centers
for Medicare and Medicaid Services. Medicare standards have come to largely
define hospice philosophy and services. Eligibility criteria for hospice
coverage under the Medicare Hospice Benefit are specified in Chart 17-1.
Federal rules for hospices require that the patient’s continuing eligibility
for hos-pice care is reviewed periodically. There is no limit to the length of
time that an eligible patient may continue to receive hospice care. Patients
who live longer than 6 months under hospice care are not discharged if their
physician and the hospice medical direc-tor continue to certify that the
patient is terminally ill with a life expectancy of 6 months or less, assuming
that the disease con-tinues its expected course. The hospice certification and
review process and the open-ended benefit structure are intended to ad-dress
the difficulty physicians face in predicting how long a patient will live, so
that patients are not restricted to a lifetime limit on the number of hospice
days they may receive.
To use hospice benefits under Medicare or Medicaid, the pa-tient must
meet eligibility criteria and “elect” to use the hospice benefit in place of
traditional Medicare or Medicaid benefits for the terminal illness. Once the
patient elects the benefit, the Medicare-certified hospice program assumes
responsibility for providing and paying for the care and treatment related to
the un-derlying illness for which hospice care was elected. The
Medicare-certified hospice is paid a predetermined dollar amount for each day
of hospice care each patient receives. Four levels of hospice care are covered
under Medicare and Medicaid hospice benefits:
•
Routine home care: All services provided are
included in the daily rate to the hospice.
•
Inpatient respite care: A 5-day inpatient stay,
provided on an occasional basis to relieve the family caregivers
•
Continuous care: Continuous nursing care provided
in the home for management of a medical crisis. Care reverts to the routine
home care level when the crisis is resolved. (For example, the patient develops
seizure activity and a nurse is placed in the home continuously to monitor the
patient and administer medications. After 72 hours the seizure activity is
under control, the family has been instructed how to care for the patient, and
the continuous nursing care is stopped.)
•
General inpatient care: Inpatient stay for symptom
man-agement that cannot be provided in the home; not subject to the guidelines
for a standard hospital inpatient stay.
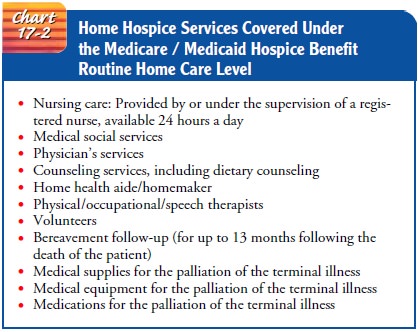
Most hospice care is provided at the “routine home care” level and
includes the services depicted in Chart 17-2. According to federal guidelines,
hospices may provide no more than 20% of the aggregate annual patient days at
the inpatient level. Patients may “revoke” their hospice benefits at any time,
resuming tradi-tional coverage under Medicare or Medicaid for the terminal
ill-ness. They may also re-elect their hospice benefits at a later time after
reassessment for eligibility according to these criteria
Related Topics