Chapter: Medical Surgical Nursing: Homeostasis, Stress, and Adaptation
Cellular Response to Injury: Inflammation
CELLULAR
RESPONSE TO INJURY: INFLAMMATION
Cells or tissues of the
body may be injured or killed by any of the agents (physical, chemical,
infectious) described earlier. When this happens, an inflammatory response (or
inflammation) naturally occurs in the healthy tissues adjacent to the site of
injury. Inflam-mation is a defensive
reaction intended to neutralize, control, oreliminate the offending agent and
to prepare the site for repair. It is a nonspecific response (not dependent on
a particular cause) that is meant to serve a protective function. For example,
inflamma-tion may be observed at the site of a bee sting, in a sore throat, in
a surgical incision, and at a burn site. Inflammation also occurs in cell
injury events, such as strokes and myocardial infarctions.
Inflammation is not the
same as infection. An infectious agent is only one of several agents that may
trigger an inflammatory re-sponse. An infection exists when the infectious agent
is living, growing, and multiplying in the tissues and is able to overcome the
body’s normal defenses.
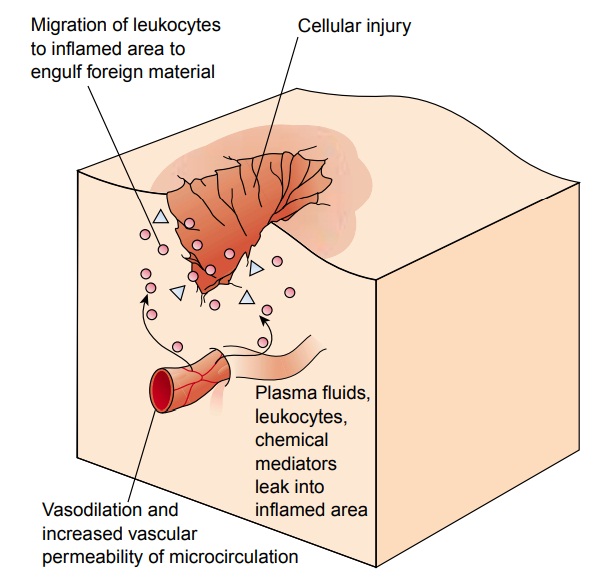
Regardless of the cause,
a general sequence of events occurs in the local inflammatory response. This
sequence involves changes in the microcirculation, including vasodilation,
increased vascu-lar permeability, and leukocytic cellular infiltration (Fig.
6-5). As these changes take place, five cardinal signs of inflammation are
produced: redness, heat, swelling, pain, and loss of function.
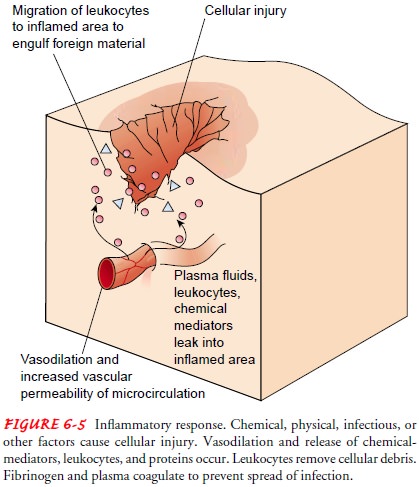
The transient
vasoconstriction that occurs immediately after injury is followed by
vasodilation and an increased rate of blood flow through the microcirculation.
Local heat and redness result. Next, vascular permeability increases, and
plasma fluids (includ-ing proteins and solutes) leak into the inflamed tissues,
produc-ing swelling. The pain produced is attributed to the pressure of fluids
or swelling on nerve endings, and to the irritation of nerve endings by
chemical mediators released at the site. Bradykinin is one of the chemical
mediators suspected of causing pain. Loss of function is most likely related to
the pain and swelling, but the exact mechanism is not completely known.
As blood flow increases
and fluid leaks into the surrounding tissues, the formed elements (red blood
cells, white blood cells, and platelets) remain in the blood, causing it to
become more vis-cous. Leukocytes (white blood cells) collect in the vessels,
exit, and migrate to the site of injury to engulf offending organisms and to
remove cellular debris in a process called phagocytosis. Fibrinogen in the
leaked plasma fluid coagulates, forming fibrin for clot formation, which serves
to wall off the injured area and prevent the spread of infection.
Chemical Mediators
Injury initiates the inflammatory response, but chemical sub-stances released at the site induce the vascular changes. Foremost among these chemicals are histamine and the kinins.
Histamine is present in many
tissues of the body but is concentrated in the mast cells. It is released when
injury occurs and is responsible for the early changes in vasodilation and
vascular permeability. Kinins increase vasodilation and vascular permeability;
they also attract neutrophils to the area. Prostaglandins, another group of
chemical substances, are also suspected of causing increased per-meability.
Systemic Response to Inflammation
The inflammatory
response is often confined to the site, causing only local signs and symptoms.
However, systemic responses can also occur. Fever is the most common sign of a
systemic response to injury, and it is most likely caused by endogenous
pyrogens (internal substances that cause fever) released from neutrophils and
macrophages (specialized forms of leukocytes). These sub-stances reset the
hypothalamic thermostat, which controls body temperature, and produce fever.
Leukocytosis, an increase in the synthesis and release of neutrophils from bone
marrow, may occur to provide the body with greater ability to fight infection.
During this process, general, nonspecific symptoms develop, in-cluding malaise,
loss of appetite, aching, and weakness.
Types of Inflammation
Inflammation is
categorized primarily by its duration and the type of exudate produced. It may
be acute, subacute, or chronic. Acute inflammation is characterized by the
local vascular and exudative changes described earlier and usually lasts less
than 2 weeks. An acute inflammatory response is immediate and serves a
protective
function. After the
injurious agent is removed, the inflammation subsides and healing takes place
with the return of normal or near-normal structure and function.
Chronic inflammation
develops if the injurious agent persists and the acute response is perpetuated.
Symptoms are present for many months or years. Chronic inflammation may also
begin in-sidiously and never have an acute phase. The chronic response does not
serve a beneficial and protective function; on the con-trary, it is
debilitating and can produce long-lasting effects. As the inflammation becomes
chronic, changes occur at the site of in-jury and the nature of the exudate
becomes proliferative. A cycle of cellular infiltration, necrosis, and fibrosis
begins, with repair and breakdown occurring simultaneously. Considerable
scarring may occur, resulting in permanent tissue damage.
Subacute inflammation
falls between acute and chronic in-flammation. It includes elements of the
active exudative phase of the acute response as well as elements of repair, as
in the chronic phase. The term subacute inflammation is not widely used.
Related Topics