Chapter: Medicine and surgery: Respiratory system
Pneumonia - Respiratory infections
Pneumonia
Definition
Pneumonia is an infective, inflammatory disease of the lung parenchyma.
Aetiology
It is useful to classify pneumonia according to the causative organism or the clinical setting, e.g. community-acquired or nosocomial (hospital-acquired), immunosuppressed. This helps to determine the choice of antibiotics for treatment.
Pneumonia most often occurs in children and the elderly, but may also affect young, fit adults. The following risk factors increase the likelihood of pneumonia and also influence the likely organism:
· Cigarette smoking and underlying lung disease.
· Stroke or other neuromuscular disorder (aspiration pneumonia often by anaerobes).
· Immunosuppression and AIDS in particular P. jirovecii.
· Intravenous drug abusers. Alcoholics and vagrants.
· Hospital patients (more often Gram-negative organisms).
Viral pneumonia is less common, but bacterial pneumonia may be a secondary complication.
Pathophysiology
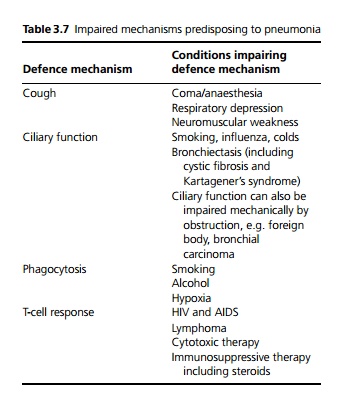
The infection may be as a result of impairment of one or more normal defence mechanisms (see Table 3.7)
Pulmonary oedema also predisposes to infection by acting as a growth medium. Pathologically pneumonia can be divided into broncho-, lobar or atypical pneumonia depending on the pattern of inflammation.
· Bronchopneumonia is most commonly seen at extremes of age. It is predisposed to by immobility and viral infections which lead to retention of secretions especially in the lower lobes. The infection is centred on the bronchi and bronchioles and spreads to involve adjacent alveoli, which become consolidated with an acute inflammatory exudate. Common causes include Strep. pneumoniae, M. catarrhalis or H. influenzae.
· Lobar pneumonia is seen most commonly in adults who may otherwise be healthy, but particularly va grants and alcoholics. Organisms spread rapidly through the alveolar spaces to involve the whole segment, lobe or lung. Ninety per cent of cases in healthy adults are caused by Strep. pneumoniae, many of the remaining cases are due to Klebsiella. Males are affected more often than females.
· Atypical pneumonias cause predominantly interstitial inflammation in the lung, clinically are less abrupt in onset and slower to resolve. Causes include the atypical bacteria Chlamydia, Coxiella, Mycoplasma and Le-gionella.
Clinical features
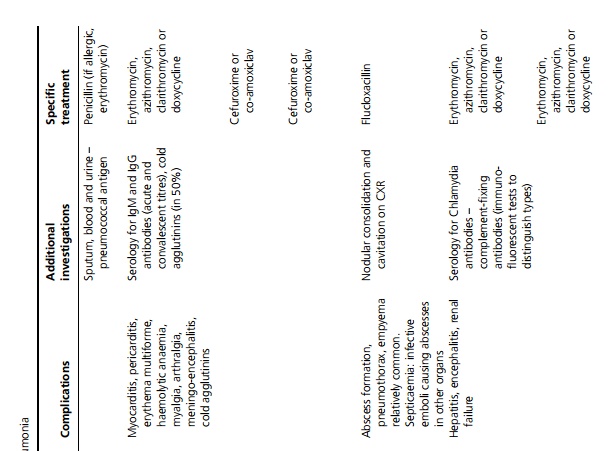
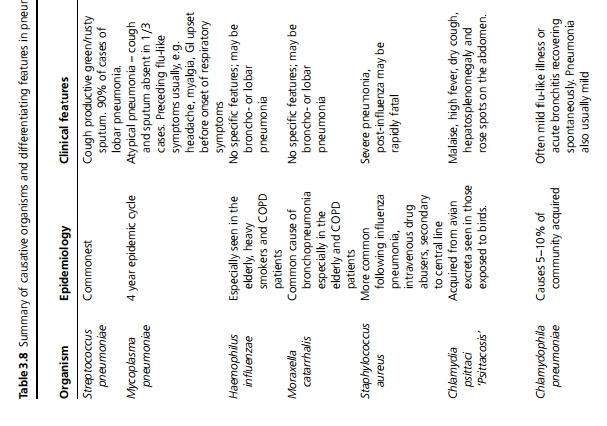
Symptoms may include fever, dyspnoea, pleuritic pain and cough often productive of green sputum; however, at extremes of age the presentation may be non-specific. On examination, classically there are signs of consolidation (such as dullness to percussion, increased vocal resonance, bronchial breathing) but even if frank consolidation is not present, most patients have tachypnoea (>20 breaths/minute) and crackles. In atypical pneumonia the signs of consolidation in the lung are often minor or absent, despite severe symptoms. Specific features, investigations and management of different types of pneumonia are summarised in Table 3.8 .
