Chapter: Medical Surgical Nursing: Health Care of the Older Adult
Common Mental Health Problems in Older Populations
Common Mental Health Problems in Older Populations
Older adults are less likely than younger people to seek treatmentfor
mental health symptoms, so health professionals are challenged to recognize,
assess, refer, collaborate, treat, and support those older adults who exhibit
noticeable changes in intellect or affect. In a community setting, the nurse
may be the only health care provider who has contact with the person. Symptoms
should not be dismissed as age-related changes; a thorough assessment may
reveal a treatable, reversible physical or mental condition.
DEPRESSION
Depression is the most common affective or mood disorder ofold age and is often
responsive to treatment. Its classification and diagnosis vary according to the
number, severity, and duration of symptoms. Depression disrupts quality of
life, increases the risk of suicide, and becomes self-perpetuating. It may also
be an early sign of a chronic illness or the result of physical illness. Signs
of depression include feelings of sadness, fatigue, dimin-ished memory and
concentration, feelings of guilt or worthless-ness, sleep disturbances,
appetite disturbances with excessive weight loss or gain, restlessness,
impaired attention span, and suicidal ideation.
Although depression among the elderly is widespread, it is often
undiagnosed and untreated. Attentive clinical evaluation is essential.
Geriatric depression and symptoms of dementia often overlap, so cognitive
impairment may be a result of depression rather than dementia. When depression
and medical illnesses co-exist, as they often do, neglect of the depression can
retard phys-ical recovery. Symptoms might be secondary to a medication
interaction or an undiagnosed physical condition. Assessing the patient’s
mental status, including assessing for depression, is vital and must not be
overlooked (Charts 12-3 and 12-4).
Depressive illness in late life should be vigorously treated with
antidepressants. Psychosocial approaches have also been found to be effective.
Selective serotonin reuptake inhibitors, such as paroxetine (Paxil), are
clinically useful and exhibit rapid action with a low occurrence of adverse
effects. Tricyclic antidepres-sants, specifically nortriptyline (Aventyl),
desipramine (Nor-pramin), and doxepin (Sinequan), are also clinically effective
for depression. Anticholinergic, cardiac, and orthostatic side effects, as well
as interactions with other medications, require that these agents be used with
care: the dosage must be managed carefully to relieve symptoms and at the same
time avoid medication tox-icity. It may take 4 to 6 weeks for symptoms to
recede, so thenurse should offer explanations and encouragement during this
period.
Alcohol abuse related to depression is significant in the elderly
population. Alcohol-related problems in older people often re-main hidden,
however, since many older adults deny their habit when questioned. Alcohol
abuse is especially dangerous in the older person because of changes in renal
and liver function as well as the probability of side effects in interactions
with prescriptive medications (Adams, Atkinson, Ganz, & O’Conner, 2000).
DELIRIUM
Delirium, often called acute confusional state, begins with con-fusion and
progresses to disorientation. The patient may experi-ence an altered level of
consciousness ranging from stupor to excessive activity. Thinking is
disorganized, and the attention span is characteristically short.
Hallucinations, delusions, fear, anxiety, and paranoia may also be evident.
Because of the acute and unexpected onset of symptoms and the unknown
under-lying cause, delirium is a medical emergency. Delirium occurs secondary
to a number of causes, including physical illness, med-ication or alcohol
toxicity, dehydration, fecal impaction, mal-nutrition, infection, head trauma,
lack of environmental cues, and sensory deprivation or overload. Older adults
are particularly vulnerable to acute confusion because of their decreased
biologic reserve and the large number of medications that many take. The nurse
must recognize the grave implications of the acute symp-toms and report them
immediately. If the delirium goes unrec-ognized and the underlying cause is not
treated, permanent, irreversible brain damage or death can follow. Delirium is
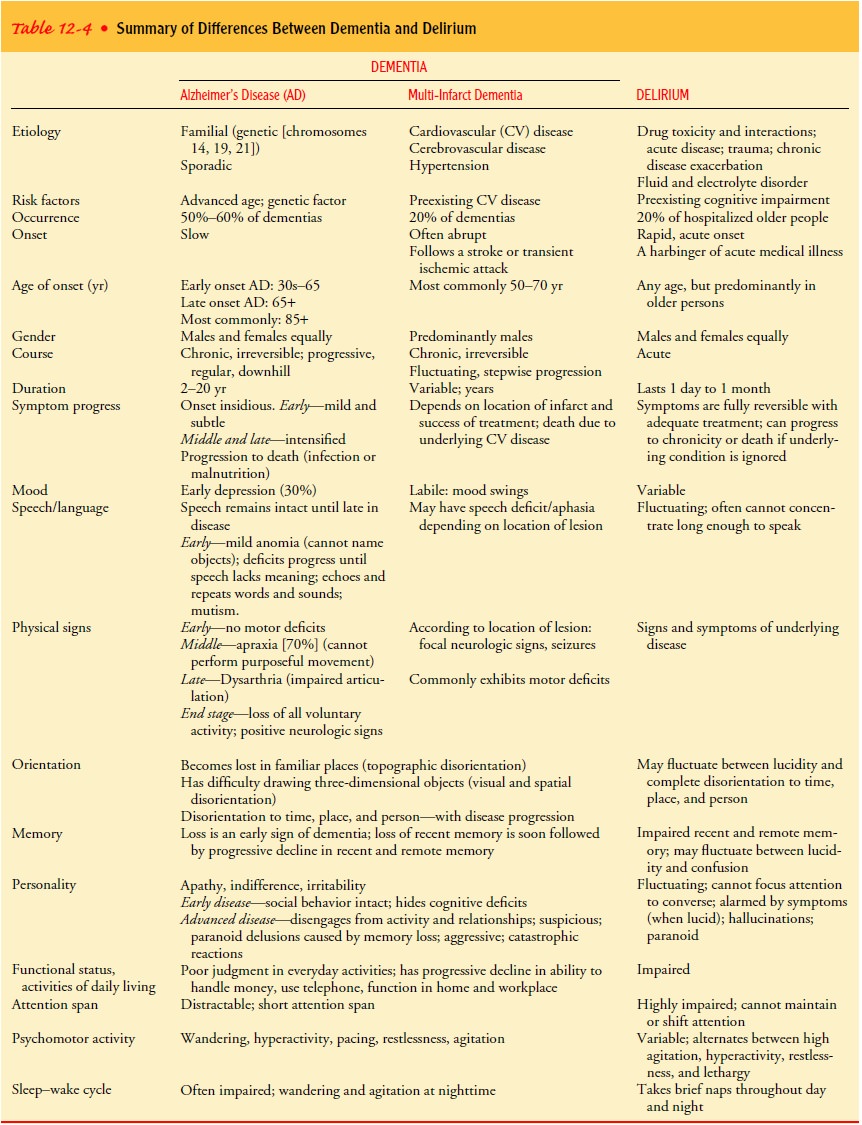
some-times mistaken for dementia (see Table 12-4 for a comparison of dementia
and delirium).
