Chapter: Medical Surgical Nursing: Health Care of the Older Adult
Physical Aspects of Aging
PHYSICAL
ASPECTS OF AGING
Cardiovascular System
Heart disease is the leading cause of death in the aged. The heart valves become thicker and stiffer, and the heart muscle and ar-teries lose their elasticity. Calcium and fat deposits accumulate within arterial walls, and veins become increasingly tortuous. Although function is maintained under normal circumstances, the cardiovascular system has less reserve and responds less effi-ciently to stress. The maximum cardiac output decreases by about 25% from age 20 to age 80. Under conditions of stress, both the maximum cardiac output and the maximum HR di-minish gradually. The relationship between maximum HR and age is as follows:
Normal maximum HR for
age = 220 ŌłÆ age in years
Hypertension has been
shown to be a serious risk factor at all ages for cardiovascular disease and
stroke. A diagnosis of hyper-tension is made only after it has been confirmed
by at least two subsequent readings. In older people, hypertension is
classified as follows:
Isolated systolic
hypertension: the systolic reading exceeds140 mm Hg, and
the diastolic measurement is normal or near normal (less than 90 mm Hg)
Primary hypertension: the diastolic pressure is greater than orequal to 90 mm Hg regardless of
the systolic pressure Secondary
hypertension: hypertension that can be attributed toan underlying cause
Cardiovascular dysfunction may manifest as congestive heart failure,
coronary artery disease, arteriosclerosis, hypertension, in-termittent
claudication (leg pain caused by walking), peripheral vascular disease,
orthostatic hypotension, dysrhythmias, cerebro-vascular accidents (strokes), or
myocardial infarction (heart attack).
Heart failure (HF) is
the number one cause of hospitalization among Medicare recipients and is a
major cause of morbidity and mortality among the elderly population in the
United States. Older patients often present with different symptoms than those
seen in younger patients. Typically, younger persons present for care with the
symptoms of exertional dyspnea, or-thopnea, and peripheral edema, whereas older
patients typically report fatigue, nausea, and abdominal discomfort. In the
younger population, men are more prone to HF, but in the el-derly population
far greater numbers of women develop it. De-pending on its cause, HF can
require various forms of therapy. The current standard of therapy for HF
includes diuretics, angiotensin-converting enzyme inhibitors (ACE inhibitors)
and, digoxin. Several large studies have also indicated that carefully
monitored, low-dose beta-blockers and spironolactone can de-crease mortality
(Rittenhouse, 2001).
Cardiovascular health can be promoted by regular exercise, proper diet,
weight control, regular blood pressure measure-ments, stress management, and
smoking cessation. To avoid light-headedness, fainting, and possible falls caused
by orthostatic hypotension, the older person should be counseled to rise slowly
(from a lying, to a sitting, to a standing position); to avoid strain-ing when
having a bowel movement; and to consider having five or six small meals each
day, rather than three, to minimize the hypotension that can occur after a
large meal. Extremes in tem-perature should be avoided, including hot showers
and whirlpool baths. Yard work should be limited to no more than 20 minutes on
hot summer days. Exposure to wind or cold weather also should be avoided
because of the risk of dizziness or falling asso-ciated with slower adjustments
of blood pressure. If an individ-ual experiences dependent edema as the day
progresses, the use of elastic compression stockings helps to minimize venous
pooling.
Respiratory System
Age-related changes in the respiratory system affect lung capacity and
function and include increased anteroposterior chest diame-ter, osteoporotic
collapse of vertebrae resulting in kyphosis (in-creased convex curvature of the
spine), calcification of the costal cartilages and reduced mobility of the
ribs, diminished efficiency of the respiratory muscles, increased lung
rigidity, and decreased alveolar surface area. Increased rigidity or loss of
elastic recoil in the lung results in increased residual lung volume and
decreased vital capacity. Gas exchange and diffusing capacity are also
di-minished. Decreased cough efficiency, reduced ciliary activity, and
increased respiratory dead space make the older person more vulnerable to
respiratory infections.
Health promotion activities that help elderly persons maintain adequate
respiratory function include regular exercise, appropri-ate fluid intake,
pneumococcal vaccination, yearly influenza im-munizations, and avoidance of
people who are ill. As with people of all ages, smoking cessation and frequent
hand hygiene are pru-dent health practices. Hospitalized older adults should be
fre-quently reminded to cough and take deep breaths, particularly
postoperatively, because their decreased lung capacity and de-creased cough
efficiency predispose them to respiratory infections and atelectasis.
