Chapter: Medical Surgical Nursing: Homeostasis, Stress, and Adaptation
Physiologic Response to Stress
PHYSIOLOGIC
RESPONSE TO STRESS
The physiologic response
to a stressor, whether it is a physical stressor or a psychological stressor,
is a protective and adaptive mechanism to maintain the homeostatic balance of
the body. The stress response is a “cascade of neural and hormonal events that
have short- and long-lasting consequences for both brain and body . . .; a
stressor is an event that challenges homeostasis, with a disease outcome being
looked upon as a failure of the normal process of adaptation to the stress”.
The General Adaptation Syndrome
Hans Selye developed a
theory of adaptation that profoundly influenced the scientific study of stress.
In 1936, Selye, experi-menting with animals, first described a syndrome
consisting of en-largement of the adrenal cortex; shrinkage of the thymus,
spleen, lymph nodes, and other lymphatic structures; and the appearance of
deep, bleeding ulcers in the stomach and duodenum. He iden-tified this as a
nonspecific response to diverse, noxious stimuli. From this beginning, he
developed a theory of adaptation to bio-logic stress that he named the general
adaptation syndrome.
PHASES OF THE GENERAL ADAPTATION SYNDROME
The general adaptation
syndrome has three phases: alarm, resis-tance, and exhaustion. During the alarm
phase, the sympathetic “fight-or-flight” response is activated with release of catechol-amines and the onset of the adrenocorticotropic hormone (ACTH)–adrenal
cortical response. The alarm reaction is defen-sive and anti-inflammatory but
self-limited. Because living in a continuous state of alarm would result in
death, the person moves into the second stage, resistance. During this stage,
adaptation to the noxious stressor occurs, and cortisol activity is still
increased. If exposure to the stressor is prolonged, exhaustion sets in and
en-docrine activity increases. This produces deleterious effects on the body
systems (especially the circulatory, digestive, and immune systems) that can
lead to death. Stages one and two of this syn-drome are repeated, in different
degrees, throughout life as the person encounters stressors.
Selye compared the
general adaptation syndrome with the life process. During childhood, there are
too few encounters with stress to promote the development of adaptive
functioning, and the child is vulnerable. During adulthood, the person
encounters a number of life’s stressful events and develops a resistance or
adap-tation. During the later years, the accumulation of life’s stressors and
the wear and tear on the organism again deplete the person’s ability to adapt,
resistance falls, and eventually death occurs.
LOCAL ADAPTATION SYNDROME
According to Selye’s
theory, a local adaptation syndrome also oc-curs.This syndrome includes the
inflammatory response and re-pair processes that occur at the local site of
tissue injury. The local adaptation syndrome occurs in small, topical injuries,
such as contact dermatitis. If the local injury is severe enough, the gen-eral
adaptation syndrome is activated as well.
Selye emphasized that
stress is the nonspecific response com-mon to all stressors, regardless of
whether they are physiologic, psychological, or social. The many conditioning
factors in each person’s environment account for why different demands are
in-terpreted by different people as stressors. Conditioning factors also
account for differences in the tolerance of different people for stress: some
people may develop diseases of adaptation, such as hypertension and migraine
headaches, while others are unaffected.
Interpretation of Stressful Stimuli by the Brain
Physiologic responses to
stress are mediated by the brain through a complex network of chemical and
electrical messages. The neural and hormonal actions that maintain homeostatic
balance are integrated by the hypothalamus, which is located in the cen-ter of
the brain, surrounded by the limbic system and the cerebral hemispheres. The
hypothalamus integrates autonomic nervous system mechanisms that maintain the
chemical constancy of the internal environment of the body. Together with the
limbic sys-tem, it also regulates emotions and many visceral behaviors
nec-essary for survival (eg, eating, drinking, temperature control,
reproduction, defense, aggression). The hypothalamus is made up of a number of
nuclei; the limbic system contains the amyg-dala, hippocampus, and septal
nuclei, along with other structures.
