Chapter: Medicine and surgery: Principles and practice of medicine and surgery
Pyrexia of unknown origin (PUO) - Infections
Pyrexia of unknown origin (PUO)
Definition
An intermittent or continuous fever >38˚C lasting more than 3 weeks and without diagnosis despite initial investigations.
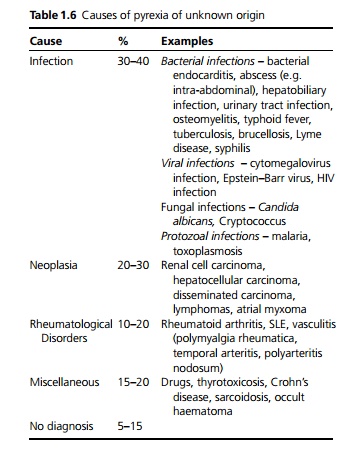
Aetiology
See Table 1.6.
Clinical features
A careful history, including systematic review is essential.
· Pattern and duration of fever (although the correlation between fever patterns and specific diseases is weak), weight loss, night sweats, headaches, rashes and any other symptoms.
· Previous illnesses including operations and psychiatric illnesses.
· Specific factors including family history, immunisation status, occupational history, travel history, history of consumption of unusual foods (e.g. unpasteurised milk), drug history (including over-the-counter medications, homeopathic preparations, drugs of abuse), sexual history, infectious contacts and animal contacts (including possible exposure to ticks and other vectors).
A full systematic examination is required including the following:
· Documentation of pattern and duration of fever.
· Specific features include rashes, lymphadenopathy, genitoperitoneal lesions, organomegaly, new or changing cardiac murmurs, signs of arthritis, abdominal tenderness or rigidity and a neurological evaluation including fundoscopy.
Investigations
1. Initial investigations: close monitoring of temperature; chest X-ray; urine for urinalysis, microscopy, culture and sensitivity; full blood count and peripheral blood film; repeated blood cultures taken at times of fever; culture of wounds, intravenous lines and other relevant sites, e.g. CSF; urea, creatinine, electrolytes and blood sugar; creatine kinase and liver function tests; C-reactive protein, ESR and immunoglobulins.
2. Specific blood tests and microbiology may be required for certain indications:
· Malarial exposure: Repeated thick and thin blood films, antigen testing.
· Intravenous drug use or at risk: Hepatitis serology, HIV testing.
· Suspected thyrotoxicosis: Thyroid function testing. Suspected rheumatological disorder: ANA, anti-
· DNA antibody, ANCA.
· Specific agent suspected: Serial titres for EBV, CMV, influenza, Toxoplasma, Lyme disease, chlamydia, salmonella, Borrelia recurrentis, Q fever, leptospirosis.
3. Other procedures that may also be considered are
· abdominal ultrasound for intra-hepatic, sub-phrenic or paracolic abscesses.
· white cell scan for demonstration of an abscess, empyema or osteomyelitis.
· bone scan for osteomyelitis or metastatic bone disease.
· CT and MRI for lymphoma, tumours or abscesses. transoesophageal echocardiography for infective
· endocarditis or atrial myxoma.
· bone marrow biopsy for leukaemia or culture for miliary TB.
· biopsy either endoscopically or percutaneously of suspected area.
Management
Blind treatment should be avoided unless the patient is septicaemic or deteriorating. In such cases a best guess of the cause and hence the antibiotic cover has to be made depending on the results of history, examination and investigations available. It is essential to continue regular reassessment for new symptoms or signs and to stop all other drugs wherever possible.
Related Topics