Chapter: Medicine and surgery: Principles and practice of medicine and surgery
Intravenous fluids - Fluid and electrolyte balance
Intravenous fluids
Intravenous fluids may be necessary for rapid fluid replacement, e.g. in
a shocked patient, or for maintenance in patients who are unable to eat and
drink or who are unable to maintain adequate intake in the face of large
losses, e.g. due to diarrhoea. When prescribing intravenous fluids certain
points should be remembered:
·
Are intravenous fluids the best
form of fluid replacement? If possible, oral fluids are preferable or if
swal-low is impaired consider nasogastric administration, which has the
advantage of allowing nasogastric feed to be given to provide nutrition.
·
Which intravenous fluid should be
given? Ideally this should be the one that matches any fluid and electrolyte
deficit or losses most closely. For example, blood loss should be replaced with
a blood transfusion and salt and water loss (e.g. vomiting, diarrhoea) with
normal saline. Additional potassium replacement is often needed in bowel
obstruction, but may be dangerous in renal failure.
·
In calculating the volume
required for maintenance check if is there increased insensible loss, e.g. due
to sweating in pyrexial patients, or are there other fluids being administered
which need to be taken into account? For example, some patients are on
intravenous drugs or intravenous nutritional supplements (total parenteral
nutrition).
·
Patients at risk of cardiac
failure (elderly, cardiac disease, liver or renal impairment) require special
caution as they are more prone to develop fluid overload.
There is no universally applicable fluid regimen. The choice of fluid
given and the rate of administration depend on the patient, any continued
losses and all patients must have continued assessment of their fluid balance
using fluid balance charts, observations and clinical examination as well as
monitoring of serum electrolytes by serial blood tests.
Fluid preparations: Intravenous fluid has to be isotonic to lysis of red blood cells. The
administration of water alone would lead to water moving across cell membranes
by osmosis, such that the cells would swell up and burst. Giving hypertonic
fluid is equally dangerous, as it causes water to move out of cells.
·
Most intravenous fluids used are
crystalloids (saline, dextrose, combined dextrose/saline, Hartmann’s solution).
It should be remembered that dextrose is rapidly metabolised by the liver;
hence giving dextrose solution is the equivalent of giving water to the
extra-cellular fluid compartment. If insufficient sodium is given in
conjunction, or the kidneys do not excrete the free water, hyponatraemia
results. This is a common problem, often because of inappropriate use of
dextrose or dextrosaline and because stress from trauma or surgery as well as
diseases such as cardiac failure promote antidiuretic hormone (ADH) release.
This leads to a mild form of syndrome of inappropriate antidiuretic hormone
(SIADH;) where there is water retention by the kidneys with resulting
hyponatraemia.
·
Colloids (albumin, dextran or
gelatin-based fluids) contain high-molecular-weight components that tend to be
retained in the intravascular compartment. This increases the colloid osmotic
pressure (oncotic pressure) of the circulation and draws fluid back into the
vascular compartment from the extracellular space. A smaller volume of colloid
compared to crystalloid is needed to have the same haemodynamic effect.
Theoretically they are of benefit for rapid expansion of the intravascular
compartment; however, they have anti-coagulant, antiplatelet and fibrinolytic
effects, which may be undesirable. There has been no consistent demonstrable
benefit of using colloid over crystalloid in most circumstances. In addition,
the use of albumin solution in hypoalbuminaemic patients (which seems logical)
has been associated with increased pulmonary oedema, possibly due to rapid
haemodynamic changes or capillary leakage of albumin.
Fluid regimens: These should consist of maintenance
fluids (which covers normal urinary, stool and insensible losses) and
replacement fluids for additional losses and to correct any pre-existing
dehydration. Fluid regimens must also take into account that patients of
differing
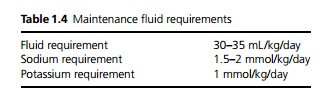
weight have different fluid and electrolyte requirements (see Table
1.4). Potassium is added to intravenous fluids in patients who are not being
fed, although this should be done with care. Both hypokalaemia and
hyper-kalaemia are potentially
life-threatening and serum potassium must be checked daily in patients who are
given potassium replacement. Patients with acute or chronic renal failure
should not have potassium added routinely to fluid replacement (although
hypokalaemia should of course be treated). Rapid administration of potassium is
dangerous, so even in hypokalaemia no more than 10 mmol/h is recommended
(except in severe hypokalaemia within an intensive care setting) and the
potassium must be uniformly mixed in the bag.
A typical daily maintenance regime for a 70 kg man with normal cardiac
and renal function consists of 8 hourly bags of:
·
1 L of 0.9% saline with 20 mmol
KCl added,
·
1 L of 5% dextrose with 20 mmol
KCl added and
·
1 L of 5% dextrose with 20 mmol
KCl added.
In general, dextrosaline is not suitable for maintenance, as it provides
insufficient sodium and tends to cause hyponatraemia. Postoperative patients
are also more prone to hyponatraemia due to mild SIADH, so may require
proportionally more sodium, e.g. 2 L of 0.9% saline to 1 L of 5% dextrose.
Replacement fluids generally need to be 0.9% saline, as losses tend to have a
high sodium concentration, e.g. drain fluid, blood, vomitus and diarrhoea.
Fluids should not be prescribed without taking into account the
patient’s current fluid balance, continued losses and underlying coexistent
diseases. It should also be remembered that intravenous fluids do not provide
any significant nutrition.
Related Topics