Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Streptococci and Enterococci
Pneumococcal Disease : Clinical Aspects
PNEUMOCOCCAL DISEASE : CLINICAL ASPECTS
MANIFESTATIONS
Pneumococcal Pneumonia
Clinically, pneumococcal pneumonia begins abruptly with a shaking chill and high fever. Cough with production of sputum pink to rusty in color (indicating the presence of RBCs) and pleuritic chest pain are common. Physical findings usually indicate pulmonary consolidation. Children and young adults typically demonstrate a lobular or lobar consoli-dation on chest radiography, whereas older patients may show a less localized bronchial distribution of the infiltrates. Without therapy, sustained fever, pleuritic pain, and produc-tive cough continue until a “crisis” occurs 5 to 10 days after onset of the disease. The cri-sis involves a sudden decrease in temperature and improvement in the patient’s condition. It is associated with effective levels of opsonizing antibody reaching the lesion. Although infection may occur at any age, the incidence and mortality of pneumococcal pneumonia increase sharply after 50 years.
Pneumococcal Meningitis
S. pneumoniae is one of the three leading causes of bacterial meningitis. The signs andsymptoms are similar to those produced by other bacteria . Acute puru-lent meningitis may follow pneumococcal pneumonia, infection at another site, or appear with no apparent antecedent infection. It may also develop after trauma involving the skull. The mortality and frequency of sequelae are slightly higher with pneumococcal meningitis than with other forms of pyogenic meningitis.
Other Infections
Pneumococci are common causes of sinusitis and otitis media . The latter frequently occurs in children in association with viral infection. Chronic infection of the mastoid or respiratory sinus sometimes extends to the subarachnoid space to cause meningitis. Pneumococci may also cause endocarditis, arthritis, and peritonitis, usually in association with bacteremia. Patients with ascites caused by diseases such as cirrhosis and nephritis may develop spontaneous pneumococcal peritonitis. Pneumococci do not cause pharyngitis or tonsillitis.
DIAGNOSIS
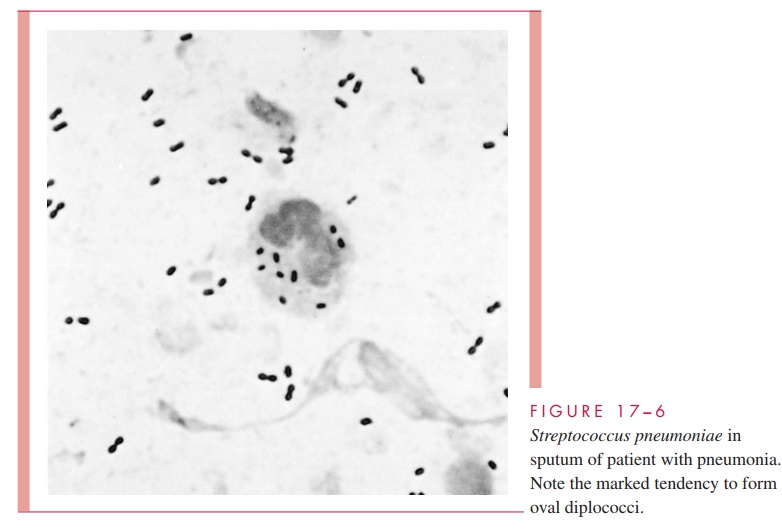
Gram smears of material from sputum and other sites of pneumococcal infection typically show Gram-positive, lancet-shaped diplococci (see Fig 17 – 6). Sputum collection may be difficult, however, and specimens contaminated with respiratory flora are useless for diag-nosis. Other types of lower respiratory specimens may be needed for diagnosis.
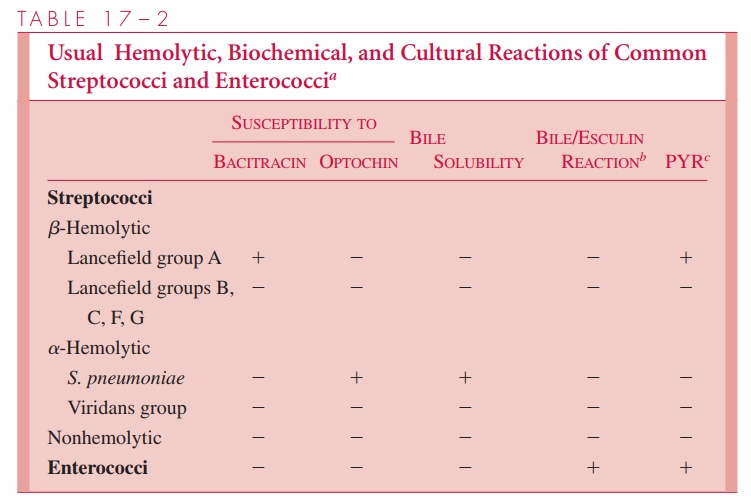
S. pneumoniae grows well overnight on blood agar medium and is usually distin-guished from viridans streptococci by susceptibility to the synthetic chemical ethylhy-drocupreine (Optochin) or by a bile solubility (see Table 17 – 2). Bacteremia is common in pneumococcal pneumonia and meningitis, and blood cultures are valuable supplements to cultures of local fluids or exudates. Detection of pneumococcal capsular antigen in body fluids is possible but valuable primarily when cultures are negative.
TREATMENT
For decades pneumococci were uniformly susceptible to penicillin at concentrations below 0.1 g/mL. In the late 1960s, this began to change, and strains with decreased sus-ceptibility to all β-lactams began to emerge. These strains have penicillin minimal inhibitory concentrations (MICs) of 0.12 to 8.0 g/mL and are associated with treatment failures in cases of pneumonia and meningitis. The resistance is not absolute and can be overcome with increased dosage depending on the MIC. The mechanism involves alter-ations in the -lactam target, the transpeptidases that cross-link peptidoglycan in cell wall synthesis. Resistant strains have mutations in one or more of these transpeptidases, which cause decreased affinity for penicillin and other β-lactams. Penicillinase is not produced. Resistance to erythromycin is uncommon but more likely with penicillin-resistant strains.
Penicillin is still the antimicrobic of choice for susceptible strains but resistance rates now exceed 10% in most locales and may be greater than 30% in some areas. Penicillin-resistant strains may be treated with erythromycin, vancomycin, or quinolones, if suscep-tible. Despite the -lactam cross resistance, high doses of third-generation cephalosporins have also been used in situations such as meningitis, where their added spectrum may be an advantage. The therapeutic response to treatment of pneumococcal pneumonia is often (but not always) dramatic. Reduction in fever, respiratory rate, and cough can occur in 12 to 24 hours but may occur gradually over several days. Chest radiography may yield nor-mal results only after several weeks.
PREVENTION
A vaccine prepared from capsular polysaccharide extracted from the 23 most common serotypes of S. pneumoniae is available. This vaccine is presently recommended for pa-tients who are particularly susceptible to pneumococcal infection because of advanced age, underlying disease, or immune status. As with other polysaccharide vaccines it is poorly immunogenic in infants. The newest vaccines follow the success of Haemophilusinfluenzae type b by conjugating the polysaccharide to protein in orderto stimulate T-cell dependent responses. This task is greatly complicated by the multiple serotype-specific polysaccharides involved in S. pneumoniae disease. A seven-valent con-jugate vaccine is now available and recommended for use beginning at 2 months of age. The polysaccharide continues to be recommended beyond the age of 5 years.
Related Topics