Chapter: Medical Surgical Nursing: Assessment of Neurologic Function
Motor and Sensory Functions of the Nervous System
Motor and Sensory Functions of the Nervous System
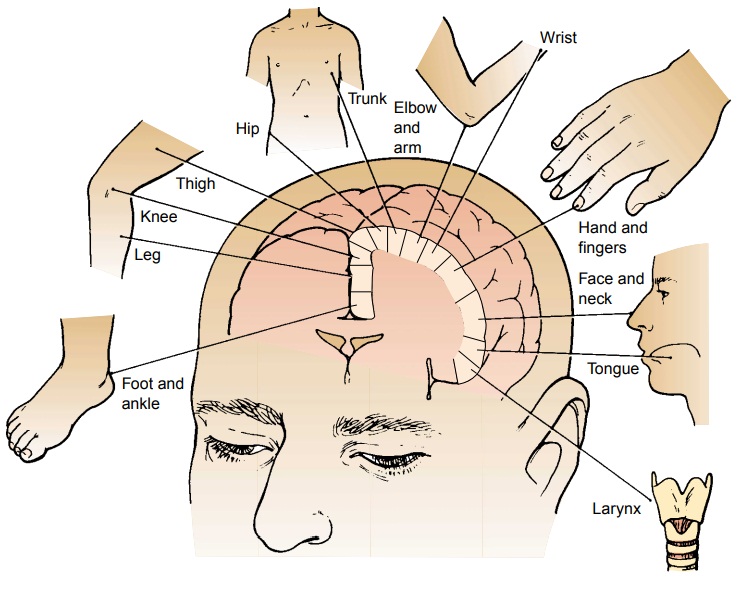
MOTOR SYSTEM FUNCTION
The motor cortex, a vertical band within each
cerebral hemi-sphere, controls the voluntary movements of the body. The exact
locations within the brain at which the voluntary movements of the muscles of
the face, thumb, hand, arm, trunk, and leg origi-nate are known (Fig. 60-13).
To initiate muscle movement, these particular cells must send the stimulus down
along their fibers. Stimulation of these cells with an electric current will
also result in muscle contraction. En route to the pons, the motor fibers
converge into a tight bundle known as the internal capsule. A com-paratively
small injury to the capsule causes paralysis in more muscles than does a much
larger injury to the cortex itself.
Within the medulla, the motor axons from the cortex
form the motor pathways or tracts, notably the corticospinal or pyramidal
tracts. Here, most of the fibers cross (or decussate) to the oppo-site side,
continuing as a crossed pyramidal tract. The remaining fibers enter the spinal
cord on the same side as the direct pyrami-dal tract. Each fiber in this tract
finally crosses to the opposite side of the cord and terminates within the gray
matter of the anterior horn on that side, in proximity to a motor nerve cell.
Fibers of the crossed pyramidal tract terminate within the anterior horn and
make connections with anterior horn cells on the same side. All of the motor
fibers of the spinal nerves represent extensions of these anterior horn cells,
with each of these fibers communicat-ing with only one particular muscle fiber.
The motor system is complex, and motor function depends on the integrity of the corticospinal tracts, the extrapyramidal system, and cerebellar function. A motor impulse consists of a two-neuron pathway (described below). The motor nerve pathways are contained in the spinal cord. Some represent the pathways of the so-called extrapyramidal system, establishing connections be-tween the anterior horn cells and the automatic control centers located in the basal ganglia and the cerebellum. Others are components of reflex arcs, forming synaptic connections between anterior horn cells and sensory fibers that have entered adjacent or neighboring segments of the cord.
Upper and Lower Motor Neurons.
The voluntary motor systemconsists of two groups of
neurons: upper motor neurons and lower motor neurons. Upper motor neurons
originate in the cere-bral cortex, the cerebellum, and the brain stem and
modulate the activity of the lower motor neurons. Upper motor neuron fibers
make up the descending motor pathways and are located entirely within the CNS.
Lower motor neurons are located either in the anterior horn of the spinal cord
gray matter or within cranial nerve nuclei in the brain stem. Axons of both
extend through pe-ripheral nerves and terminate in skeletal muscle. Lower motor
neurons are located in both the CNS and the peripheral nervous system.
