Chapter: Medical Surgical Nursing: End-of-Life Care
Psychosocial Issues - Nursing Care of the Terminally Ill Patient
PSYCHOSOCIAL
ISSUES
Nurses are responsible for educating patients about the possibil-ities
and probabilities inherent in their illness and their life with the illness,
and for supporting them as they conduct life review, values clarification,
treatment decision making, and end-of-life closure. The only way to do this
effectively is to try to appreciate and understand the illness from the
patient’s perspective.
Kübler-Ross’s (1969) work revealed that patients in the final stages of
life can and will talk openly about their experiences, ex-posing as a myth the
view that patients will be harmed by honest discussion with their caregivers
about death. Despite the contin-ued reluctance of health care providers to
engage in open discus-sion about end-of-life issues, studies have confirmed
that patients want information about their illness and end-of-life choices are
not harmed by open discussion about death (McSkimming, Super, Driever et al.,
1997; Virmani, Schneiderman & Kaplan, 1994).
At the same time, nurses need to be both culturally aware and sensitive
in their approaches to communication with patients and families about death.
Attitudes toward open disclosure about ter-minal illness vary widely among
different cultures, and direct com-munication to the patient about such matters
may be viewed as harmful (Blackhall, Murphy, Frank et al., 1995). To provide
ef-fective patient- and family-centered care at the end of life, nurses must be
willing to set aside their assumptions so that they can dis-cover what type and
amount of disclosure is most meaningful to each patient and family within their
unique belief systems.
The social and legal evolution of advance directive documents represents some progress in our willingness to both contemplate and communicate our wishes surrounding the end of life (Chart 17-3). Now legally sanctioned in every state and federally sanc-tioned through the Patient Self-Determination Act (PSDA) of 1990, advance directives are written documents that allow the in-dividual who is of sound mind to document his or her preferences regarding the use or nonuse of medical treatment at the end of life, specify the preferred setting for care, and communicate other valuable insights into his or her values and beliefs.
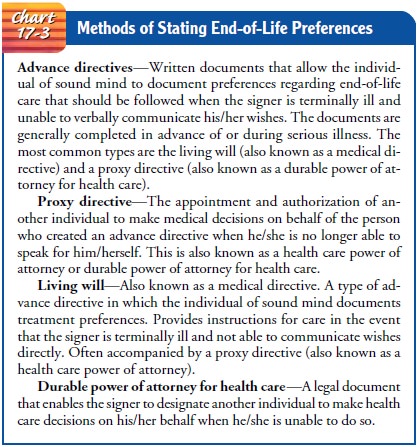
The addition of a proxy directive (the appointment and authorization of an-other
individual to make medical decisions on behalf of the per-son who created the
advance directive when he or she can no longer speak for himself or herself) is
an important addition to the “living will” or medical directive that specifies
the signer’s preferences. Although these documents are widely available from
health care providers, community organizations, bookstores, and the Internet,
their underuse reflects society’s continued discomfort with openly confronting
the subject of death. Further, the exis-tence of a properly executed advance
directive does not reduce the complexity of end-of-life decisions. The advance
directive should not be considered an adequate substitute for ongoing
communi-cation between health care provider, patient, and family as the end of
life approaches (Lynn, 1991).
Related Topics