Chapter: Medical Surgical Nursing: Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Infective Endocarditis - Infectious Diseases of the Heart
INFECTIVE ENDOCARDITIS
Infective
endocarditis is an infection of the valves and endothe-lial surface of the
heart. Endocarditis usually develops in people with cardiac structural defects
(eg, valve disorders). Infective en-docarditis is more common in older people,
probably because of decreased immunologic response to infection and the
meta-bolic alterations associated with aging. There is a high incidence of
staphylococcal endocarditis among IV/injection drug users who most commonly
have infections of the right heart valves (Bayer et al., 1998; Braunwald,
2001).
The
incidence of infective endocarditis remained steady at about 4.2 cases per
100,000 patients in the years from 1950 to the mid-1980s (Braunwald et al.,
2001). The incidence then in-creased, partially attributed to increased
IV/injection drug abuse (Braunwald et al., 2001). In 1998, a total of 2212
deaths were attributed to infective endocarditis (American Heart Association,
2001). Invasive procedures, particularly those involving mucosal surfaces, can
cause a bacteremia. The bacteremia rarely lasts for more than 15 minutes
(Dajani et al., 1997). If a person has some anatomic cardiac defect, bacteremia
can cause bacterial endo-carditis (Dajani et al., 1997). The combination of the
invasive procedure, the particular bacteria introduced into the bloodstream,
and the cardiac defect may result in infective endocarditis.
Pathophysiology
Infective
endocarditis is most often caused by direct invasion of the endocardium by a
microbe (eg, streptococci, enterococci, pneumococci, staphylococci). The
infection usually causes de-formity of the valve leaflets, but it may affect
other cardiac structures such as the chordae tendineae. Other causative micro-organisms
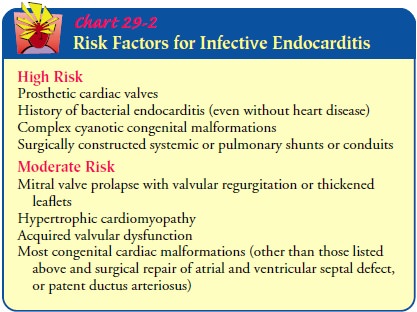
include fungi and rickettsiae. Patients at higher risk for infective
endocarditis are those with prosthetic heart valves, a his-tory of
endocarditis, complex cyanotic congenital malformations, and systemic or
pulmonary shunts or conduits that were surgically constructed (eg, saphenous
vein grafts, internal mammary artery grafts). At high risk are patients with
rheumatic heart disease or mitral valve prolapse and those who have prosthetic
heart valves (Chart 29-2).
Hospital-acquired endocarditis occurs most often in patients with debilitating disease, those with indwelling catheters, and those receiving prolonged intravenous or antibiotic therapy. Patients receiving immunosuppressive medications or cortico-steroids may develop fungal endocarditis.
A
diagnosis of acute infective endocarditis is made when the onset of infection
and resulting valvular destruction is rapid, oc-curring within days to weeks.
The onset of infection may take 2 weeks to months, diagnosed as subacute
infective endocarditis (Braunwald et al., 2001).
Clinical Manifestations
Usually,
the onset of infective endocarditis is insidious. The signs and symptoms
develop from the toxic effect of the infection, from destruction of the heart valves,
and from embolization of fragments of vegetative growths on the heart. The
occurrence of peripheral emboli is not experienced by patients with right heart
valve infective endocarditis (Bayer et al., 1998; Braunwald, 2001). The patient
exhibits signs and symptoms similar to those described in rheumatic
endocarditis (see previous discussion).
Assessment and Diagnostic Findings
The
general manifestations, which may be mistaken for influenza, include vague
complaints of malaise, anorexia, weight loss, cough, and back and joint pain.
Fever is intermittent and may be absent in patients who are receiving
antibiotics or corticosteroids or in those who are elderly or have heart
failure or renal failure. Splinter hemorrhages (ie, reddish-brown lines and streaks)
may be seen under the fingernails and toenails, and petechiae may appear in the
conjunctiva and mucous membranes. Small, painful nodules (Osler’s nodes) may be
present in the pads of fingers or toes. Hemorrhages with pale centers (Roth’s
spots) that may be seen in the fundi of the eyes are caused by emboli in the
nerve fiber layer of the eye.