The
motor pathways from the brain to the spinal cord, as well as from the cerebrum
to the brain stem, are formed by upper motor neurons. They begin in the cortex
of one side of the brain, descend through the internal capsule, cross to the
opposite side in the brain stem, descend through the corticospinal tract, and
synapse with the lower motor neurons in the cord. The lower motor neurons
receive the impulse in the posterior part of the cord and run to the myoneural
junction located in the periph-eral muscle. The clinical features of lesions of
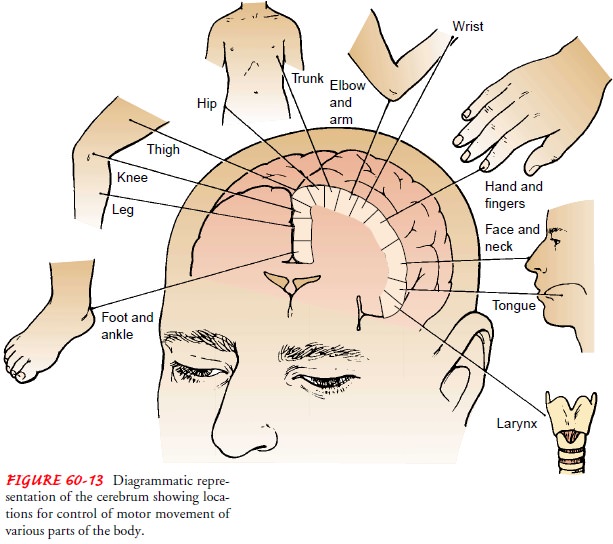
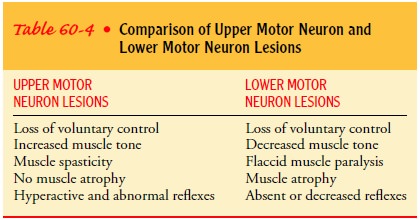
upper and lower motor neurons are discussed in the sections that follow and in
Table 60-4.
Upper Motor Neuron Lesions. Upper motor neuron
lesions can involve the motor cortex, the internal capsule, the spinal cord,
and other structures of the brain through which the corticospinal tract descends.
If the upper motor neurons are damaged or de-stroyed, as frequently occurs with
stroke or spinal cord injury, paralysis (loss of voluntary movement) results.
However, because the inhibitory influences of intact upper motor neurons are
now impaired, reflex (involuntary) movements are uninhibited, and hence
hyperactive deep tendon reflexes, diminished or absent superficial reflexes,
and pathologic reflexes such as a Babinski re-sponse occur. Severe leg
spasms can occur as the result of an upper motor neuron lesion; the spasms
result from the preserved reflex arc, which lacks inhibition along the spinal
cord below the level of injury.
There is little or no muscle atrophy, and muscles
remain per-manently tense, exhibiting spastic paralysis or paresis (weakness).
Paralysis associated with upper motor neuron lesions usually af-fects a whole
extremity, both extremities, and an entire half of the body. Hemiplegia
(paralysis of an arm and leg on the same side of the body) can be the result of
an upper motor neuron lesion. If hemorrhage, an embolus, or a thrombus destroys
the fibers from the motor area in the internal capsule, the arm and the leg of
the opposite side become stiff and very weak or paralyzed, and the reflexes are
hyperactive. When both legs are paralyzed, the condition is called paraplegia;
paralysis of all four extremities is quadriple-gia.
Lower Motor Neuron Lesions.
A patient is considered to havelower motor neuron damage if a motor nerve is severed between the muscle and the spinal cord.
The result of lower motor neu-ron damage is muscle
paralysis. Reflexes are lost, and the muscle becomes flaccid (limp) and atrophied from disuse. If the patient has
injured the spinal trunk and it can heal, use of the muscles connected to that
section of the spinal cord may be regained. If the anterior horn motor cells
are destroyed, however, the nerves cannot regenerate and the muscles are never
useful again. Flac-cid paralysis and atrophy of the affected muscles are the
princi-pal signs of lower motor neuron disease. Lower motor neuron lesions can
be the result of trauma, infection (poliomyelitis), tox-ins, vascular
disorders, congenital malformations, degenerative processes, and neoplasms.