Integumentary System
The functions of the
skin include protection, temperature regu-lation, sensation, and excretion.
With aging, changes occur that affect the function and appearance of the skin.
The epidermis and dermis become thinner. Elastic fibers are reduced in number,
and collagen becomes stiffer. Subcutaneous fat diminishes, particu-larly in the
extremities. Decreased numbers of capillaries in the skin result in diminished
blood supply. These changes cause a loss of resiliency and wrinkling and
sagging of the skin. Hair pig-mentation decreases, resulting in gradual
graying. The skin be-comes drier and susceptible to irritations because of
decreased activity of the sebaceous and sweat glands. These changes in the
integument reduce tolerance to extremes of temperature and to exposure to the
sun.
Strategies to promote
healthy skin function include avoiding exposure to the sun, using a lubricating
skin cream, avoiding long soaks in the tub, and maintaining adequate intake of
water (8 to 10 eight-ounce glasses per day).
Reproductive System
Ovarian production of estrogen and progesterone ceases with menopause.
Changes occurring in the female reproductive sys-tem include thinning of the
vaginal wall, along with a narrowing in size and a loss of elasticity;
decreased vaginal secretions, result-ing in vaginal dryness, itching, and
decreased acidity; involution (atrophy) of the uterus and ovaries; and
decreased pubococcygeal muscle tone, resulting in a relaxed vagina and
perineum. These changes contribute to vaginal bleeding and painful intercourse.
In older men, the penis and testes decrease in size, and levels of
androgens diminish. Erectile dysfunction may develop with concomitant
cardiovascular disease, neurologic disorders, dia-betes, or even respiratory
disease, which limits exercise tolerance.
Sexual desire and activity decline but do not disappear. The use of
water-based lubricants can help prevent painful intercourse. Local estrogen
replacement intravaginally enhances vaginal tissue without the risks and side
effects of oral estrogen. Several modal-ities are available for treatment of
erectile dysfunction, which is linked to cardiovascular, neurologic, endocrine,
or occasionally psychological dysfunction. The use of vacuum penile pumps,
local injection or placement of vasostimulating medication into the ure-thral
opening, and use of an oral medication, sildenafil citrate (Vi-agra), have all
proved effective for some patients. Sildenafil citrate is contraindicated in
patients who are taking oral nitrates.
If significant sexual
dysfunction is present, referral to a gyne-cologist or urologist is warranted.
For both men and women, maintenance of a daily physical exercise routine
promotes en-hanced sexual performance.
Genitourinary System
The genitourinary system continues to function adequately in older
people, although there is a decrease in kidney mass, pri-marily because of a
loss of nephrons. Changes in kidney function include a decreased filtration
rate, diminished tubular function with less efficiency in resorbing and
concentrating the urine, and a slower restoration of acidŌĆōbase balance in
response to stress. Older women often suffer from stress or urge incontinence,
or both. Benign prostatic hyperplasia (enlarged prostate gland), which is a
common finding in older men, causes a gradual in-crease in urine retention and
overflow incontinence. Prostate can-cer, a slow-growing cancer, is most often
seen in men older than
70 years of age. Kidney and bladder cancers are most frequently seen
after the age of 50 years. Smoking is known to be a primary causative agent of
these carcinomas.
Adequate consumption of fluids is important to reduce the risk of
bladder infections and urinary incontinence. Other healthy habits include
having ready access to toilet facilities and voiding every 2 to 3 hours while
awake. Avoidance of bladder-irritating substancesŌĆösuch as caffeinated,
carbonated, and acidic beverages, Nutra-sweet, and alcoholŌĆöwill greatly reduce
urinary urgency and frequency. Water intake should be increased to avoid
concentrated urine, which causes urinary urgency.
Pelvic floor exercises,
first described by Kegel (1948), can also be extremely useful in reducing the
symptoms of stress and urge incontinence. Teaching the patient how to do the
exercises be-gins with identifying the pubococcygeus muscle, which is the same
muscle used to hold back flatus or to voluntarily stop the flow of urine without
contracting the abdomen, buttocks, or inner thigh muscles. The pelvic muscles
are first tightened and then relaxed, maintaining a 5-second contraction with
10-second rest intervals. This exercise should be routinely practiced for 30 to
80 repetitions each day; additional repetitions are discouraged because of the
risk of fatigue of the muscle. Because achieving bet-ter muscle control takes
at least several months to accomplish, the elderly person is encouraged to
consistently perform the exercises. To maintain pubococcygeus muscle control,
these daily exercises must continue indefinitely. The use of biofeedback to
confirm the correct execution of these exercises increases their effective-ness
significantly.
