Chapter: Medical Surgical Nursing: End-of-Life Care
Communication - Nursing Care of the Terminally Ill Patient
COMMUNICATION
As has been discussed, remarkable strides have been made in the ability
to prolong life, but attention to care for the dying lags be-hind (Callahan,
1993b). On one level, this comes as no surprise. Each of us will eventually
face death, and most would agree that one’s own demise is a subject he or she
would prefer not to con-template. Indeed, Glaser and Strauss (1965) noted that
unwill-ingness in our culture to talk about the process of dying is tied to our
discomfort with the notion of particular deaths—those of our patients’ and our
own—rather than talking about death in the ab-stract, which is more
comfortable. Finucane (1999) observed that our struggle to stay alive is a
prerequisite to being human. Con-fronting death in our patients uncovers our
own deeply rooted fears.
To develop a level of comfort and expertise in communicat-ing with
seriously and terminally ill patients and their families, nurses and other
clinicians need to first consider their own expe-riences with and values
concerning illness and death. Reflection, reading, and talking with family
members, friends, and colleagues can assist the nurse to examine beliefs about
death and dying. Talking with individuals from differing cultural backgrounds
canassist the nurse to view personally held beliefs through a different lens,
and can help to sensitize the nurse to death-related beliefs and practices in
other cultures. Discussion with nursing and non-nursing colleagues can also be
useful to reveal the values shared by many health care professions and identify
diversity in the val-ues of patients in their care. Values clarification and
personal death awareness exercises can provide a starting point for
self-discovery and discussion.
Skills for Communicating With the Seriously Ill
Nurses need to develop skill and comfort in assessing patients’ and
families’ responses to serious illness and planning interven-tions that will
support their values and choices throughout the continuum of care. Patients and
families need ongoing assistance: telling a patient something once is not
teaching, and hearing the patient’s words is not the same as active listening.
Throughout the course of a serious illness, patients and their families will
en-counter complicated treatment decisions, bad news about disease progression,
and recurring emotional responses. In addition to the time of initial
diagnosis, lack of response to the treatment course, decisions to continue or
withdraw particular interven-tions, and decisions about hospice care are
examples of critical points on the treatment continuum that demand patience,
em-pathy, and honesty from the nurse. Discussing sensitive issues such as
serious illness, hopes for survival, and fears associated with death is never easy.
However, the art of therapeutic communica-tion can be learned and, like other
skills, must be practiced to gain expertise. Similar to other skills,
communication should be prac-ticed in a “safe” setting, such as a classroom or
clinical skills lab-oratory with other students or clinicians.
Although communication
with each patient and family should be tailored to their level of understanding
and values concerning disclosure, general guidelines for the nurse include the
following (Addington, 1991):
· Deliver and interpret
the technical information necessary for making decisions without hiding behind
medical termi-nology.
· Realize that the best
time for the patient to talk may be when it is least convenient for you.
· Being fully present
during any opportunity for communi-cation is often the most helpful form of
communication.
· Allow the patient and
family to set the agenda regarding the depth of the conversation.
Nursing Interventions When the Patient and Family Receive Bad News
Communicating about a life-threatening diagnosis or about dis-ease
progression is best accomplished by the interdisciplinary team in any setting—a
physician, nurse, and social worker should be present whenever possible to
provide information, facilitate dis-cussion, and address concerns. Most
importantly, the presence of the team conveys caring and respect for the
patient and family. Creating the right setting is particularly important. If
the patient wishes to have family present for the discussion, arrangements
should be made to have the discussion at a time that is best for the patient
and family. A quiet area with a minimum of disturbances should be used. Each
clinician who is present should turn off beep-ers or other communication
devices for the duration of the meet-ing and should allow sufficient time for
the patient and family to absorb and respond to the news. Finally, the space in
which the meeting takes place should be conducive to seating all of the
par-ticipants at eye level. It is difficult enough for patients and fami-lies
to be the recipients of bad news without having an array of clinicians standing
uncomfortably over them at the foot of the pa-tient’s bed.
After an initial
discussion of a life-threatening illness or pro-gression of a disease, patients
and their families will have many questions and may need to be reminded of
factual information. Coping with news about a serious diagnosis or poor
prognosis is an ongoing process. The nurse needs to be sensitive to these
on-going needs and may need to repeat previously provided infor-mation or
simply be present while the patient and family react emotionally. The most
important intervention the nurse can pro-vide is listening empathetically.
Seriously ill patients and their families need time and support to cope with
the changes brought about by serious illness and the prospect of impending
death. The nurse who is able to sit comfortably with another’s suffering, time
and time again, without judgment and without the need to solve the patient’s
and family’s problems provides an intervention that is a gift beyond measure.
Keys to effective listening include the following:
· Resist the impulse to
fill the “empty space” in communica-tion with talk.
