Chapter: Medical Surgical Nursing: Health Care of the Older Adult
Environmental Aspects of Aging
ENVIRONMENTAL
ASPECTS OF AGING
About 95% of the elderly
live in the community, and 75% own their homes. In 1991, about 31% of elderly
persons were living alone (79% of these were women). In the 65 years and older
age group, half as many women as men were married and living with their
spouses: 40% of women compared with 74% of men. About 48% of the women older
than 65 years of age were wid-owed, compared with only 15% of the men. This
difference in marital status is a result of several factors: women have a
longer life expectancy than men do, women tend to marry older men, and women
tend to remain widowed, whereas men often remarry (U.S. Bureau of the Census,
2000).
Living Arrangement Options
Ideally, older persons do best in their own, familiar environment. But
adjustments to the environment may be required to allow the older adult to
remain in his or her own home or apartment. Sometimes, in order to enable them
to remain in their own home, an older adult or couple seek out family members
who might be willing to live in the home, or agree to board someone in
ex-change for completion of household chores.
Sometimes older adults or couples agree to move in with adult children.
This can be a rewarding experience as the children, their parents, and the
grandchildren interact and share household re-sponsibilities. It can also be
stressful, depending on the family dy-namics. Adult children and their older
parents may also choose to pool their financial resources by moving into a
house that has an attached “in-law suite.” This arrangement provides security
for the older adult along with privacy for both families.
Continuing Care Retirement Communities (CCRCs), are be-coming more
popular as the first of the baby boomers enter their retirement years. CCRCs
are retirement communities consisting of single-dwelling houses or apartments
for those individuals who are still able to manage all of their day-to-day
needs, assisted liv-ing apartments for those who need limited assistance with
their daily living needs, and skilled nursing services when continuous nursing
assistance is required. These communities usually con-tract for a large down
payment before the resident moves into the community. This payment allows the
individual or couple the option to reside in the community from the time of
total inde-pendence through the need for assisted or skilled nursing care. This
concept allows for decisions about living arrangements and health care to be
made before any decline in health status occurs. A CCRC also provides
continuity at a time in an older adult’s life when many other factors, such as
health status, income, and avail-ability of friends and family members, may be
changing.
Assisted living facilities are an option when physical or cogni-tive
changes require at least minimal supervision. Assisted living allows for a
degree of independence while providing minimal nursing assistance (eg,
administration of medication and coordi-nation of scheduled and acute care
medical assistance). Other ser-vices, such as laundry, cleaning, and meals, may
also be included.
Skilled nursing facilities offer continuous nursing care. Usu-ally, if
an older adult suffers a major health event such as a stroke, myocardial
infarction, or cancer and is hospitalized, Medicare will cover the cost of the
first 30 to 90 days in a skilled nursing facility if ongoing therapy is needed.
The stipulation for contin-ued Medicare coverage during this time is
documentation of per-sistent improvement in the required therapies, which most
often include physical therapy, occupational therapy, respiratory ther-apy, and
cognitive therapy. Some individuals choose to have nursing home insurance as a
means of paying, at least in part, for the cost of these services, should they
become necessary. When an individual’s financial resources become exhausted as
a result of prolonged nursing home care, the family, the institution, or both
may apply for Medicaid reimbursement. An increasing number of skilled nursing
facilities offer subacute care. This area of the fa-cility offers a high level
of nursing care and may either prevent the need for an individual to be
transferred to a hospital setting or allow a hospitalized individual to be
transferred back to the fa-cility sooner.
