Chapter: Medical Surgical Nursing: Assessment of Neurologic Function
Physical Examination - Assessment: The Neurologic Examination
PHYSICAL EXAMINATION
The neurologic examination is a systematic process
that includes a variety of clinical tests, observations, and assessments
designed to evaluate a complex system. Although the neurologic examination is
often limited to a simple screening, the examiner must be able to conduct a
thorough neurologic assessment when the patient’s history or other physical
findings warrant it..
The
brain and spinal cord cannot be examined as directly as other systems of the
body. Thus, much of the neurologic exami-nation is an indirect evaluation that
assesses the function of the specific body part or parts controlled or
innervated by the ner-vous system. A neurologic assessment is divided into five
compo-nents: cerebral function, cranial nerves, motor system, sensory system,
and reflexes. As in other parts of the physical assessment, the neurologic
examination follows a logical sequence and pro-gresses from higher levels of
cortical function such as abstract thinking to lower levels of function such as
the determination of the integrity of peripheral nerves.
Assessing Cerebral Function
Cerebral
abnormalities may cause disturbances in mental status, intellectual
functioning, and thought content and in patterns of emotional behavior. There
may also be alterations in perception, motor and language abilities, as well as
lifestyle.
MENTAL STATUS
An assessment of mental status begins by observing
the patient’s appearance and behavior, noting dress, grooming, and personal
hygiene. Posture, gestures, movements, facial expressions, and motor activity
often provide important information about the pa-tient. The patient’s manner of
speech and level of consciousness are also assessed. Is the patient’s speech
clear and coherent? Is the patient alert and responsive, or drowsy and
stuporous?
Assessing orientation to time, place, and person
assists in eval-uating mental status. Does the patient know what day it is,
what year it is, and the name of the president of the United States? Is the
patient aware of where he or she is? Is the patient aware of who the examiner
is and of his or her purpose for being in the room? Is the capacity for
immediate memory intact?
INTELLECTUAL FUNCTION
A
person with an average IQ can repeat seven digits without fal-tering and can
recite five digits backward. The examiner might ask the patient to count
backward from 100 or to subtract 7 from 100, then 7 from that, and so forth
(called serial 7s) ( Johnson, 2001). The capacity to interpret well-known
proverbs tests ab-stract reasoning, which is a higher intellectual function; for
ex-ample, does the patient know what is meant by “the early bird catches the
worm”? Patients with damage to the frontal cortex appear superficially normal
until one or more tests of integrative capacity are performed. Questions
designed to assess this capac-ity might include the ability to recognize
similarities: how are a mouse and dog or pen and pencil alike? Can the patient
make judgements about situations—for instance, if the patient arrived home
without a house key, what alternatives are there?
THOUGHT CONTENT
During
the interview, it is important to assess the patient’s thought content. Are the
patient’s thoughts spontaneous, natural, clear, relevant, and coherent? Does
the patient have any fixed ideas, illusions, or preoccupations? What are his or
her insights into these thoughts? Preoccupation with death or morbid events,
hallucinations, and paranoid ideation are examples of unusual thoughts or
perceptions that require further evaluation.
EMOTIONAL STATUS
An assessment of cerebral functioning also includes
the patient’s emotional status. Is the patient’s affect (external manifestation
of mood) natural and even, or irritable and angry, anxious, apathetic or flat,
or euphoric? Does his or her mood fluctuate normally, or does the patient
unpredictably swing from joy to sadness during the interview? Is affect
appropriate to words and thought content? Are verbal communications consistent
with nonverbal cues?
PERCEPTION
The
examiner may now consider more specific areas of higher cortical function. Agnosia is the inability to interpret
or recog-nize objects seen through the special senses. The patient may see a
pencil but not know what it is called or what to do with it. The patient may
even be able to describe it but not to interpret its function. The patient may
experience auditory or tactile agnosia as well as visual agnosia. Each of the
dysfunctions implicates a dif-ferent part of the cortex (Chart 60-1).
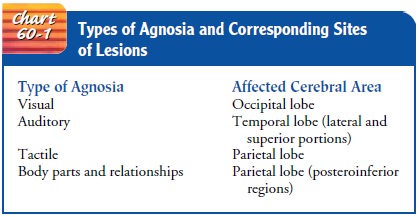
Screening
for visual and tactile agnosia provides insight into the patient’s cortical
interpretation ability. The patient is shown a familiar object and asked to
identify it by name. Placing a fa-miliar object (eg, key, coin) in the
patient’s hand and having him or her identify it with both eyes closed is an
easy way to assess tac-tile interpretation.
