Chapter: Medical Surgical Nursing: Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Rheumatic Endocarditis - Infectious Diseases of the Heart
Infectious Diseases of the Heart
Among
the most common infections of the heart are infective en-docarditis,
myocarditis, and pericarditis. The ideal management is prevention.
RHEUMATIC ENDOCARDITIS
Acute rheumatic fever, which occurs most often in school-age children, follows 0.3% to 3% of cases of group A beta-hemolytic streptococcal pharyngitis (Chin, 2001). Prompt treatment of strep throat with antibiotics can prevent the development of rheumatic fever (Chart 29-1). The Streptococcus is spread by direct contact with oral or respiratory secretions. Although the bacteria are the causative agents, malnutrition, overcrowding, and lower socioeconomic status may predispose individuals to rheumatic fever (Beers et al., 1999).
The incidence of rheumatic fever in the United States and other developed countries is believed to have steadily decreased, but the exact incidence is difficult to determine
because the infection may go unrecognized and patients may not seek treatment
(Braunwald et al., 2001; Beers et al., 1999). As many as 39% of patients with
rheumatic fever develop various degrees of rheumatic heart disease associated
with valvu-lar insufficiency, heart failure, and death (Chin, 2001). The
dis-ease also affects all bony joints, producing polyarthritis. The prevalence
of rheumatic heart disease is difficult to determine be-cause clinical
diagnostic criteria are not standardized and autop-sies are not routinely
performed. Except for rare outbreaks, the prevalence of rheumatic heart disease
in the United States is be-lieved to be less than 0.05 cases per 1000 people
(Chin, 2001). The number of U.S. citizens who die from rheumatic heart dis-ease
declined from approximately 15,000 in 1950 to about 4,000 in 2001 (AHA, 2001).
Pathophysiology
The
heart damage and the joint lesions of rheumatic endocardi-tis are not
infectious in the sense that these tissues are not invaded and directly damaged
by destructive organisms; rather, they rep-resent a sensitivity phenomenon or
reaction occurring in response to hemolytic streptococci. Leukocytes accumulate
in the affected tissues and form nodules, which eventually are replaced by scar
tis-sue. The myocardium is certain to be involved in this inflamma-tory
process; rheumatic myocarditis develops, which temporarily weakens the
contractile power of the heart. The pericardium also is affected, and rheumatic
pericarditis occurs during the acute illness. These myocardial and pericardial
complications usually occur without serious sequelae. Rheumatic endocarditis,
how-ever, results in permanent and often crippling side effects.
Clinical Manifestations
Rheumatic
endocarditis anatomically manifests first by tiny translucent vegetations or
growths, which resemble pinhead-sized beads arranged in a row along the free
margins of the valve flaps. These tiny beads look harmless enough and may
disappear with-out injuring the valve leaflets. More often, however, they have
serious effects. They are the starting point of a process that grad-ually
thickens the leaflets, rendering them shorter and thicker than normal and
preventing them from closing completely. The result is leakage, a condition
called valvular regurgitation. The
most common site of valvular regurgitation is the mitral valve. In some
patients, the inflamed margins of the valve leaflets become adherent, resulting
in valvular stenosis, a narrowed or stenotic valvular orifice. Regurgitation
and stenosis may occur in the same valve.
A
few patients with rheumatic fever become critically ill with intractable heart
failure, serious dysrhythmias, and pneumonia. These patients are treated in an
intensive care unit. Most patients recover quickly. However, although the
patient is free of symp-toms, certain permanent residual effects remain that
often lead to progressive valvular deformities. The extent of cardiac damage,
or even its existence, might not have been apparent in clinical ex-aminations
during the acute phase of the disease. Eventually, however, the heart murmurs
that are characteristic of valvular stenosis, regurgitation, or both become
audible on auscultation and, in some patients, even detectable as thrills on
palpation. Usually, the myocardium can compensate for these valvular de-fects
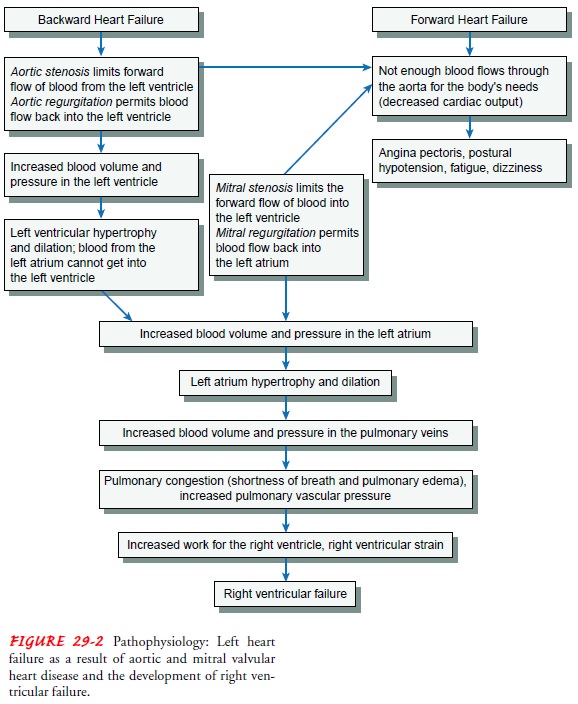
very well for a time. As long as the myocardium can com-pensate, the patient
remains in apparently good health. With continued valvular alterations, the
myocardium is unable to com-pensate (see Fig. 29-2), as evidenced by signs and
symptoms of heart failure.
Assessment and Diagnostic Findings
During
assessment, the nurse should keep in mind that the symp-toms depend on which
side of the heart is involved. The mitral valve is most often affected,
producing symptoms of left-sided heart failure: shortness of breath with
crackles and wheezes in the lungs. The severity of the symptoms depends on the
size and location of the lesion. The systemic symptoms that are pres-ent are
proportionate to the virulence of the invading organism. When a new murmur is
detected in a patient with a systemic in-fection, infectious endocarditis
should be suspected. The patient is also at risk for embolic phenomena of the lung
(eg, recurrent pneumonia, pulmonary abscesses), kidney (eg, hematuria, renal
failure), spleen (eg, left upper quadrant pain), heart (eg, myo-cardial
infarction), brain (eg, stroke), or peripheral vessels.
Prevention
Rheumatic
endocarditis is prevented through early and adequate treatment of streptococcal
infections. A first-line approach in preventing initial attacks of rheumatic
endocarditis is to recog-nize streptococcal infections, treat them adequately,
and control epidemics in the community. Every nurse should be familiar with the
signs and symptoms of streptococcal pharyngitis: high fever (38.9°C to 40°C [101°F to 104°F]),
chills, sore throat, redness of the throat with exudate, enlarged lymph nodes,
abdominal pain, and acute rhinitis.
Medical Management
The
objectives of medical management are to eradicate the causative organism and
prevent additional complications, such as a thromboembolic event. Long-term
antibiotic therapy is the recommended treatment, and penicillin administered
parenter-ally remains the medication of choice.
The
patient who has rheumatic endocarditis and whose valvu-lar dysfunction is mild
may require no further treatment. Never-theless, the danger exists for
recurrent attacks of acute rheumatic fever, bacterial endocarditis, embolism
from vegetations or mural thrombi in the heart, and eventual cardiac failure.
Nursing Management
A
key nursing role in rheumatic endocarditis is teaching patients about the
disease, its treatment, and the preventive steps needed to avoid potential
complications. After acute treatment with anti-biotics, patients need to learn
about the need to take prophylactic antibiotics before invasive procedures.
Related Topics