As menopause approaches,
a womanŌĆÖs circulating estrogen de-creases, and, as a result, the pelvic floor
is deprived of its needed blood supply and nutrients. This causes increasing
stress and urge incontinence. Through the use of biofeedback-assisted pelvic
muscle exercise, an individual can successfully regain bladder function. These
exercises are also recommended for men with dribbling incontinence related to
prostatectomy. The nurse in-structs the patient to tighten the rectal sphincter
until the penis and testes slightly lift. Frequent repetition produces the
desired muscle tone.
Constipation can be a
major factor contributing to urinary in-continence. The patient is encouraged
to eat a high-fiber diet, drink adequate fluids, and increase mobility to
promote regular bowel function.
Urinary tract infections are prevalent in older women. The reasons
include the effects of decreased estrogen, which shortens the urethral length,
allowing easier passage of bacteria into the bladder; less overall fluid
consumption, which causes a concen-trated urine in which bacteria can
proliferate; and the introduc-tion of bacteria from the rectum as a result of
poor bathroom hygiene secondary to impaired mobility and joint changes.
Lim-ited range of motion of the arm and limited hand dexterity often result in
a womanŌĆÖs cleansing the perineal area in a back-to-front motion, causing
bacteria such as Escherichia coli to
be introduced to the urethral meatus and thus into the bladder (Degler, 2000b).
Gastrointestinal System
The older adult is at increased risk for impaired nutrition. Peri-odontal disease leading to tooth decay and loss of teeth is com-mon. Salivary flow diminishes, and the older person may experience a dry mouth. A preference for sweet and salty foods results from a decrease of taste receptors. Major complaints often center on feelings of fullness, heartburn, and indigestion. Gastric motility may decrease, resulting in delayed emptying of stomach contents.
Diminished secretion of acid and pepsin reduces the absorption of iron,
calcium, and vitamin B12. Absorption of nutrients in the small intestine also appears to
diminish with age. The function of the liver, gallbladder, and pancreas is
generally maintained, although absorption and tolerance to fat may decrease.
The inci-dence of gallstones and common bile duct stones increases
pro-gressively with advancing years.
Difficulty in swallowing, or dysphagia, affects 1 in 17 people,
including 6.2 million Americans over the age of 60 years, with 300,000 to
600,000 new cases diagnosed each year. It is a serious condition that can be
life-threatening. It results from interrup-tion or dysfunction of neural
pathways, such as can occur with stroke. It may also develop from dysfunction
of the striated and smooth muscles of the gastrointestinal tract in up to 50%
of pa-tients with ParkinsonŌĆÖs disease and in those with conditions such as
multiple sclerosis, poliomyelitis, and amyotrophic lateral scle-rosis (Lou
GehrigŌĆÖs disease). Aspiration of food or fluid is the most serious complication
and can occur in the absence of cough-ing or choking (Galvan, 2001).
Constipation is common
in aged people. When mild, the symptoms involve abdominal discomfort and
flatulence, but more serious consequences include fecal impaction that
contributes to diarrhea around the impaction, fecal incontinence, and
obstruc-tion. Predisposing factors for constipation include lack of dietary
bulk, prolonged use of laxatives, the use of some medications, inactivity,
insufficient fluid intake, and excessive dietary fat. Another factor may be
ignoring the urge to defecate.
Gastrointestinal health
promotion practices include receiving regular dental care; eating small,
frequent meals; avoiding heavy activity after eating; eating a high-fiber,
low-fat diet; ingesting an adequate amount of fluids; establishing regular
bowel habits; and avoiding the use of laxatives and antacids. Understanding
that there is a direct correlation between loss of smell and taste per-ception
and food intake helps caregivers to intervene to maintain elderly patientsŌĆÖ
health.