MOTOR ABILITY
Assessment of cortical motor integration is carried out by asking the patient to perform a skilled act (throw a ball, move a chair). Successful performance requires the ability to understand the ac-tivity desired and normal motor strength. Failure signals cerebral dysfunction.
LANGUAGE ABILITY
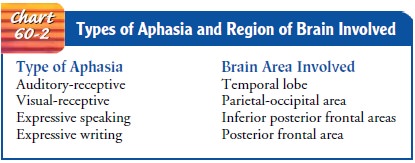
The person with normal neurologic function can
understand and communicate in spoken and written language. Does the patient
answer questions appropriately? Can he or she read a sentence from a newspaper
and explain its meaning? Can the patient write his or her name or copy a simple
figure that the examiner has drawn? A deficiency in language function is called
aphasia. Dif-ferent types of aphasia result from injury to different parts of
the brain (Chart 60-2).
IMPACT ON LIFESTYLE
The
nurse assesses the impact the neurologic impairment has on the patient’s
lifestyle. Issues to consider include the limitations imposed on the patient by
any deficit and the patient’s role in so-ciety, including family and community
roles. The plan of care that the nurse develops needs to address and support
adaptation to the neurologic deficit and continued function to the extent
possible within the patient’s support system.
DOCUMENTATION OF FINDINGS
Interpretation
and documentation of neurologic abnormalities, particularly mental status
abnormalities, should be specific and nonjudgmental. Lengthy descriptions and
the use of terms such as “inappropriate” or “demented” should be avoided. Terms
such as these often mean different things to different people and are therefore
not useful when describing behavior. The examiner records and reports specific
observations regarding orientation, level of consciousness, emotional state, or
thought content, all of which permit comparison by others over time. Analysis
and the conclusions that may be drawn from these findings usually de-pend on
the examiner’s knowledge of neuroanatomy, neuro-physiology, and neuropathology.
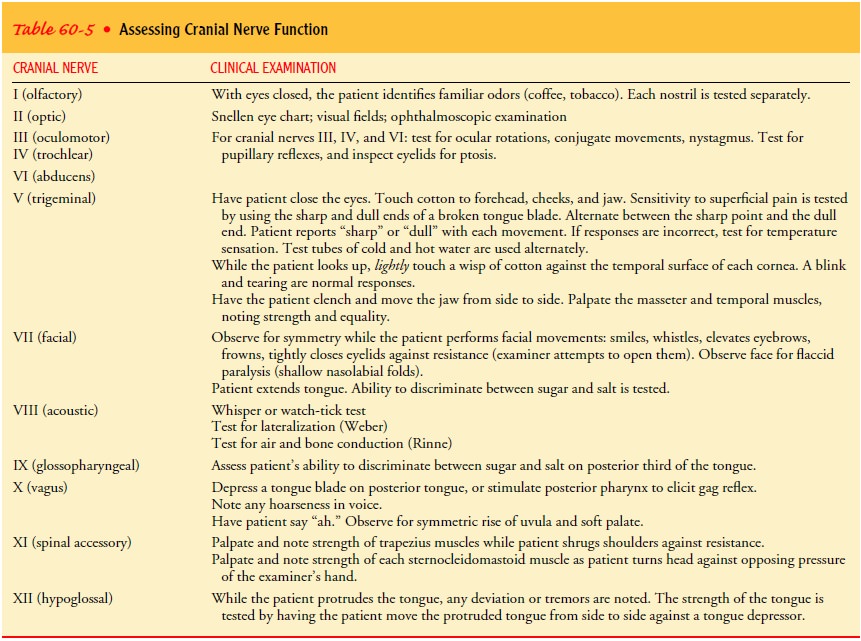
Examining the Cranial Nerves
Table 60-5 describes how to assess the cranial
nerves. Opposite sides of the face and neck are compared throughout the
examination.