Macroscopy/microscopy
Bronchopneumonia: The affected areas of the lung are consolidated. The air spaces are filled with an acute inflammatory exudate causing the lung to be firm and a dark red or grey colour. The bronchi are inflamed and pleural involvement is common.
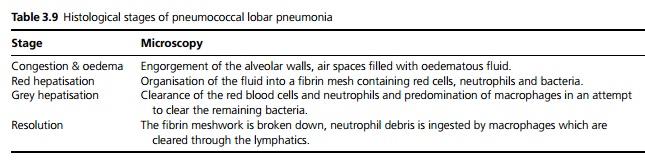
Lobar pneumonia: The affected lobe is consolidated with the acute inflammatory exudate being contained in a single segment, lobe or lung. Several identifiable stages are seen in a pneumococcal lobar pneumonia (see Table 3.9):
Complications
Development of lung abscesses and pleural effusion (which may be reactive or infected, i.e. an empyema), pleural infection (pleurisy) and septicaemia.
Investigations
A chest X-ray will demonstrate areas of consolidation, any abscesses, effusions and masses (such as under-lying bronchial carcinoma). X-ray changes generally lag behind clinical features so the X-ray may occasionally be normal at presentation, and may remain abnormal for several weeks after the pneumonia has resolved.
The white cell count will normally demonstrate a neutrophilia. If patients require admission, sputum and blood cultures should be taken and specific serological tests are available for Legionella and other atypical pneumonias.
Urea and electrolytes are measured for hydration and to detect any co-existing renal disease.
Blood gases may be required to monitor oxygenation and to assess for respiratory failure.
In severe cases, immunosuppressed individuals and those unresponsive to standard therapy, broncho scopy and bronchial lavage may be considered, as this is more likely to give microbiological results.
Patients should have a followup chest X-ray after 6 weeks to ensure resolution, and to exclude any underlying lesion such as carcinoma causing obstruction.
Management
· Non-pharmacological: Fluids, physiotherapy to clear secretions, analgesia for pleuritic pain where necessary and oxygen if there is hypoxia (guided by arterial blood gases).
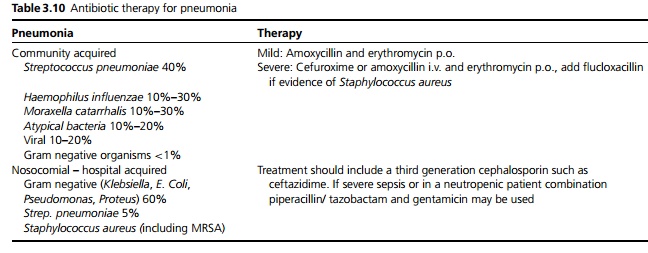
· Empirical antibiotic treatment should be commenced immediately based on knowledge of the likely organisms, modified where necessary by local microbiology guidelines and on the basis of culture results (see Table 3.10).
· Patients with sickle cell disease, asplenia or severe dysfunction of the spleen, chronic renal disease or nephrotic syndrome, coeliac disease, immunodeficiency or immunosuppression, haematological malignancy, cardiovascular disease, chronic pulmonary disease, chronic liver disease or diabetes mellitus should receive pneumovax prophylaxis.
Prognosis
Outcome depends greatly on the age of the patient and concurrent disease (including diabetes mellitus, chronic renal failure, congestive heart failure and underlying respiratory disease such as chronic obstructive pulmonary disease). Mortality for community-acquired pneumonia is about 14% (about 20% for those requiring hospital admission and up to 35% for those requiring intensive care).
British Thoracic Society guideline for identifying patients with severe community acquired pneumonia:
Core features (score 1 for each): Confusion, urea ≥ 7 mmol/L, respiratory rate ≥ 30 breaths per minute,
low blood pressure (systolic <90 mmHg or diastolic ≤60 mmHg).
Additional adverse features include: Age ≥ 50 years, coexisting chronic disease, hypoxia (PaO2 < 8 kPa or oxygen saturation < 92%), bilateral or multilobe involvement on chest X-ray.
A score of 2 or more core features suggest a severe pneumonia with indication for initial combined antibiotic therapy.
Related Topics