Nutritional Health
The social, psychological, and physiologic functions of eating
in-fluence the dietary habits of the aged person. Decreased physical activity
and a slower metabolic rate reduce the number of calo-ries needed by the older
adult to maintain an ideal weight. Apathy, immobility, depression, loneliness,
poverty, inadequate knowl-edge, lack of oral health, and lack of taste
discrimination also con-tribute to suboptimal nutrient intake. Budgetary
constraints and physical limitations may impair food shopping and meal
prepa-ration. Education regarding healthy versus ŌĆ£empty-calorieŌĆØ foods is
helpful.
Health promotion teaching includes encouraging a diet that is low in
sodium and saturated fats and high in vegetables, fruits, and fish. The older
adult requires a variety of foods to maintain balanced nutrition. No more than
20% to 25% of dietary calo-ries should be consumed as fat. Reducing salt intake
is also advo-cated, because sodium reduction has been shown to correct
hypertension in some people. Protein intake should remain the same in later
adulthood as in earlier years. Carbohydrates, a major source of energy, should
supply the diet with 55% to 60% of the daily calories. Simple sugars should be
avoided and complex car-bohydrates encouraged. Potatoes, whole grains, brown
rice, and fruit provide the person with minerals, vitamins, and fiber and
should be encouraged. Drinking 8 to 10 eight-ounce glasses of water per day is
recommended unless contraindicated by a medical condition. A multivitamin each day helps
to maintain daily nutritional needs.
Sleep
Sleep disturbances frequently occur in older people, affecting more than
50% of adults 65 years of age or older. The elderly often experience variations
in their normal sleepŌĆōwake cycles, and the lack of quality sleep at night often
creates the need for napping during the day. Laboratory screening can help to
rule out disease processes that might be affecting an older personŌĆÖs ability to
sleep at night. If a spouse notes excessive snoring, a sleep study is
indi-cated to rule out sleep apnea. The nurse can recommend prudent sleep
hygiene behaviors such as avoiding daytime napping, eating a light snack before
bedtime, and decreasing the overall time in bed to adjust for the fewer hours
of sleep needed than when the patient was younger (Grandjean & Gibbons,
2000).
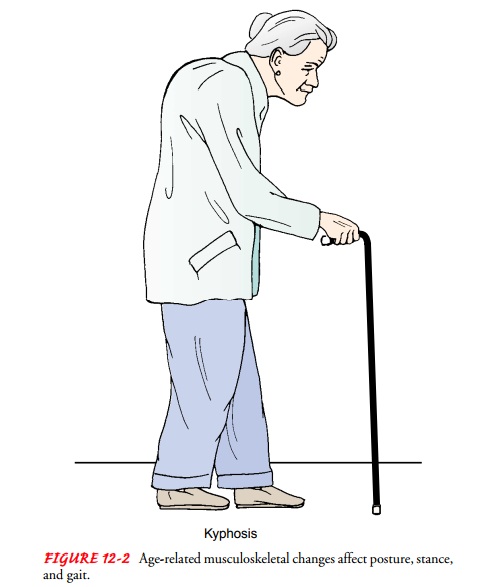
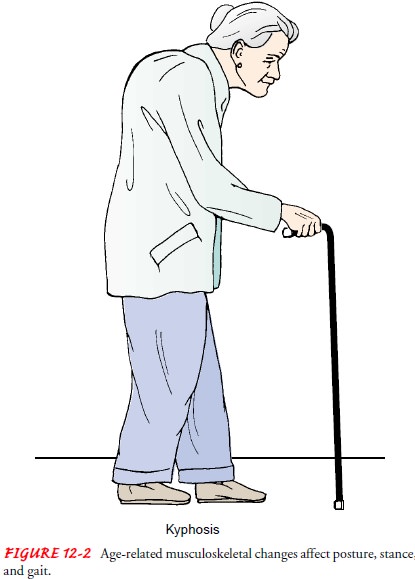
Musculoskeletal System
A gradual, progressive decrease in bone mass begins before the age of 40
years. Excessive loss of bone density results in osteoporosis, which affects
both older men and women but is most prevalent in postmenopausal women. It is
also seen in older men who are receiving hormone treatments for prostate
cancer. A higher inci-dence is found among northern Europeans and Asians. Its
typi-cal form is associated with inactivity, inadequate calcium intake, loss of
estrogens, and a history of cigarette smoking. The danger of fracture as a
result of bone reabsorption is especially high for the dorsal portion of the
vertebra, humerus, radius, femur, and tibia. A loss of height occurs in later
life as a result of osteoporotic changes of the spine, kyphosis (excessive
convex curvature of the spine), and flexion of the hips and knees. These
changes negatively affect mobility, balance, and internal organ function (Fig.