Examining the Motor System
A thorough examination of the motor system includes an assess-ment of muscle size, tone, and strength, coordination, and balance. The patient is instructed to walk across the room while the exam-iner observes posture and gait. The muscles are inspected, and pal-pated if necessary, for their size and symmetry. Any evidence of atrophy or involuntary movements (tremors, tics) is noted. Mus-cle tone (the tension present in a muscle at rest) is evaluated by pal-pating various muscle groups at rest and during passive movement. Resistance to these movements is assessed and documented. Abnormalities in tone include spasticity (increased muscle tone), rigidity (resistance to passive stretch), and flaccidity.
MUSCLE STRENGTH
Assessing
the patient’s ability to flex or extend the extremities against resistance
tests muscle strength. The function of an in-dividual muscle or group of
muscles is evaluated by placing the muscle at a disadvantage. The quadriceps,
for example, is a pow-erful muscle responsible for straightening the leg. Once the
leg is straightened, it is exceedingly difficult for the examiner to flex the
knee. Conversely, if the knee is flexed and the patient is asked to straighten
the leg against resistance, a more subtle disability can be elicited. The
evaluation of muscle strength compares the sides of the body to each other. For
example, the right upper ex-tremity is compared to the left upper extremity. In
this way, sub-tle differences in muscle strength can be more easily detected
and accurately described.
Clinicians
use a five-point scale to rate muscle strength (O’Hanlon-Nichols, 1999). A 5
indicates full power of contrac-tion against gravity and resistance or normal
muscle strength; 4 indicates fair but not full strength against gravity and a
moderate amount of resistance or slight weakness; 3 indicates just sufficient
strength to overcome the force of gravity or moderate weakness; 2 indicates the
ability to move but not to overcome the force of gravity or severe weakness; 1
indicates minimal contractile power—weak muscle contraction can be palpated but
no movement is noted—or very severe weakness; and 0 indicates complete
paralysis. A stick figure may be used to record muscle strength and is a
precise form of documenting findings. Distal and proximal strength in both upper
and lower extremities is recorded using the five-point scale (Fig. 60-14).

Assessment
of muscle strength can be as detailed as necessary. One may quickly test the
strength of the proximal muscles of the upper and lower extremities, always
comparing both sides. The strength of the finer muscles that control the
function of the hand (hand grasp) and the foot (dorsiflexion and plantar
flexion) can then be assessed.
BALANCE AND COORDINATION
Cerebellar influence on the motor system is
reflected in balance control and coordination. Coordination in the hands and
upper extremities is tested by having the patient perform rapid, alternat-ing
movements and point-to-point testing. First, the patient is in-structed to pat
his or her thigh as fast as possible with each hand separately. Then the
patient is instructed to alternately pronate and supinate the hand as rapidly
as possible. Lastly, the patient is asked to touch each of the fingers with the
thumb in a consecutive motion. Speed, symmetry, and degree of difficulty are
noted.
Point-to-point testing is accomplished by having the patient touch the examiner’s extended finger and then his or her own nose. This is repeated several times. This assessment is then car-ried out with the patient’s eyes closed.
Coordination
in the lower extremities is tested by having the patient run the heel down the
anterior surface of the tibia of the other leg. Each leg is tested in turn. Ataxia is defined as incoor-dination of
voluntary muscle action, particularly of the muscle groups used in activities
such as walking or reaching for objects. The presence of ataxia or tremors
(rhythmic, involuntary move-ments) during these movements suggests cerebellar
disease.
It
is not necessary to carry out each of these assessments for co-ordination.
During a routine examination, it is advisable to per-form a simple screening of
the upper and lower extremities by having the patient perform either rapid,
alternating movements or point-to-point testing. When abnormalities are
observed, a more thorough examination is indicated.
The
Romberg test is a screening test for
balance. The patient stands with feet together and arms at the side, first with
eyes open and then with both eyes closed for 20 to 30 seconds. The exam-iner
stands close to reassure the patient of support if he or she be-gins to fall.
Slight swaying is normal, but a loss of balance is abnormal and is considered a
positive Romberg test. Additional cerebellar tests for balance in the
ambulatory patient include hop-ping in place, alternating knee bends, and
heel-to-toe walking (both forward and backward).