Life Care Plans
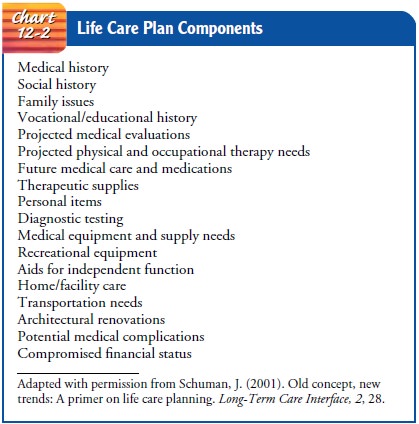
A life care plan is an individualized document that assesses and
eval-uates a client’s present and future health care and living needs. The
typical components of a life care plan are listed in Chart 12-2. Life care
plans were originally developed in 1981 as standardized, ef-ficient guidelines
for medical and ancillary quality-of-life services. A life care plan provides
valuable information regarding factors that can radically affect the
individual’s health care and quality of life. A life care plan is often
requested for individuals with cata-strophic injuries or illness (eg, traumatic
brain injury, amputa-tion, multiple sclerosis) who will require ongoing
rehabilitative
A life care plan may also serve as the blue-print
for what will be expected in long-term care. These plans provide a guideline of
anticipated patient care needs for families, insurance companies, attorneys,
discharge planners, case managers, and all medical and nursing professionals.
The cost of the life care plan varies, depending on the planner, the severity
of the injury or illness, and who is paying for the service, but the average
cost is currently between $5,000 and $20,000 (Schuman, 2001).
The Role of the Family
Planning for care and understanding the psychosocial issues confronting
the older person must be accomplished within the context of the family. If
dependency needs occur, the spouse often assumes the role of primary caregiver.
In the absence of the surviving spouse, an adult child usually assumes
caregiver responsibilities and may eventually need help in providing care and
support. Two common myths in American society are that adult children and their
aged parents are socially alienated and that adult children abandon their
parents when health and other dependency problems arise. Extensive research
refutes both of these beliefs. The family is an important source of sup-port
for older people (Fig. 12-3). Approximately 81% of elderly persons have living
children. Of those elders living alone, two thirds have at least one child
living within 30 minutes of their home, and 62% see at least one adult child
weekly (U.S. Bureau of the Census, 2000).

Social attitudes and
cultural values often dictate that adult children should provide services and
financial support and as-sume the burden of care if their aged parents are
unable to care for themselves. Illness creates special problems for people who
live alone. If community agencies or adult children are unable to pro-vide
care, elders are at high risk for institutionalization.
Regardless of the amount of responsibility and love an adult child exhibits toward dependent elderly parents, strains do de-velop if care continues for a long period. Research exploring the relationship between aged parents and their adult children shows that the quality of the parent–child relationship declines with the poor health of the parent. Under certain circumstances of high risk, strains in intergenerational relationships can result in elder abuse (Hoban & Kearney, 2000; Phillips, 2000; Tumolo, 2000).
Elder abuse is an active
or passive act or behavior that is harm-ful to the elderly person. Such behavior
includes physical vio-lence, personal neglect, financial exploitation,
violation of rights, denial of health care, and self-inflicted abuse.
Preventive action should be taken when strains are evident, before elder abuse
oc-curs. Interdisciplinary team members can be enlisted to help the caregiver
develop self-awareness, increased insight, and an un-derstanding of the aging
process. At the same time, community resources may be useful for both the aged
person and the care-giver (Geldmacher, Heck, & O’Toole, 2001).
Community Support Services
Many community supports
exist that help the older person main-tain independence. Informal sources of
help, such as family, friends, the mail carrier, church members, and neighbors,
can all keep an informal watch. Area Agencies on Aging perform many community
services, including telephone reassurance, friendly visitors, home repair
services, and home-delivered meals. Home-maker and chore services can be
obtained at an hourly rate through these agencies or through local community
nursing ser-vices. If a person is unable to pay, these services may be
subsidized through local and state funds.
Other community support
services are available to help the older person outside the home. Senior
centers have social and health promotion activities, and some provide a
nutritious noon-time meal. Adult day care facilities offer daily nursing care
and social opportunities; these services also enable family members to carry on
daily activities while the older person is at the day care center.
Home Health Care
Home care is often used as a means to prevent hospitalization for frail,
elderly outpatients or to shorten a hospital stay. It can also be used as a
high-tech substitute for hospitalization and can include the use of intravenous
therapy and other therapies previously de-livered in the acute care setting.