12-2).
The muscles diminish in
size and lose strength, flexibility, and endurance with decreased activity and
advanced age. Back pain is common. Beginning in middle age, the cartilage of
joints pro-gressively deteriorates. Degenerative joint disease is found in
everyone past the age of 70 years.
Calcium supplements,
vitamin D, fluoride, estrogens, and weight-bearing exercises are often
prescribed for the person who is at high risk for or already has osteoporosis.
Although osteo-porosis cannot be reversed, the disease process can be slowed. A
bone density test is the gold standard to assess for osteoporosis. Once it is
diagnosed and treatment begun, yearly follow-up de-terminations of the bone
density level are indicated. For skeletal health, the nurse can recommend the following
(Scheiber & Torregrosa, 2000):
ŌĆó
A high calcium intake, 1500 mg/day. Dairy products
and dark green vegetables are excellent sources, as are soups and broths made
with a soup bone and cooked with added vine-gar to leach calcium from the bone.
Calcium supplements can be recommended to ensure that the daily calcium in-take
is adequate.
ŌĆó
A low-phosphorus diet. A calcium-to-phosphorus
ratio of 1:1 is ideal; red meats, cola drinks, and processed foods that are low
in calcium and high in phosphorus are avoided.
ŌĆó
Weight-bearing exercise. The pull of muscle
insertions on the long bones strengthens the muscles and retards calcium
resorption.
ŌĆó
Reduction of caffeine and alcohol. This assists in
stopping further demineralization and renal excretion of calcium.
ŌĆó
Smoking cessation.
ŌĆó
Selective estrogen receptor modulators, such as
raloxifene (Evista), preserve bone mineral density without estrogenic effects
on the uterus. This medication is indicated for both prevention and treatment
of osteoporosis. Although hor-mone replacement therapy (HRT) has been the
mainstay of therapy for perimenopausal women, recent studies have demonstrated
greater risks than previously recognized (Chen, Weiss, Newcomb, Barlow &
White, 2002).
ŌĆó
The bisphosphate drugs (e.g., Fosamax, Actonel).
These drugs bind to mineralized bone surfaces to inhibit osteo-clastic activity
and promote bone formation.
Muscle strength and flexibility can be enhanced with a pro-gram of
regular exercise. The axiom ŌĆ£use it or lose itŌĆØ is very rel-evant when
considering the physical capacity of aged people. The nurse plays an important
role by encouraging older adults to participate in a regular exercise program.
Regular exercise in-creases the strength and efficiency of heart contractions,
im-proves oxygen uptake by cardiac and skeletal muscles, reduces fatigue,
increases energy, and reduces cardiovascular risk factors. Muscle endurance,
strength, and flexibilityŌĆöall outcomes of regular exerciseŌĆöalso help to promote
independence and psy-chological well-being. Aerobic exercises are the
foundation of programs of cardiovascular endurance conditioning. A physical
examination by a physician or nurse practitioner is necessary be-fore
initiating an exercise program, and older persons should perform exercises in
moderation and use short rests to avoid undue fatigue. Swimming and brisk
walking are often recom-mended because they are managed easily and usually are
enjoyed by the older person.
Information about the nature and time course of menopause-associated bone
loss through early markers may be used to help to preserve bone and thus stop
the natural sequelae of osteoporosis. A nurse-led research team used frequent
sequential serum mark-ers to confirm these changes and found a correlation with
elevated alkaline phosphatase (ALP) and concentrations of follicle-stimulating
hormone as a marker for vitamin K status. Therefore, perimenopausal women with
elevated ALP can be targeted for health promotion to preserve bone density
(Lukacs, 2000).
Nervous System
The structure and function of the nervous system change with ad-vanced
age, and a reduction in cerebral blood flow accompanies nervous system changes.
The loss of nerve cells contributes to a progressive loss of brain mass, and
the synthesis and metabolism of the major neurotransmitters are also reduced.
Because nerve impulses are conducted more slowly, older people take longer to
respond and react. The autonomic nervous system performs less efficiently, and
postural hypotension, which causes the person to lose consciousness or feel
lightheaded on standing up quickly, may occur. Cerebral ischemia with related
lightheadedness may interfere with mobility and safety. The nurse advises the
person to allow a longer time to respond to a stimulus and to move more deliberately.