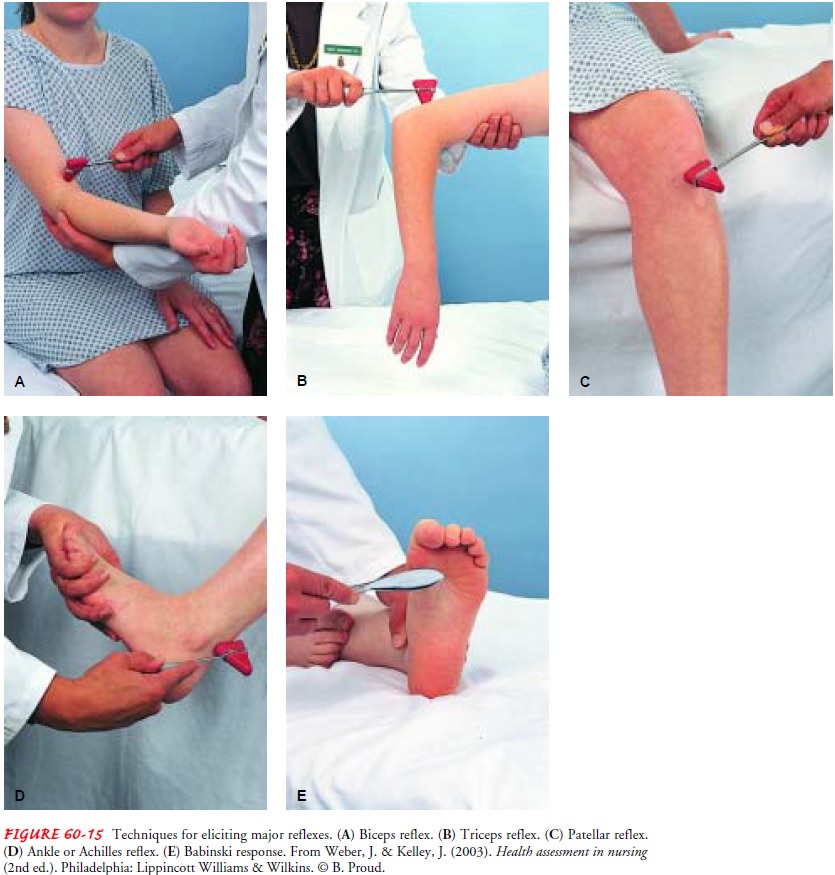
Examining the Reflexes
The motor reflexes are involuntary contractions of
muscles or muscle groups in response to abrupt stretching near the site of the
muscle’s insertion. The tendon is struck directly with a reflex hammer or
indirectly by striking the examiner’s thumb, which is placed firmly against the
tendon. Testing these reflexes enables the examiner to assess involuntary
reflex arcs that depend on the presence of afferent stretch receptors, spinal
synapses, efferent motor fibers, and a variety of modifying influences from
higher levels. Common reflexes that may be tested include the deep ten-don
reflexes (biceps, brachioradialis, triceps, patellar, and ankle reflexes) and
superficial or cutaneous reflexes (abdominal reflexes and plantar or Babinski
response) (Fig. 60-15).
TECHNIQUE
A reflex hammer is used to elicit a deep tendon
reflex. The han-dle of the hammer is held loosely between the thumb and index
finger, allowing a full swinging motion. The wrist motion is sim-ilar to that
used during percussion. The extremity is positioned so that the tendon is
slightly stretched. This requires a sound knowledge of the location of muscles
and their tendon attach-ments. The tendon is then struck briskly, and the
response is compared with that on the opposite side of the body. A wide
vari-ation in reflex response may be considered normal; it is more im-portant,
however, that the reflexes be symmetrically equivalent. When the comparison is
made, both sides should be equivalently relaxed and each tendon struck with
equal force.
Valid
findings depend on several factors: proper use of the re-flex hammer, proper
positioning of the extremity, and a relaxed patient. If the reflexes are
symmetrically diminished or absent, the examiner may use reinforcement to
increase reflex activity. This involves the isometric contraction of other
muscle groups. If lower extremity reflexes are diminished or absent, the
patient is instructed to lock the fingers together and pull in opposite
direc-tions. Having the patient clench the jaw or press the heels against the
floor or examining table may similarly elicit more reliable bi-ceps, triceps,
and brachioradialis reflexes.
