Chapter: Medicine and surgery: Principles and practice of medicine and surgery
Hypercalcaemia - Fluid and electrolyte balance
Hypercalcaemia
Definition
A serum calcium level of >2.6 mmol/L.
Incidence
Relatively common.
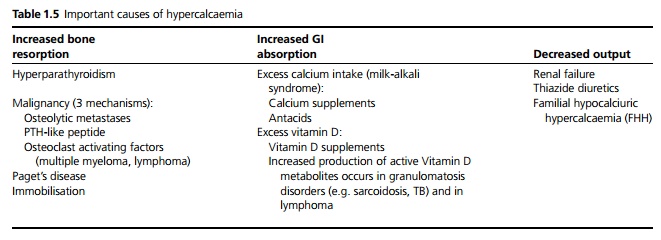
Aetiology
Important causes of hypercalcaemia are given in Table 1.5. More than 80% of cases are due to malignancy or primary hyperparathyroidism.
Pathophysiology
Hypercalcaemia prevents membrane depolarisation leading to central nervous system effects, decreased muscle power and reduced gut mobility. It also has multiple effects on the kidney: it reduces the glomerular filtration rate; it can cause acute or chronic renal failure; it can also cause nephrogenic diabetes insipidus, urinary stones and calcium deposition in the kidney and other tissues. Hypercalcaemia causes shortening of the Q–T interval but this is not associated with an increased risk of cardiac arrhythmias.
Clinical features
The condition may be asymptomatic and diagnosed incidentally on calcium measurement. Early symptoms are often insidious, including loss of appetite, fatigue, lethargy, weakness, constipation and thirst. The symptoms of hypercalcaemia can be summarised as bones, stones, moans and groans:
· Bone pain may be due to metastases, multiple myeloma or bone disease as a complication of hyperparathyroidism.
· Urinary stones.
· Moans due to confusion and drowsiness. Depression and acute psychosis can also occur.
· Groans due to abdominal symptoms such as nausea, vomiting, pain and constipation.
Deposition of calcium in heart valves, coronary arteries and other blood vessels may occur. Hypertension is relatively common, possibly due to renal impairment and also related to calcium-induced vasocon-striction.
Investigations
These are aimed at assessing the severity of hypercalcaemia to guide management and to look for the underlying cause. The serum calcium should be checked and corrected for serum albumin because only the ionised calcium (not bound to protein) is active. The total serum calcium is corrected as follows:
Corrected calcium = Measured calcium + 0.02(40 − serum albumin)
· Mild hypercalcaemia (2.6–2.8 mmol/L) is suggestive of primary hyperparathyroidism.
· Moderate to severe hypercalcaemia is more commonly due to malignancy.
Blood should be sent for U&Es (to look for renal impairment), serum protein electrophoresis and Bence Jones protein (to look for myeloma) and a PTH (parathyroid hormone) level. If the PTH level is normal or high, this is diagnostic of hyperparathyroidism because it should be suppressed in hypercalcaemia. A chest X-ray may demonstrate malignancy or sarcoidosis. Serum phosphate may be helpful, as it tends to be low in malignancy or primary hyperparathyroidism but high in other causes. If PTH is low, PTH-like peptide can be measured.
Other tests which may be useful include the following:
· Urinary calcium, which is raised in most causes of hypercalcaemia, but relatively low (<100 mg or 2.5 mmol/day) in milk–alkali syndrome, thiazide di-uretic use and FHH.
· Vitamin D and its active metabolites.
· Serum angiotensin converting enzyme (ACE), which may be raised in pulmonary sarcoidosis.
Management
This depends on the severity, whether acute or chronic and the underlying cause. Any causative drugs should be withdrawn.
· Patients should be assessed for fluid status and any dehydration corrected. Rehydration reduces calcium levels by a dilutional effect and by increasing renal clearance. Intravenous saline is often needed because many patients feel too nauseous to tolerate sufficient oral fluids and polyuria is common due to nephrogenic diabetes insipidus.
· Loop diuretics such as furosemide can be used in conjunction with fluids to increase renal excretion of calcium and prevent fluid overload.
· Bisphosphonates can be used, which inhibit bone turnover and therefore reduce serum calcium. Steroids may be used if the underlying diagnosis is a known malignancy, but is less useful if there is ectopic PTH production.
· If there is renal failure, early consultation with a nephrologist is needed, as increased renal excretion of calcium is often impossible or difficult to achieve and dialysis may be required.
· Further management depends on the underlying cause.
Related Topics