Chapter: Medical Physiology: Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen Therapy
Physiologic Peculiarities of Specific Pulmonary Abnormalities
Physiologic Peculiarities of Specific Pulmonary Abnormalities
Chronic Pulmonary Emphysema
The term pulmonary emphysema literally means excess air in the lungs. However, this term is usually used to describe complex obstructive and destructive process of the lungs caused by many years of smoking. It results from the following major pathophysiologic changes in the lungs:
1. Chronic infection, caused by inhaling smoke orother substances that irritate the bronchi and bronchioles. The chronic infection seriously deranges the normal protective mechanisms of the airways, including partial paralysis of the cilia of the respiratory epithelium, an effect caused by nicotine. As a result, mucus cannot be moved easily out of the passageways. Also, stimulation of excess mucus secretion occurs, which further exacerbates the condition. Too, inhibition of the alveolar macrophages occurs, so that they become less effective in combating infection.
2. The infection, excess mucus, and inflammatory edema of the bronchiolar epithelium together cause chronic obstruction of many of the smaller airways.
3. The obstruction of the airways makes it especially difficult to expire, thus causing entrapment of
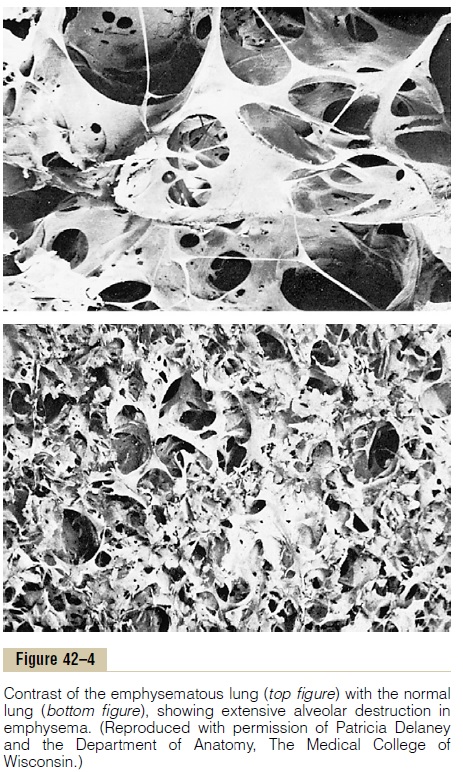
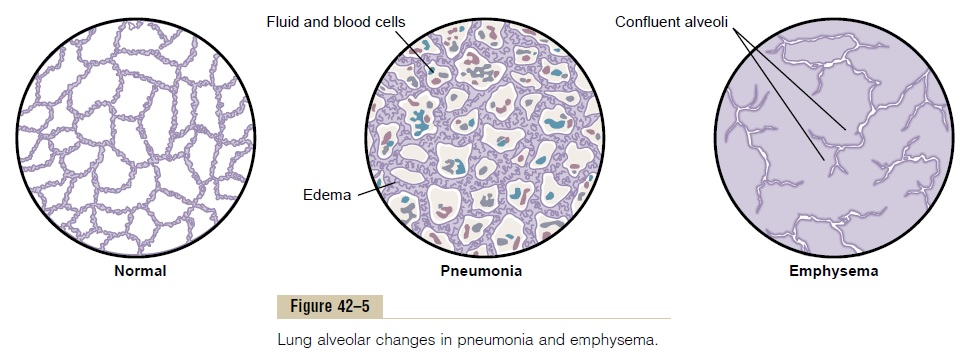
air in the alveoli and overstretching them. This,combined with the lung infection, causes markeddestruction of as much as 50 to 80 per cent of the alveolar walls. Therefore, thefinal picture of theemphysematous lung is that shown in Figures 42–4 (top) and 42–5.
The physiologic effects of chronic emphysema are extremely varied, depending on the severity of the disease and the relative degrees of bronchiolar ob-struction versus lung parenchymal destruction. Among the different abnormalities are the following:
1. The bronchiolar obstruction increases airwayresistance and results in greatly increased work ofbreathing. It is especially difficult for the person to move air through the bronchioles during expiration because the compressive force on the outside of the lung not only compresses the alveoli but also compresses the bronchioles, which further increases their resistance during expiration.
2. The marked loss of alveolar walls greatly decreases the diffusing capacity of the lung, whichreduces the ability of the lungs to oxygenate the blood and remove carbon dioxide from the blood.
3. The obstructive process is frequently much worse in some parts of the lungs than in other parts,so that some portions of the lungs are well ventilated, while other portions are poorly ventilated. This often causes extremely abnormalventilation..-perfusion ratios, with a very low Va/Q in some parts (physiologic shunt), resultingin poor aeration of the blood, and very high Va/Q in other parts (physiologic dead space), resulting in wasted ventilation, both effects occurring in the same lungs.
4. Loss of large portions of the alveolar walls also decreases the number of pulmonary capillaries through which blood can pass. As a result, the pulmonary vascular resistance often increases markedly, causing pulmonary hypertension. This in turn overloads the right side of the heart and frequently causes right-sided heart failure.