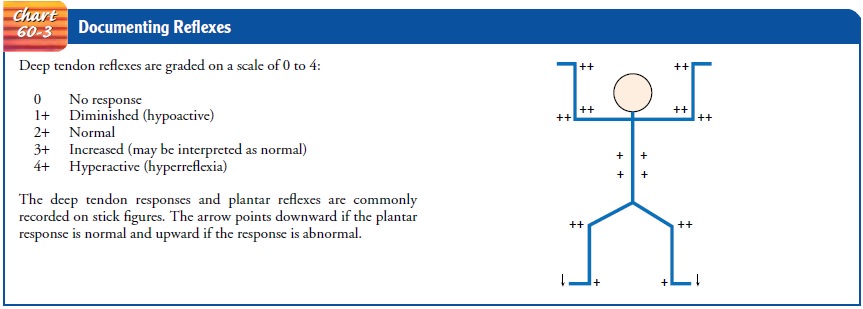
GRADING THE REFLEXES
The absence of reflexes is significant, although
ankle jerks (Achilles reflex) may be normally absent in older people. Deep
tendon re-flex responses are often graded on a scale of 0 to 4+. A 4+ indicates a hyperactive
reflex, often indicating pathology; 3+
indicates a re-sponse that is more brisk than average but may be normal or
in-dicative of disease; 2+ indicates an average or
normal response; 1+ indicates a hypoactive or diminished response; and
0 indicates no response. As stated previously, scale ratings are highly
subjective. Findings can be recorded as a fraction, indicating the scale range
(eg, 2/4). Some examiners prefer to use the terms present, absent, and
diminished when describing reflexes. As with muscle strength recording, a stick
figure such as the one shown in Chart 60-3 may also be used to record numerical
findings.
BICEPS REFLEX
The biceps reflex is elicited by striking the
biceps tendon of the flexed elbow. The examiner supports the forearm with one
arm while placing the thumb against the tendon and striking the thumb with the
reflex hammer. The normal response is flexion at the elbow and contraction of
the biceps (see Fig. 60-15A).
TRICEPS REFLEX
To
elicit a triceps reflex, the patient’s arm is flexed at the elbow and positioned
in front of the chest. The examiner supports the patient’s arm and identifies
the triceps tendon by palpating 2.5 to 5 cm (1 to 2 in) above the elbow. A
direct blow on the tendon normally produces contraction of the triceps muscle
and exten-sion of the elbow (see Fig. 60-15B).
BRACHIORADIALIS REFLEX
With
the patient’s forearm resting on the lap or across the ab-domen, the
brachioradialis reflex is assessed. A gentle strike of the hammer 2.5 to 5 cm
(1 to 2 in) above the wrist results in flexion and supination of the forearm.
PATELLAR REFLEX
The patellar reflex is elicited by striking the patellar tendon just below the patella. The patient may be in a sitting or a lying position. If the patient is supine, the examiner supports the legs to fa-cilitate relaxation of the muscles. Contractions of the quadriceps and knee extension are normal responses (see Fig. 60-15C ).
ANKLE REFLEX
To
elicit an ankle (Achilles) reflex, the foot is dorsiflexed at the ankle and the
hammer strikes the stretched Achilles tendon (see Fig. 60-15D). This reflex normally produces
plantar flexion. If the examiner cannot elicit the ankle reflex and suspects
that the patient cannot relax, the patient is instructed to kneel on a chair or
similar elevated, flat surface. This position places the ankles in dorsiflexion
and reduces any muscle tension in the gastroc-nemius. The Achilles tendons are
struck in turn, and plantar flex-ion is usually demonstrated.
CLONUS
When reflexes are very hyperactive, a phenomenon
called clonus may be elicited. If
the foot is abruptly dorsiflexed, it may continue to “beat” two or three times
before it settles into a position of rest. Occasionally with central nervous
system disease this activity per-sists and the foot does not come to rest while
the tendon is being stretched but persists in repetitive activity. The
unsustained clonus associated with normal but hyperactive reflexes is not
considered pathologic. Sustained clonus always indicates the presence of
cen-tral nervous system disease and requires further evaluation.
SUPERFICIAL REFLEXES
The major superficial reflexes include corneal, gag or swallowing, upper/lower abdominal, cremasteric (men only), plantar, and perianal.