Home health care was the area of U.S. health care that saw the most rapid rate
of growth in the 1990s, and by the end of the 1990s it had come to represent
almost one tenth of the total Medicare budget. Rather than viewing home health
care as a means of controlling health care costs, the Federal government’s
Centers for Medicaid and Medicare Services (CMS), formerly the Health Care
Financing Administration (HCFA), de-vised plans to limit the growth of home
health care services. The first system put into place to accomplish decreased
allocations for home health was called the Prospective Payment System (PPS) for
home care, implemented in 2000. Later came a means of quanti-fying needed home care,
called the Outcome and Assessment In-formation Set (OASIS). The OASIS rates
individual consumers of home health care in terms of their ability to perform
activities of daily living (ADLs) and instrumental activities of daily living
(IADLs). Nursing care and rehabilitation services requiring the ex-pertise of a
registered nurse and other health professionals were tra-ditionally paid for by
Medicare. With the advent of the PPS, limits on reimbursement may mean
consideration of alternative means of reimbursement for such services,
including private pay and health insurance products (HCFA, 2000; Plotkin &
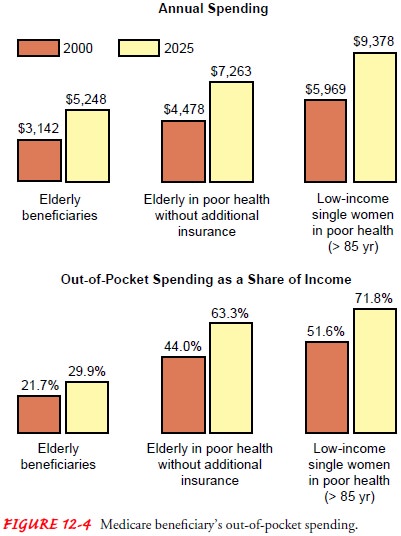
Roche, 2000; Nus baum, 2000). Figure 12-4 shows the estimated growth in
Medicare and out-of-pocket annual spending between 2000 and 2025.
Safety and Comfort in the Home Environment
Injuries rank seventh as a cause of death for older people. The nurse
can encourage lifestyle and environmental changes that older adults and their
families can adopt. Adequate lighting with mini-mal glare and shadow can be
achieved through the use of small area lamps, indirect lighting, sheer curtains
to diffuse direct sunlight, dull rather than shiny surfaces, and nightlights.
Sharply contrast-ing colors can be used to mark the edges of stairs. Grab bars
by the tub and toilet are useful. Loose clothing, improperly fitting shoes,
scatter rugs, small objects, and pets create hazards and increase the risk of
falls. A person functions best in familiar settings if furniture and objects
remain as unchanged as is safely possible.
Hospice Services
Hospice services are a dignified alternative to the chaos of the acute
care setting when a patient with an end-stage disease is not ex-pected to live
long. Hospice is a program of supportive and pal-liative services for dying
patients and their families that includes physical, psychological, social, and
spiritual dimensions of care. Under Medicare and Medicaid, all needed medical
and nursing services are provided to keep the patient as pain free and
comfort-able as possible. The family must agree to assist in the care of the
patient, and services are brought into the home as needed. Hos-pice services
may also be incorporated into the care of residents in long-term care
facilities and include care for end-stage dementia.
Hospice services that are provided in a person’s home also are rated via the OASIS system. Although this system can be very cumbersome and time-consuming in hospice care because of the many care providers involved, it can serve as an excellent tool with which nurses can assess the effects of particular services on specific patient outcomes (Plotkin & Roche, 2000).
Home care and hospice nurses are in a unique position to fa-cilitate
early discussions about a patient’s wishes and goals at the end of life. Too often,
discussion regarding end-of-life care is postponed until a crisis situation
occurs, making it difficult or im-possible for the patient to be an active
participant in the discus-sion. Home health nurses can assist the patient and
family with identifying available options and initiating conversation about
preparing an end-of-life plan (Norlander & McSteen, 2000).
Related Topics