The
cardiac manifestations include heart murmurs, which may be absent initially.
Progressive changes in murmurs over time may be encountered and indicate
valvular damage from veg-etations or perforation of the valve or the chordae
tendineae. Enlargement of the heart or evidence of heart failure is also found.
The
central nervous system manifestations include headache, temporary or transient
cerebral ischemia, and strokes, which may be caused by emboli to the cerebral
arteries. Embolization may be a presenting symptom; it may occur at any time
and may involve other organ systems. Embolic phenomena may occur, as discussed
in the previous section on rheumatic endocarditis.
Although
the described characteristics may indicate infective endocarditis, the signs
and symptoms may indicate other diseasesas well. A definitive diagnosis is made
when a microorganism is found in two separate blood cultures, in a vegetation,
or in an ab-scess. Three sets of blood cultures (with each set including one
aerobic and one anaerobic culture) should be obtained before ad-ministration of
any antimicrobial agents. Negative blood cultures do not totally rule out the
diagnosis of infective endocarditis. An echocardiogram may assist in the
diagnosis by demonstrating a moving mass on the valve, prosthetic valve, or
supporting struc-tures and by identification of vegetations, abscesses, new
pros-thetic valve dehiscence, or new regurgitation (Braunwald et al., 2001). An
echocardiogram may also demonstrate the develop-ment of heart failure.
Prevention
Although
rare, bacterial endocarditis may be life-threatening. A key strategy is primary
prevention in high-risk patients (ie, those with rheumatic heart disease,
mitral valve prolapse, or prosthetic heart valves). Antibiotic prophylaxis is
recommended for high-risk patients immediately before and sometimes after the
following procedures:
·
Dental procedures that induce
gingival or mucosal bleed-ing, including professional cleaning and placement of
orthodontic bands (not brackets)
·
Tonsillectomy or adenoidectomy
·
Surgical procedures that involve
intestinal or respiratory mucosa
·
Bronchoscopy with a rigid
bronchoscope
·
Sclerotherapy for esophageal varices
·
Esophageal dilation
·
Gallbladder surgery
·
Cystoscopy
·
Urethral dilation
·
Urethral catheterization if urinary
tract infection is present
·
Urinary tract surgery if urinary
tract infection is present
·
Prostatic surgery
·
Incision and drainage of infected
tissue
·
Vaginal hysterectomy
·
Vaginal delivery
The
type of antibiotic used for prophylaxis varies with the type of procedure and
the degree of risk. The patient is usually in-structed to take 2 g of
amoxicillin (Amoxil) 1 hour before dental, oral, respiratory, or esophageal
procedures. If the patient is aller-gic to penicillin (eg, ampicillin [Omnipen,
Polycillin], carbenicillin [Geocillin], cloxacillin [Cloxapen], methicillin
[Staphcillin], nafcillin [Nafcil, Unipen], oxacillin [Prostaphlin, Bactocill],
penicillin G [Bicillin, Permapen]), clindamycin (Cleocin), ceph-alexin
(Keflex), cefadroxil (Duricef), azithromycin (Zithromax), or clarithromycin
(Biaxin) may be used. Recommendations for gastrointestinal or genitourinary
procedures are ampicillin and gentamicin (Garamycin) for high-risk patients,
amoxicillin or am-picillin for moderate-risk patients, and substituting
vancomycin (Vancocin) only for patients allergic to ampicillin or amoxicillin.
The
severity of oral inflammation and infection is a significant factor in the
incidence and degree of bacteremia. Poor dental hy-giene can lead to
bacteremia, particularly in the setting of a den-tal procedure. Regular
personal and professional oral health care and rinsing with an antiseptic
mouthwash for 30 seconds before dental procedures may assist in reducing the
risk of bacteremia. Increased vigilance is also needed in patients with
intravenous catheters. To minimize the risk of infection, nurses must ensure
that meticulous hand hygiene, site preparation, and the use ofaseptic technique
occur during the insertion and maintenance procedures (Schmid, 2000). All
catheters are removed as soon as they are no longer needed or no longer
function.