These reflexes are graded differently
than the motor re-flexes and are noted to be present (+)
or absent (-). Of these, only three are tested commonly. The corneal reflex is
tested carefully using a clean wisp of cotton and lightly touching the outer
cor-ner of each eye on the sclera. The reflex is present if the action elicits
a blink. Conditions such as a cerebrovascular accident or coma might result in
loss of this reflex, either unilaterally or bi-laterally. Loss of this reflex
indicates the need for eye protection and possible lubrication to prevent
corneal damage.
The
gag reflex is elicited by gently touching the posterior phar-ynx with a
cotton-tipped applicator; first on one side of the uvula and then the other.
Positive response is an equal elevation of the uvula and “gag” with
stimulation. Absent response on one or both sides can be seen following a
cerebrovascular accident and requires careful evaluation and treatment of the
resultant swal-lowing dysfunction to prevent aspiration of food and fluids into
the lungs.
The
plantar reflex is elicited by stroking the lateral side of the foot with a
tongue blade or the handle of a reflex hammer. Stimulation normally causes toe
flexion. Toe fanning (positive Babinski) is an abnormal response and is
discussed below (O’Hanlon-Nichols, 1999).
BABINSKI RESPONSE
A
well-known reflex indicative of central nervous system disease affecting the
corticospinal tract is the Babinski
reflex. In some-one with an intact central nervous system, if the lateral
aspect of the sole of the foot is stroked, the toes contract and are drawn
to-gether (see Fig. 60-15E ). In
patients who have central nervous system disease of the motor system, however,
the toes fan out and are drawn back. This is normal in newborns but represents
a se-rious abnormality in adults. Several other reflexes convey similar
information. Many of them are interesting but not particularly informative.
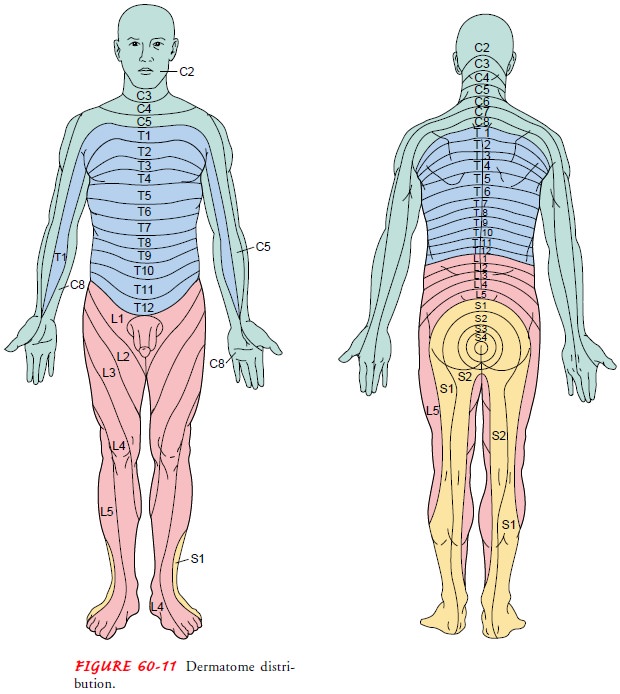
Sensory Examination
The sensory system is even more complex than the
motor system because sensory modalities are carried in different tracts located
in different portions of the spinal cord. The sensory examination is largely
subjective and requires the cooperation of the patient. The examiner should be
familiar with dermatomes that represent the distribution of the peripheral nerves
that arise from the spinalcord (see Fig. 60-11). Most
sensory deficits result from periph-eral neuropathy and follow anatomic
dermatomes. Exceptions to this include major destructive lesions of the brain;
loss of sen-sation, which may affect an entire side of the body; and the
neuropathies associated with alcoholism, which occur in a glove-and-stocking
distribution or over the entire hand or foot in areas traditionally covered by
a glove or sock.
Assessment
of the sensory system involves tests for tactile sen-sation, superficial pain,
vibration, and position sense (proprio-ception). During the sensory assessment,
the patient’s eyes are closed. Simple directions and reassurance that the
examiner will not hurt or startle the patient encourage the cooperation of the
patient.
Tactile
sensation is assessed by lightly touching a cotton wisp to corresponding areas
on each side of the body. The sensitivity of proximal parts of the extremities
is compared with that of distal parts.