Literature supports the
concept that each of these structures responds differently to stimuli, and each
has its own characteris-tic response (Watkins, 1997). The cerebral hemispheres
are con-cerned with cognitive functions: thought processes, learning, and
memory. The limbic system has connections with both the cere-bral hemispheres
and the brain stem. In addition, the reticular ac-tivating system, which is a
network of cells that forms a two-way communication system, extends from the
brain stem into the midbrain and limbic system. This network controls the alert
or waking state of the body.
In the stress response,
afferent impulses are carried from sen-sory organs (eye, ear, nose, skin) and
internal sensors (barorecep-tors, chemoreceptors) to nerve centers in the
brain. The response to the perception of stress is integrated in the hypothalamus,which
coordinates the adjustments necessary to return to homeo-static balance. The
degree and duration of the response varies; major stress evokes both
sympathetic and pituitary adrenal responses.
Neural and
neuroendocrine pathways under the control of the hypothalamus are also
activated in the stress response. First, there is a sympathetic nervous system
discharge, followed by a sympathetic-adrenal-medullary discharge. If the stress
persists, the hypothalamic-pituitary system is activated (Fig. 6-2).
SYMPATHETIC NERVOUS SYSTEM RESPONSE
The sympathetic nervous
system response is rapid and short-lived. Norepinephrine is released at nerve
endings that are in di-rect contact with their respective end organs to cause
an increase in function of the vital organs and a state of general body
arousal. The heart rate is increased and peripheral vasoconstriction oc-curs, raising the blood pressure. Blood is also
shunted away from abdominal organs. The purpose of these activities is to
provide better perfusion of vital organs (brain, heart, skeletal muscles)Blood
glucose is increased, supplying more readily available en-ergy. The pupils are
dilated, and mental activity is increased; a greater sense of awareness exists.
Constriction of the blood ves-sels of the skin limits bleeding in the event of
trauma. The per-son is likely to experience cold feet, clammy skin and hands,
chills, palpitations, and a knot in the stomach. Typically, the per-son appears
tense, with the muscles of the neck, upper back, and shoulders tightened;
respirations may be rapid and shallow, with the diaphragm tense.
SYMPATHETIC-ADRENAL-MEDULLARY RESPONSE
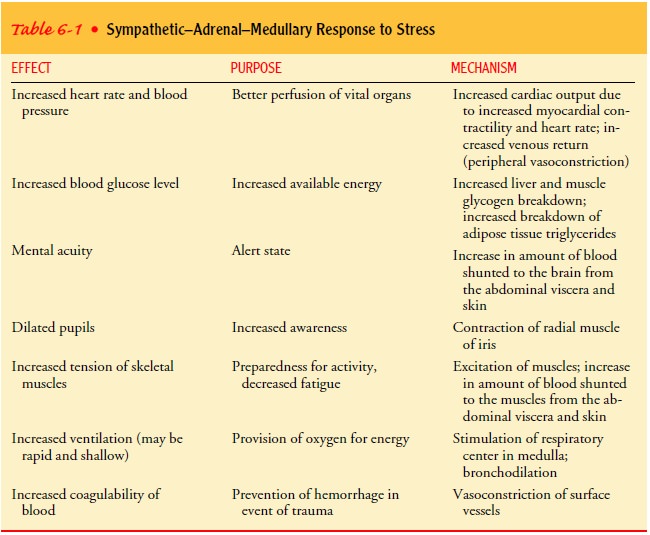
In addition to its direct effect on major end organs, the sympa-thetic nervous system also stimulates the medulla of the adrenal gland to release the hormones epinephrine and norepinephrine into the bloodstream. The action of these hormones is similar to that of the sympathetic nervous system and have the effect of sus-taining and prolonging its actions. Epinephrine and norepineph-rine are catecholamines that stimulate the nervous system and produce metabolic effects that increase the blood glucose level and increase the metabolic rate. The effect of the sympathetic and adrenal-medullary responses is summarized in Table 6-1. This effect is called the “fight-or-flight” reaction.