Complications
Even
if the patient responds to the therapy, endocarditis can be destructive to the
heart and other organs. Heart failure and cerebral vascular complications, such
as stroke, may occur before, during, or after therapy. The development of heart
failure, which may re-sult from perforation of a valve leaflet, rupture of
chordae, blood flow obstruction due to vegetations, or intracardiac shunts from
dehiscence of prosthetic valves, indicates a poor prognosis with medical
therapy alone and a higher surgical risk (Braunwald et al., 2001). Valvular
stenosis or regurgitation, myocardial damage, and mycotic (fungal) aneurysms
are potential heart complications. Many other organ complications can result
from septic or non-septic emboli, immunologic responses, abscess of the spleen,
mycotic aneurysms, and hemodynamic deterioration.
Medical Management
The
causative organism may be identified by serial blood cultures. The objective of
treatment is to eradicate the invading organism through adequate doses of an
appropriate antimicrobial agent.
PHARMACOLOGIC THERAPY
Antibiotic
therapy is usually administered parenterally in a con-tinuous intravenous
infusion for 2 to 6 weeks. Parenteral therapy is administered in doses that
achieve a high serum concentration and for a significant duration to ensure
eradication of the dor-mant bacteria within the dense vegetations. This therapy
is often delivered in the patient’s home and is monitored by a home care nurse.
Serum levels of the selected antibiotic are monitored. If the serum does not
demonstrate bactericidal activity, increased dosages of the antibiotic are
prescribed, or a different antibiotic is used. Numerous antimicrobial regimens
are in use, but penicillin is usually the medication of choice. Blood cultures
are taken periodically to monitor the effect of therapy. In fungal endo-carditis,
an antifungal agent, such as amphotericin B (Abelect, Amphocin, Fungizone), is
the usual treatment.
The
patient’s temperature is monitored at regular intervals be-cause the course of
the fever is one indication of the effectiveness of treatment. However, febrile
reactions also may occur as a re-sult of medication. After adequate
antimicrobial therapy is ini-tiated, the infective organism usually disappears.
The patient should begin to feel better, regain an appetite, and have less
fa-tigue. During this time, patients require psychosocial support be-cause,
although they feel well, they may find themselves confined to the hospital or
home with restrictive intravenous therapy.
SURGICAL MANAGEMENT
After
the patient recovers from the infectious process, seriously damaged valves may
need to be replaced. Surgical valve replace-ment greatly improves the prognosis
for patients with severe symptoms from damaged heart valves. Aortic or mitral
valve ex-cision and replacement are required for patients who develop
congestive heart failure despite adequate medical treatment, pa-tients who have
more than one serious systemic embolic episode, and patients with uncontrolled
infection, recurrent infection, or fungal endocarditis. Many patients who have
prosthetic valve en-docarditis (ie, infected prostheses) require valve
replacement.
Nursing Management
The
nurse monitors the patient’s temperature; the patient may have fever for weeks.
Heart sounds are assessed; a new murmur may indicate involvement of the valve
leaflets. The nurse monitors for signs and symptoms of systemic embolization,
or for patients with right heart endocarditis, the nurse monitors for signs and
symptoms of pulmonary infarction and infiltrates. The nurse as-sesses signs and
symptoms of organ damage such as stroke (ie, cere-brovascular accident or brain
attack), meningitis, heart failure, myocardial infarction, glomerulonephritis,
and splenomegaly.
Patient
care is directed toward management of infection. The patient is started on
antibiotics as soon as blood cultures have been obtained. All invasive lines
and wounds should be assessed daily for redness, tenderness, warmth, swelling,
drainage, or other signs of infection. Patients and their families are
instructed about any activity restrictions, medications, and signs and symptoms
of infection. The nurse should instruct the patient and family about the need
for prophylactic antibiotics before, and possibly after, dental, respiratory,
gastrointestinal, or genitourinary procedures. Home care nurses supervise and
monitor intravenous antibiotic therapy delivered in the home setting and
educate the patient and family about prevention and health promotion. The nurse
pro-vides the patient and family with emotional support and facili-tates coping
strategies during the prolonged course of the infection and antibiotic
treatment required. If the patient received surgical treatment, the nurse
provides postoperative care and instruction.
Related Topics