Pain
and temperature sensations are transmitted together in the lateral part of the
spinal cord, so it is unnecessary to test for temperature sense in most
circumstances. Determining the patient’s sensitivity to a sharp object can
assess superficial pain perception. The patient is asked to differentiate
between the sharp and dull ends of a broken wooden cotton swab or tongue blade;
using a safety pin is inadvisable because it breaks the integrity of the skin.
Both the sharp and dull sides of the object are applied with equal intensity at
all times, and as with the motor evaluation the two sides are compared.
Vibration and proprioception are transmitted
together in the posterior part of the cord. Vibration may be evaluated through
the use of a low-frequency (128- or 256-Hz) tuning fork. The handle of the
vibrating fork is placed against a bony prominence, and the patient is asked
whether he or she feels a sensation and is instructed to signal the examiner
when the sensation ceases. Common locations used to test for vibratory sense include
the distal joint of the great toe and the proximal thumb joint. If the patient
does not perceive the vibrations at the distal bony promi-nences, the examiner
progresses upward with the tuning fork until the patient perceives the
vibrations. As with all measure-ments of sensation, a side-to-side comparison
is made.
Position sense or proprioception may be determined
by ask-ing the patient to close both eyes and indicate, as the great toe is
alternately moved up and down, in which direction movement has taken place.
Vibration and position sense are often lost together, frequently in
circumstances in which all others remain intact.
Integration
of sensation in the brain is evaluated next. This may be performed by testing
two-point discrimination—when the patient is touched with two sharp objects
simultaneously, are they perceived as two or as one? If touched simultaneously
on op-posite sides of the body, the patient should normally report being
touched in two places. If only one site is reported, the one not being
recognized is said to demonstrate extinction. Another test of higher cortical
sensory ability is stereognosis. The patient is in-structed to close both eyes
and identify a variety of objects (eg, keys, coins) that are placed in one hand
by the examiner.
Gerontologic Considerations
The nervous system undergoes many changes during
the normal aging process and is extremely vulnerable to general systemic
ill-ness. Changes throughout the nervous system vary in degree as the person
ages. Nerve fibers that connect directly to muscles show little decline in
function with age, as do simple neurologic functions that involve a number of
connections in the spinal cord. Disease in the elderly often makes it difficult
to distinguish normal from abnormal changes. However, it is important for
clinicians not to attribute abnormality or dysfunction to aging without
appropriate investigation (Kaye & Quinn, 2000).
Structural Changes.
There are a number of
alterations that occurwith increasing age. Brain weight decreases, as does the
number of synapses. A loss of neurons occurs in select regions of the brain.
There is a reduction in cerebral blood flow and metabolism. Temperature
regulation becomes less efficient. In the peripheral nervous system, myelin is
lost, resulting in a decrease in conduc-tion velocity in some nerves. There is
an overall reduction in muscle bulk and the electrical activity within muscles.
Taste buds atrophy and nerve cell fibers in the olfactory bulb degenerate.
Nerve cells in the vestibular system of the inner ear, cerebellum, and
proprioceptive pathways also degenerate. Deep tendon re-flexes can be decreased
or in some cases absent. Hypothalamic function is modified such that stage IV
sleep is reduced. There is an overall slowing of autonomic nervous system
responses. Pupil-lary responses are reduced or may not appear at all in the
presence of cataracts (Kaye & Quinn, 2000).
Motor Alterations.
There is an overall reduction in muscle bulk,with
atrophy most easily noted in the hands (Kaye & Quinn, 2000). Changes in
motor function often result in a flexed posture, shuffling gait, and rigidity
of movement. These changes can create difficulties for the older person in
maintaining or recovering bal-ance. Strength and agility are diminished, and
reaction time and movement time are decreased. Repetitive movements and mild
tremors may be noted during an examination and may be of con-cern to the
individual. Observation of gait may reveal a wide-based gait with balance
difficulties.
Sensory Alterations.
Sensory isolation due to visual and hearingloss can
cause confusion, anxiety, disorientation, misinterpretation of the environment,
and feelings of inadequacy. Sensory alter-ations may require modification of
the home environment, such as large-print reading materials or sound
enhancement for the telephone, as well as extra orientation to new
surroundings. Simple explanations of routines, the location of the bathroom,
and how to operate the call bell are just a few examples of infor-mation the
elderly patient needs when hospitalized.
Temperature Regulation and Pain Perception.