Chronic emphysema usually progresses slowly over many years. The person develops both hypoxia and hypercapnia because of hypoventilation of many alveoli plus loss of alveolar walls. The net result of all these effects is severe, prolonged, devastatingairhunger that can last for years until the hypoxia andhypercapnia cause death—a high penalty to pay for smoking.
Pneumonia
The term pneumonia includes any inflammatory con-dition of the lung in which some or all of the alveoli are filled with fluid and blood cells, as shown in Figure 42–5. A common type of pneumonia is bacterial pneu-monia, caused most frequently bypneumococci.This disease begins with infection in the alveoli; the pulmonary membrane becomes inflamed and highly porous so that fluid and even red and white blood cells leak out of the blood into the alveoli.
Thus, the infected alveoli become progressively filled with fluid and cells, and the infection spreads by extension of bacteria or virus from alveolus to alveolus. Eventually, large areas of the lungs, sometimes whole lobes or even a whole lung, become “consolidated,” which means that they are filled with fluid and cellular debris.
In pneumonia, the gas exchange functions of the lungs change in different stages of the disease. In early stages, the pneumonia process might well be localized to only one lung, with alveolar ventilation reduced while blood flow through the lung continues normally. This results in two major pulmonary abnormalities: (1) reduction in the total available surface area of the res-piratory membrane and (2) decreased ventilation-perfusion ratio. Both these effects cause hypoxemia (low blood oxygen) and hypercapnia(high blood carbon dioxide).
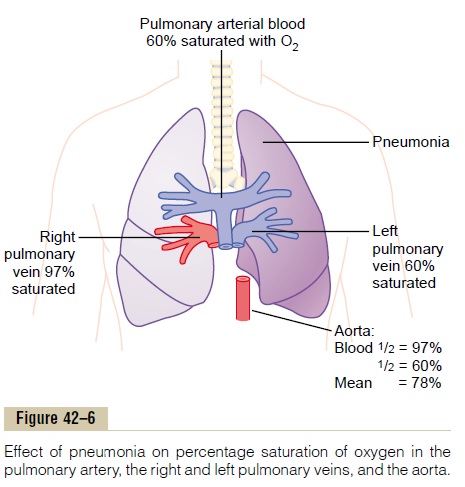
Figure 42–6 shows the effect of the decreased ventilation-perfusion ratio in pneumonia, showing that the blood passing through the aerated lung becomes 97 per cent saturated with oxygen, whereas that passing through the unaerated lung is about 60 per cent saturated. Therefore, the average saturation of the blood pumped by the left heart into the aorta is only about 78 per cent, which is far below normal.
Atelectasis
Atelectasis means collapse of the alveoli. It can occur in localized areas of a lung or in an entire lung. Its most common causes are (1) total obstruction of the airway or (2) lack of surfactant in the fluids lining the alveoli.
Airway Obstruction. The airway obstruction type ofatelectasis usually results from (1) blockage of many small bronchi with mucus or (2) obstruction of a major bronchus by either a large mucus plug or some solid object such as a tumor. The air entrapped beyond the block is absorbed within minutes to hours by the blood flowing in the pulmonary capillaries. If the lung tissue is pliable enough, this will lead simply to collapse of the alveoli.
However, if the lung is rigid because of fibrotic tissue and cannot collapse, absorption of air from the alveoli creates very negative pressures within the alveoli, which pull fluid out of the pulmonary cap-illaries into the alveoli, thus causing the alveoli to fill completely with edema fluid. This almost always is the effect that occurs when an entire lung becomes atelectatic, a condition called massive collapse of the lung.
The effects on overall pulmonary function caused by massive collapse (atelectasis) of an entire lung areshown in Figure 42–7. Collapse of the lung tissue not only occludes the alveoli but also almost always increases the resistance to blood flow through the pul-monary vessels of the collapsed lung. This resistance
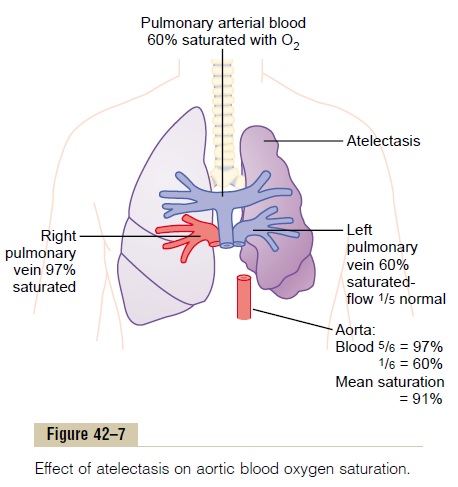
increase occurs partially because of the lung collapse itself, which compresses and folds the vessels as the volume of the lung decreases. In addition, hypoxia in the collapsed alveoli causes additional vasoconstriction.