Compression of nerve roots by herni-ated intervertebral disks is a common cause
of lower motor neu-ron dysfunction.
Coordination of Movement.
The smoothness, accuracy, andstrength that characterize the muscular
movements of a normal person are attributable to the influence of the
cerebellum and the basal ganglia.
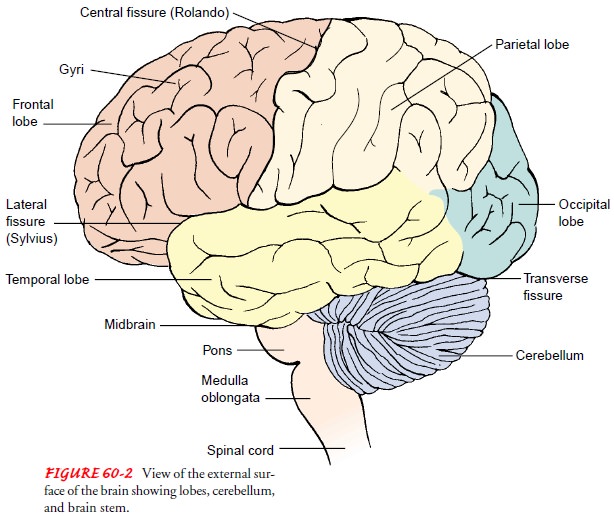
The
cerebellum (refer to Fig. 60-2), described earlier, is located beneath the
occipital lobe of the cerebrum; it is responsible for the coordination,
balance, and timing of all muscular move-ments that originate in the motor
centers of the cerebral cortex. Through the action of the cerebellum, the
contractions of op-posing muscle groups are adjusted in relation to each other
to maximal mechanical advantage; muscle contractions can be sus-tained evenly
at the desired tension and without significant fluc-tuation, and reciprocal
movements can be reproduced at high and constant speed, in stereotyped fashion
and with relatively little effort.
The basal ganglia, masses of gray matter in the
midbrain be-neath the cerebral hemispheres, border the lateral ventricles and
lie in proximity to the internal capsule. The basal ganglia play an important
role in planning and coordinating motor movements and posture. Complex neural
connections link the basal ganglia with the cerebral cortex. The major effect
of these structures is to inhibit unwanted muscular activity; disorders of the
basal ganglia result in exaggerated, uncontrolled movements.
Impaired cerebellar function, which may occur as a
result of an intracranial injury or some type of an expanding mass (eg, a
hemorrhage, abscess, or tumor), results in loss of muscle tone, weakness, and
fatigue. Depending on the area of the brain af-fected, the patient has
different motor symptoms or responses. The patient may demonstrate decorticate,
decerebrate, or flaccid posturing, usually as a result of cerebral trauma
(Bateman, 2001). Decortication (decorticate posturing) is the result of lesions
of the internal capsule or cerebral hemispheres; the patient has flexion and
internal rotation of the arms and wrists and extension, inter-nal rotation, and
plantar flexion of the feet. Decerebration (de-cerebrate posturing), the result
of lesions at the midbrain, is more ominous than decortication. The patient has
extension and ex-ternal rotation of the arms and wrists and extension, plantar
flex-ion, and internal rotation of the feet. Flaccid posturing is usually the
result of lower brain stem dysfunction; the patient has no motor function, is
limp, and lacks motor tone.
Flaccidity
preceded by decerebration in a patient with cerebral injury indicates severe
neurologic impairment, which may herald brain death. However, before the
declaration of brain death, the patient must have spinal cord injury ruled out,
the effects of all neuromuscular paralyzing agents must have worn off, and any
other possible treatable causes of neurologic impairment must be investigated.
Tumors,
infection, or abscess and increased intracranial pres-sure can all affect the
cerebellum. Cerebellar signs, such as ataxia, incoordination, and seizures, as
well as CSF obstruction and com-pression of the brain stem may be seen. Signs
of increased in-tracranial pressure, including vomiting, headache, and changes
in vital signs and level of consciousness, are especially common when CSF flow
is obstructed.