Other manifesta-tions of neurologic changes are
related to temperature regulation and pain. The elderly patient may feel cold
more readily than heat and may require extra covering when in bed; a room
temperature somewhat higher than usual may be desirable. Reaction to painful
stimuli may be decreased with age. Because pain is an important warning signal,
caution must be used when hot or cold packs are used. The older patient may be
burned or suffer frostbite before being aware of any discomfort. Complaints of
pain, such as ab-dominal discomfort or chest pain, may be more serious than the
patient’s perception might indicate and thus require careful evaluation.
Taste and Smell Alterations.
The acuity of the taste buds de-creases with age; along with an altered
olfactory sense, this may cause a decreased appetite and subsequent weight
loss. Extra sea-soning often increases food intake as long as it does not cause
gastric irritation. A decreased sense of smell due to atrophy of olfactory
organs may present a safety hazard, because elderly people living alone may be
unable to detect household gas leaks or fires. Smoke and carbon monoxide
detectors, important for all, are critical for the elderly.
Tactile and Visual Alterations.
Another neurologic
alteration inthe elderly patient is the dulling of tactile sensation due to a
de-crease in the number of areas of the body responding to all stimuli and in
the number and sensitivity of sensory receptors. There may be difficulty in
identifying objects by touch, and because fewer tactile cues are received from
the bottom of the feet, the person may get confused as to body position and
location.
These factors, combined with sensitivity to glare,
decreased peripheral vision, and a constricted visual field, may result in
dis-orientation, especially at night when there is little or no light in the
room. Because the elderly person takes longer to recover visual sensitivity
when moving from a light to dark area, night-lights and a safe and familiar
arrangement of furniture are essential.
Mental Status.
Mental status is evaluated while the history is ob-tained, and areas of
judgment, intelligence, memory, affect, mood, orientation, speech, and grooming
are assessed. Family members who bring the patient to the attention of the
health care provider may have noticed changes in the patient’s mental status.
Drug toxicity should always be suspected as a causative factor when the patient
has a change in mental status. Delirium
(mental confu-sion, usually with delusions and hallucinations) is seen in
elderly patients who have underlying central nervous system damage or are
experiencing an acute condition such as infection, adverse medication reaction,
or dehydration. About 25% of patients over the age of 70 admitted to the
hospital have delirium ( Johnson, 2001). The cause is often reversible and
treatable (as in drug toxi-city, vitamin B deficiency, or thyroid disease).
Depression may produce impairment of attention and memory. For elderly
pa-tients, delirium, which is an acute change in mental status attrib-utable to
a treatable medical problem, must be differentiated from dementia, which is a
chronic and irreversible deterioration of cognitive status.
Nursing Implications.
Nursing care for patients with age-relatedchanges to the nervous system and
for patients with long-term neurologic disability who are aging should include
the modifica-tions previously described. In addition, the consequences of any
neurologic deficit and its impact on overall function such as ac-tivities of
daily living, use of assistive devices, and individual coping need to be
assessed and considered in planning care for patients.
Patient
teaching is also affected because the nurse must un-derstand the altered responses
and the changing needs of the el-derly patient before beginning to teach. When
caring for the elderly patient, the nurse adapts activities such as
preoperative teaching, diet therapy, and instruction about new medications,
their timing, and doses to the patient’s needs and capabilities. The nurse
considers the presence of decline in fine motor move-ment and failing vision.
When using visual materials for teaching or menu selection, adequate lighting
without glare, contrasting colors, and large print are used to offset visual
difficulties caused by rigidity and opacity of the lens in the eye and slower
pupillary reaction.
Procedures and preparations needed for diagnostic
tests are ex-plained, taking into account the possibility of impaired hearing and
slowed responses in the elderly. Even with hearing loss, the elderly patient
often hears adequately if the speaker uses a low-pitched, clear voice; shouting
only makes it harder for the patient to understand the speaker. Providing
auditory and visual cues aids understanding; if the patient has a significant
hearing or vi-sual loss, assistive devices, a signer, or a translator may be
needed.
Teaching
at an unrushed pace and using reinforcement en-hance learning and retention.
Material should be short, concise, and concrete. Vocabulary is matched to the
patient’s ability, and terms are clearly defined. The elderly patient requires
adequate time to receive and respond to stimuli, to learn, and to react. These
measures allow comprehension, memory, and formation of association and
concepts.
Related Topics