HYPOTHALAMIC-PITUITARY RESPONSE
The longest-acting phase
of the physiologic response, which is more likely to occur in persistent
stress, involves the hypothalamic-pituitary pathway. The hypothalamus secretes
corticotropin-releasing factor, which stimulates the anterior pituitary to
produce ACTH. ACTH in turn stimulates the adrenal cortex to produce glucocorticoids, primarily cortisol.
Cortisol stimulates proteincatabolism, releasing amino acids; stimulates liver
uptake of amino acids and their conversion to glucose (gluconeogenesis); and in-hibits glucose uptake (anti-insulin
action) by many body cells but not those of the brain and heart. These
cortisol-induced meta-bolic effects provide the body with a ready source of
energy during a stressful situation. This effect has some important
im-plications. For example, a person with diabetes who is under stress, such as
that caused by an infection, needs more insulin than usual. Any patient who is
under stress (caused, for example, by illness, surgery, trauma or prolonged
psychological stress) catab-olizes body protein and needs supplements. Children
subjected to severe stress have retarded growth.
The actions of the
catecholamines (epinephrine and norepi-nephrine) and cortisol are the most
important in the general response to stress. Other hormones released are antidiuretic hor-mone (ADH) from the
posterior pituitary and aldosterone fromthe adrenal cortex. ADH and aldosterone
promote sodium and water retention, which is an adaptive mechanism in the event
of hemorrhage or loss of fluids through excessive perspiration. ADH has also
been shown to influence learning and may thus facilitate coping in new and
threatening situations. Secretion of growth hormone and glucagon stimulates the
uptake of amino acids by
Endorphins, which are endogenous opiates, increase
during stress and enhance the threshold for tolerance of painful stimuli. They
may also affect mood and have been implicated in the so-called “high” that
long-distance runners experience. The secretion of other hormones is also
affected, but their adaptive function is less clear.
IMMUNOLOGIC RESPONSE
Research findings show
that the immune system is connected to the neuroendocrine and autonomic
systems. Lymphoid tissue is richly supplied by autonomic nerves capable of
releasing a num-ber of different neuropeptides that can have a direct effect on
leukocyte regulation and the inflammatory response. Neuro-endocrine hormones
released by the central nervous system and endocrine tissues can inhibit or
stimulate leukocyte function. The wide variety of stressors people experience
may result in different alterations in autonomic activity and subtle variations
in neuro-hormone and neuropeptide synthesis. All of these possible auto-nomic
and neuroendocrine responses can interact to initiate, weaken, enhance, or
terminate an immune response (Watkins, 1997).
The study of the relationships
among the neuroendocrine sys-tem, the central and autonomic nervous systems,
and the im-mune system and the effects of these relationships on overall health
outcomes is called psychoneuroimmunology.
Because one’s perception of events and coping styles determine whether, and to
what extent, an event activates the stress response system, and be-cause the
stress response affects immune activity, one’s percep-tions, ideas, and
thoughts can have profound neurochemical and immunologic consequences. Multiple
studies have demonstrated alteration of immune function in people who are under
stress, as evidenced by a decrease in the number of leukocytes, impaired immune
response to immunizations, and diminished cytotoxicity of natural killer cells
(Andersen et al., 1998; Constantino, Sec-ula, Rabin, & Stone, 2000; Glaser
& Kiecolt-Glaser, 1997; Pike et al., 1997; Robinson, Matthews, &
Witek-Janusek, 2000). Other studies have identified certain personality traits,
such as op-timism and active coping, as having positive effects on health or
specific immune measures (Chalfont & Bennett, 1999; Goodkin et al., 1996;
Kennedy, 2000; Sergerstrom, Fahey, Kemeny, & Taylor, 1998). As research
continues, this new field of study will continue to uncover to what extent and
by what mechanisms people can consciously influence their immunity.
Related Topics