Because of the vascular constriction, blood flow through the atelectatic lung becomes slight. Fortu-nately, most of the blood is routed through the venti-lated lung and therefore becomes well aerated. In the situation shown in Figure 42–7, five sixths of the blood passes through the aerated lung and only one sixth through the unaerated lung. As a result, the overall ventilation-perfusion ratio is only moderately com-promised, so that the aortic blood has only mild oxygen desaturation despite total loss of ventilation in an entire lung.
Lack of “Surfactant” as a Cause of Lung Collapse. The secre-tion and function of surfactant in the alveoli were discussed. It was pointed out that the surfactant is secreted by special alveolar epithelial cells into the fluids that coat the inside surface of the alveoli. The surfactant in turn decreases the surface tension in the alveoli 2- to 10-fold, which normally plays a major role in preventing alveolar collapse. However, in a number of conditions, such as in hyalinemembrane disease (also called respiratory distress syn-drome), which often occurs in newborn prematurebabies, the quantity of surfactant secreted by the alveoli is so greatly depressed that the surface tension of the alveolar fluid becomes several times normal. This causes a serious tendency for the lungs of these babies to collapse or to become filled with fluid. Many of these infants die of suffocation when large portions of the lungs become atelectatic.
Asthma
Asthma is characterized by spastic contraction of the smooth muscle in the bronchioles, which partially obstructs the bronchioles and causes extremely diffi-cult breathing. It occurs in 3 to 5 per cent of all people at some time in life.
The usual cause of asthma is contractile hypersensi-tivity of the bronchioles in response to foreign sub-stances in the air. In about 70 per cent of patients younger than age 30 years, the asthma is caused by allergic hypersensitivity, especially sensitivity to plant pollens. In older people, the cause is almost always hypersensitivity to nonallergenic types of irritants in the air, such as irritants in smog.
The allergic reaction that occurs in the allergic type of asthma is believed to occur in the following way:The typical allergic person has a tendency to form abnor-mally large amounts of IgE antibodies, and these anti-bodies cause allergic reactions when they react with the specific antigens that have caused them to develop in the first place. In asthma, these antibodies are mainly attached to mast cells that are present in the lung interstitium in close association with the bronchioles and small bronchi. When the asth-matic person breathes in pollen to which he or she is sensitive (that is, to which the person has developed IgE antibodies), the pollen reacts with the mast cell– attached antibodies and causes the mast cells to release several different substances. Among them are (a) histamine, (b)slow-reacting substance of anaphylaxis (which is a mixture of leukotrienes), (c) eosinophilicchemotactic factor, and (d) bradykinin. The combinedeffects of all these factors, especially the slow-reacting substance of anaphylaxis, are to produce (1) localized edema in the walls of the small bronchioles, as well as secretion of thick mucus into the bronchiolar lumens, and (2) spasm of the bronchiolar smooth muscle. Therefore, the airway resistance increases greatly.
As discussed earlier, the bronchiolar diameter becomes more reduced during expiration than during inspiration in asthma, caused by bronchi-olar collapse during expiratory effort that compresses the outsides of the bronchioles. Because the bronchi-oles of the asthmatic lungs are already partially occluded, further occlusion resulting from the external pressure creates especially severe obstruction during expiration. That is, the asthmatic person often can inspire quite adequately but has great difficulty expir-ing. Clinical measurements show (1) greatly reduced maximum expiratory rate and (2) reduced timed expi-ratory volume. Also, all of this together results in dyspnea, or “air hunger,” which is discussed later.
The functional residual capacity and residual volume of the lung become especially increased during the acute asthmatic attack because of the difficulty in expiring air from the lungs. Also, over a period of years, the chest cage becomes permanently enlarged, causing a “barrel chest,” and both the functional resid-ual capacity and lung residual volume become perma-nently increased.
Tuberculosis
In tuberculosis, the tubercle bacilli cause a peculiar tissue reaction in the lungs, including (1) invasion of the infected tissue by macrophages and (2) “walling off ” of the lesion by fibrous tissue to form the so-called tubercle. This walling-off process helps to limit furthertransmission of the tubercle bacilli in the lungs and therefore is part of the protective process against extension of the infection. However, in about 3 per cent of all people who develop tuberculosis, if untreated, the walling-off process fails and tubercle bacilli spread throughout the lungs, often causing extreme destruction of lung tissue with formation of large abscess cavities.
Thus, tuberculosis in its late stages is characterized by many areas of fibrosis throughout the lungs, as well as reduced total amount of functional lung tissue. These effects cause (1) increased “work” on the part of the respiratory muscles to cause pulmonary venti-lation and reduced vital capacity and breathing capac-ity; (2) reduced total respiratory membrane surface area and increased thickness of the respiratory membrane, causing progressively diminished pulmonary diffusingcapacity; and (3) abnormal ventilation-perfusion ratio in the lungs, further reducing overall pulmonary diffu-sion of oxygen and carbon dioxide.
Related Topics