Therapeutic interventions vary, depending on the reason for the
symptoms. Because medication interactions and toxicity are often implicated,
nonessential medications should be stopped. Nutritional and fluid intake should
be supervised and monitored. The environment should be quiet and calm. To
increase orien-tation and provide
familiar environmental cues, the nurse en-courages family members or friends to
touch and talk to the patient. It is important to question the family carefully
about the patient’s prior cognitive state. Ongoing mental status assessments
using this baseline are helpful in evaluating responses to treat-ment and to
the hospital or extended care facility admission.
THE DEMENTIAS: MULTI-INFARCT DEMENTIA AND ALZHEIMER’S DISEASE
Dementia reportedly affects 3% to 11% of community-residingadults older than 65
years of age and 20% to 50% of community-residing adults older than age 85.
Most of those suffering from dementia who are in the over-85 age group reside
in institutional settings. Of those individuals 100 years and older, almost 60%
are noted to demonstrate dementia. Despite this high incidence, clinicians fail
to detect dementia in 21% to 72% of patients. In order for a diagnosis of
dementia to be made, at least two domains of altered function must exist—memory
and at least one of the following: language, perception, visuospatial function,
calcula-tion, judgment, abstraction, and problem-solving (Mayo Foun-dation for
Medical Education and Research [Mayo], 2001).
Symptoms are usually subtle in onset and often progress slowly until
they are obvious and devastating. The changes char-acteristic of dementia fall
into three general categories: cognitive, functional, and behavioral.
Reversible causes of dementia include alcohol abuse, medication use
(polypharmacy), psychiatric disor-ders, and normal-pressure hydrocephalus. The
three most com-mon nonreversible dementias are Alzheimer’s disease,
multi-infarct dementia, and mixed Alzheimer’s and multi-infarct dementia.
Alzheimer’s disease accounts for more than 60% of all dementias, and
multi-infarct dementia (vascular dementia) accounts for another 5% to 20%.
Other non-Alzheimer’s dementias include Parkinson’s disease, AIDS-related
dementia, and Pick’s disease. These remaining dementias account for fewer than
15% of cases and are relatively uncommon (National Institute of Neurologi-cal
Disorders and Stroke, 2000).
Dementia is
characterized by an uneven, downward decline in mental function. Multi-infarct
dementia is sometimes confused with Alzheimer’s disease, paranoia, or delirium
because of its un-predictable clinical course. The diagnosis can be even more
diffi-cult if the patient is suffering from both Alzheimer’s disease and
multi-infarct dementia.
Multi-infarct, or
vascular dementia, has the following defin-ing characteristics:
·
There must be evidence of dementia.
·
There must be evidence of cerebrovascular disease
(by his-tory, clinical examination, or brain imaging).
·
The two disorders must be reasonably related.
Alzheimer’s disease is a progressive, irreversible, degenerative neurologic disease that begins insidiously and is characterized by gradual losses of cognitive function and disturbances in be-havior and affect. Alzheimer’s disease is not found exclusively in the elderly; in 1% to 10% of cases, its onset occurs in middle age. A family history of Alzheimer’s disease and the presence of Down syndrome are two established risk factors for Alzheimer’s disease. If family members have at least one other relative with Alzheimer’s disease, then a familial component, which non specifically includes both environmental triggers and genetic determinants, is said to exist. Genetic studies show that autosomal-dominant forms of Alzheimer’s disease are associated with early onset and early death.
In 1987, chromosome 21 was first implicated in early-onset fa-milial
Alzheimer’s disease. Soon after, the gene coding for amyloid precursor protein
(APP) was also found to be on
chromosome 21. Not until 1991 was an actual mutation in association with
famil-ial Alzheimer’s disease found in the APP
gene of chromosome 21. For those with this gene, onset of Alzheimer’s disease
began in their 50s. Only a few of the cases of familial Alzheimer’s disease
have been found to involve this genetic mutation. In 1992, chromosome 14 was
found to contain an unidentified mutation also linked to familial Alzheimer’s
disease. Since 1995, molecular biologists have been discovering even
more-specific genetic information about the various forms of Alzheimer’s
disease, including genetic differences between early- and late-onset
Alzheimer’s disease. These genetic differences are helping to pinpoint risk
factors associated with the disease, although the genetic indicators are not
specific enough to be used as reliable diagnostic markers (Mayo, 2001).
Related Topics