· Allow the patient and
family sufficient time to reflect and respond after asking a question.
· Prompt gently: “Do you
need more time to think about this?”
· Avoid distractions
(noise, interruptions).
· Avoid the impulse to
give advice.
· Avoid canned responses:
“I know just how you feel.”
· Ask questions.
· Assess
understanding—your own and the patient’s—by re-stating, summarizing, and
reviewing.
Responding With Sensitivity To Difficult Questions
Patients will often direct questions or concerns to nurses before they
have been able to fully discuss the details of their diagnosis and prognosis
with the physician or the entire health care team. Using open-ended questions
allows the nurse to elicit the pa-tient’s and family’s concerns, explore
misconceptions and needs for information, and form the basis for collaboration
with the physician and other team members. For example, the seriously ill
patient may ask the nurse, “Am I dying?” The nurse should avoid making
unhelpful responses that dismiss the patient’s real con-cerns or defer the
issue to another care provider. Nursing assess-ment and intervention are always
possible, even when a need for further discussion with the physician is clearly
indicated. When-ever possible, discussions in response to the patient’s
concerns should occur when the patient expresses a need, although it may be the
least convenient time for the nurse (Addington, 1991). Creating an
uninterrupted space of just 5 minutes can do much to identify the source of the
concern, allay anxieties, and plan for follow-up. For example, in response to
the question, “Am I dying?” the nurse could establish eye contact and follow
with a statement acknowledging the patient’s fears (“This must be very
difficult for you”) and an open-ended statement or question (“Tell me more
about what is on your mind.”). The nurse then needs to listen intently, ask
additional questions for clarification, and provide reassurance only when it is
realistic. In this example,
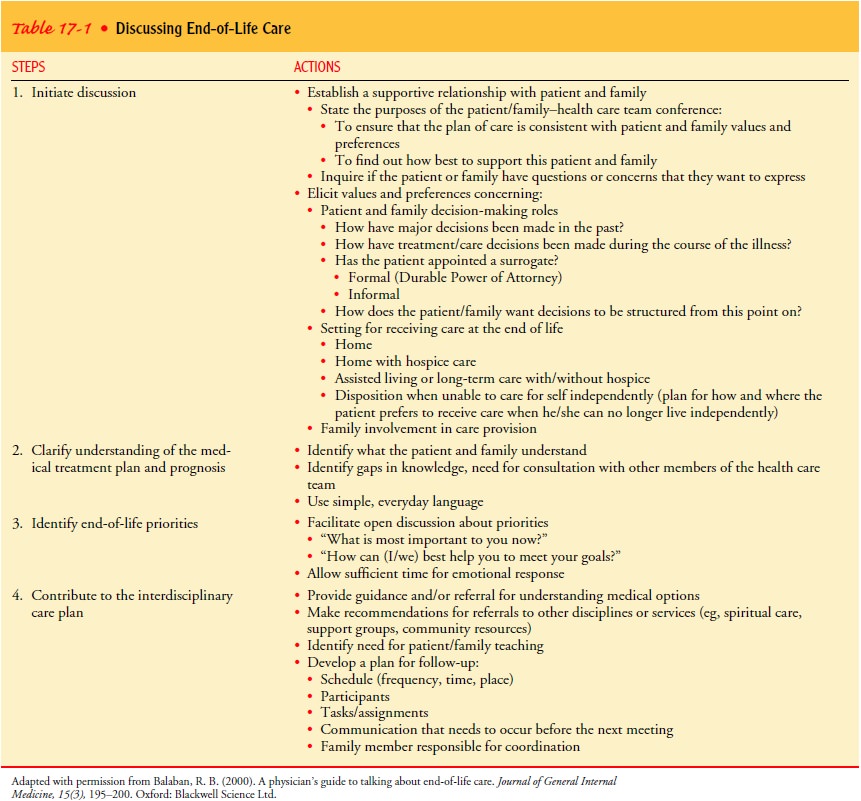
As
a member of the interdisciplinary team caring for the pa-tient at the end of
life, the nurse fills an important role in facili-tating the team’s
understanding of the patient’s values and preferences, the family dynamics
concerning decision making, and the patient’s and family’s response to
treatment and chang-ing health status. Many dilemmas in patient care at the end
of life are related to poor communication between team members and the patient
and family and failure of team members to commu-nicate effectively with each
other. Regardless of the care setting, the nurse can ensure a proactive
approach to the psychosocial care of the patient and family. Periodic,
structured assessments pro-vide an opportunity for all parties to consider
their priorities and plan for an uncertain future. The nurse can assist the
patient and family to clarify their values and preferences concerning
end-of-life care by using a structured approach. Sufficient time must be
devoted to each step, so that the patient and family have time to process new
information, formulate questions, and consider their options. The nurse may
need to plan several meetings to accom-plish the four steps described in Table
17-1.
Related Topics