Homeostasis is more difficult to maintain, but in the absence of pathologic
changes, the older person functions ade-quately and retains cognitive and
intellectual abilities.
Mental function is
threatened by physical or emotional stresses. A sudden onset of confusion may
be the first symptom of an in-fection or change in physical condition
(pneumonia, urinary tract infection, medication interactions, dehydration, and others).
A slowed reaction time
places the older person at risk for falls and injuries, including driving
errors. Compared with the per-mile fatality rate for drivers aged 25 to 69
years, that for drivers 70 years of age and older is nine times as high. When
an elderly person has been witnessed driving unsafely, he or she should re-ceive
a driving fitness evaluation; this is often administered by an occupational
therapist in conjunction with a neuropsychologist, who can help with the more
detailed cognitive testing (Dolinar, McQuillen, & Ranseen, 2001).
Sensory System
Sensory losses with old
age affect all sensory organs and can be devastating to the person who cannot
see to read or watch televi-sion, hear conversation well enough to communicate,
or dis-criminate taste well enough to enjoy food.
SENSORY LOSSES VERSUS SENSORY DEPRIVATION
Sensory losses can often be helped by assistive devices such as glasses
and hearing aids. In contrast, sensory deprivation is the ab-sence of stimuli
in the environment or the inability to interpret existing stimuli (perhaps as a
result of a sensory loss). This depri-vation can lead to boredom, confusion,
irritability, disorienta-tion, and anxiety. Meaningful sensory stimulation
offered to the older person is often helpful in correcting this problem. One
sense can substitute for another in observing and interpreting stimuli. The
nurse can enhance sensory stimulation in the envi-ronment with colors,
pictures, textures, tastes, smells, and sounds. The stimuli are most meaningful
if they are interpreted to the older person and if they are changed often.
Cognitively impaired persons respond well to touch and to familiar music.
VISION
As new cells form on the
outside surface of the lens of the eye, the older central cells accumulate and
become yellow, rigid, dense, and cloudy, leaving only the outer portion of the
lens elas-tic enough to change shape (accommodate) and focus at near and far
distances. As the lens becomes less flexible, the near point of focus gets
farther away. This condition, presbyopia,
usually begins in the fifth decade of life, and requires the wearing of reading
glasses to magnify objects. In addition, the yellowing, cloudy lens causes
light to scatter and makes the older person sensitive to glare. The ability to
discern blue from green de-creases. The pupil dilates slowly and less
completely because of increased stiffness of the muscles of the iris, so the
older person takes longer to adjust when going to and from light and dark
en-vironments or settings and needs brighter light for close vision. Although
pathologic visual conditions are not part of normal aging, the incidence of eye
disease (most commonly cataracts, glaucoma, diabetic retinopathy, and
age-related macular degen-eration) increases in older people.
Age-related macular degeneration, in its most severe forms, is the most
common cause of blindness in adults older than 55 years of age in the United
States, and it is estimated to affect more than 10 million Americans. Risk
factors include sunlight exposure, cig-arette smoking, and heredity, and people
with fair skin and blue eyes are much more prone to the disease. Sunglasses and
hats with visors provide some protection. Yearly eye checkups ensure early
detection, which makes surgical correction much more success-ful. Optical aids
to magnify print and printed objects may help those already suffering from the
effects of macular degeneration to continue to read (Friberg, 2000).
HEARING
Presbycusis, a loss of the ability to hear
high-frequency tones at-tributed to irreversible inner ear changes, occurs in
midlife. Older people are often unable to follow conversation because tones of
high-frequency consonants (letters f, s, th, ch, sh, b, t, p) all sound alike.
Hearing loss may cause the older person to re-spond inappropriately,
misunderstand conversation, and avoid social interaction. This behavior may be
erroneously interpreted as confusion. Wax buildup or other correctable problems
may also be responsible for major hearing difficulties. A properly pre-scribed
and fitted hearing aid may be useful in reducing hearing deficits.
TASTE AND SMELL
Of the four basic tastes
(sweet, sour, salty, and bitter), sweet tastes are particularly dulled in older
people. Blunted taste may con-tribute to the preference for salty, highly
seasoned foods, but herbs, onions, garlic, and lemon should be encouraged as
substi-tutes for salt to flavor food.
Related Topics