Destruction
or dysfunction of the basal ganglia leads not to paralysis but to muscle
rigidity, with disturbances of posture and movement. Such patients tend to have
involuntary movements. These may take the form of coarse tremors, most often in
the upper extremities, particularly in the distal portions; athetosis, movement
of a slow, squirming, writhing, twisting type; or chorea, marked by spasmodic,
purposeless, irregular, uncoordi-nated motions of the trunk and the
extremities, and facial gri-macing. Disorders due to lesions of the basal
ganglia include Parkinson’s disease, Huntington’s disease, and spasmodic
torticollis.
SENSORY SYSTEM FUNCTION
Integrating Sensory Impulses.
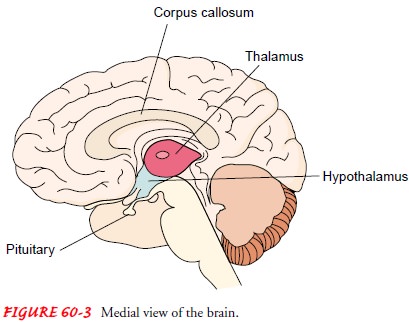
The thalamus, a major receivingand transmitting
center for the afferent sensory nerves, is a large structure connected to the
midbrain. It lies next to the third ven-tricle and forms the floor of the
lateral ventricle (see Fig. 60-3). The thalamus integrates all sensory impulses
except olfaction. It plays a role in the conscious awareness of pain and the
recogni-tion of variation in temperature and touch. The thalamus is
re-sponsible for the sense of movement and position and the ability to
recognize the size, shape, and quality of objects.
Receiving Sensory Impulses.
Afferent impulses travel from theirpoints of origin
to their destinations in the cerebral cortex via the ascending pathways
directly, or they may cross at the level of the spinal cord or in the medulla,
depending on the type of sensation that is registered. Sensory information may
be integrated at the level of the spinal cord or may be relayed to the brain.
Knowledge of these pathways is important for neurologic assessment and for
understanding symptoms and their relationship to various lesions.
Sensory
impulses enter the spinal cord by way of the posterior root. These axons convey
sensations of heat, cold, and pain and enter the posterior gray column of the
cord, where they make connections with the cells of secondary neurons. Pain and
tem-perature fibers cross immediately to the opposite side of the cord and
course upward to the thalamus. Fibers carrying sensations of touch, light
pressure, and localization do not connect immedi-ately with the second neuron
but ascend the cord for a variable distance before entering the gray matter and
completing this con-nection. The axon of the secondary neuron crosses the cord
and proceeds upward to the thalamus.
Position
and vibratory sensation are produced by stimuli aris-ing from muscles, joints,
and bones. These stimuli are conveyed, uncrossed, all the way to the brain stem
by the axon of the pri-mary neuron. In the medulla, synaptic connections are
made with cells of the secondary neurons, whose axons cross to the opposite
side and then proceed to the thalamus.
Sensory Losses.
Destruction of a sensory nerve results in totalloss
of sensation in its area of distribution. Transection of the spinal cord yields
complete anesthesia below the level of injury. Selective destruction or
degeneration of the posterior columns of the spinal cord is responsible for a
loss of position and vibratory sense in segments distal to the lesion, without
loss of touch, pain, or temperature perception. A lesion, such as a cyst, in
the center of the spinal cord causes dissociation of sensation—loss of pain at the
level of the lesion. This occurs because the fibers carrying pain and
temperature cross within the cord immediately on en-tering; thus, any lesion
that divides the cord longitudinally di-vides these fibers. Other sensory
fibers ascend the cord for variable distances, some even to the medulla, before
crossing, thereby by-passing the lesion and avoiding destruction.
Lesions affecting the posterior spinal nerve roots
may cause im-pairment of tactile sensation, including intermittent severe pain
that is referred to their areas of distribution. Tingling of the fingers and
the toes can be a prominent symptom of spinal cord disease, presumably due to
degenerative changes in the sensory fibers that extend to the thalamus (ie,
belonging to the spinothalamic tract).
Related Topics