Chapter: Medical Surgical Nursing: Health Care of the Older Adult
Pharmacologic Aspects of Aging
PHARMACOLOGIC
ASPECTS OF AGING
Older people use more medications than does any other age group:
although they comprise only 12.6% of the total popula-tion, they use 30% of all
prescribed medications and 40% of all over-the-counter medications. Medications
have improved the health and well-being of older people by alleviating symptoms
of discomfort, treating chronic illnesses, and curing infectious pro-cesses.
Problems commonly occur, however, because of medication interactions, multiple
medication effects, multiple medication use (polypharmacy), and noncompliance. Combinations of pre-scription
medications and some over-the-counter medications further complicate the
problem.
Any medication is capable of altering nutritional status, which, in the
elderly, may already be compromised by a marginal diet or by chronic disease
and its treatment. Medications can depress the appetite, cause nausea and vomiting,
irritate the stomach, cause constipation or diarrhea, and decrease absorption
of nutrients. In addition, they can alter electrolyte balance and carbohydrate
and fat metabolism. A few examples of medications capable of alter-ing the
nutritional status are antacids, which produce thiamine deficiency; cathartics,
which diminish absorption; antibiotics and phenytoin, which reduce utilization
of folic acid; and phenothi-azines, estrogens, and corticosteroids, which
increase food intake and cause weight gain.
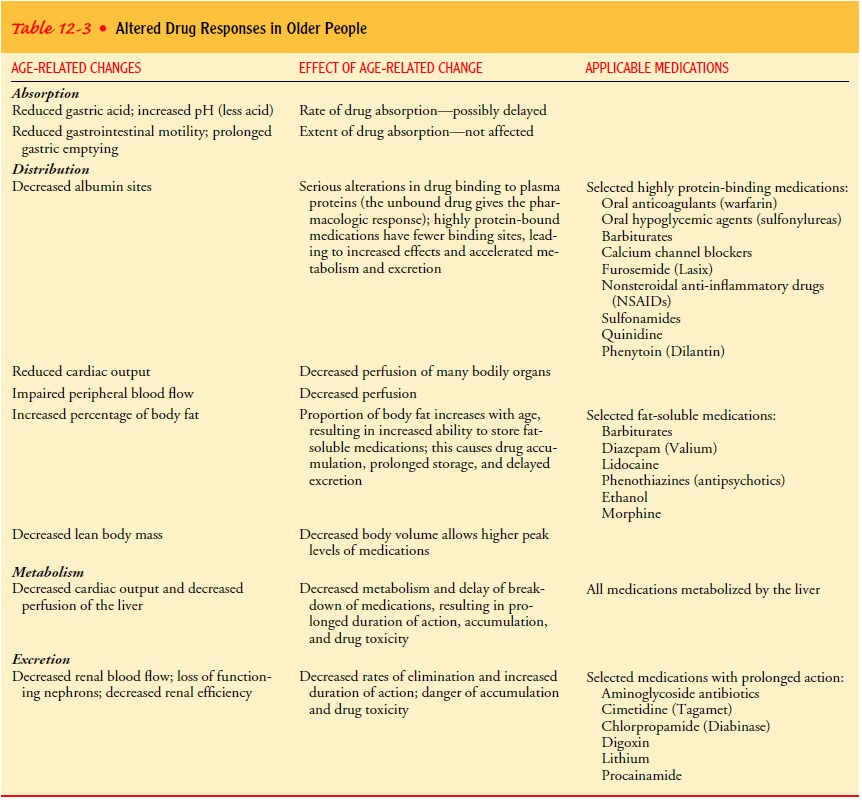
Altered Pharmacokinetics
Pharmacokinetics is the study of the actions of medications in the body,
including the processes of absorption, distribution, metab-olism, and
excretion. Variability in these processes in older peo-ple (Table 12-3) is
caused, in part, by a reduced capacity of the liver and kidneys to metabolize
and excrete the medications and by lowered efficiency of the circulatory and
nervous systems in coping with the effect of certain medications. Many
medications and their metabolites are excreted by the kidney. With advanced
age, body weight, total body water, lean body mass, and plasma albumin
(protein) all decrease, while body fat increases. Conse-quently, agents that
are highly protein-bound have fewer binding sites and higher pharmacologic
activity, whereas fat-soluble agents have more binding sites, and therefore
enhanced storage and de-layed elimination.
Nursing Implications
The nurse administering medications to older people must be aware of the
following:
•
Medications removed from the body primarily by
renal ex-cretion remain in the body for a longer time in people withdecreased
renal function. Often dosages must be reduced, because overdosage and
medication toxicity at usual thera-peutic dosages are common.
•
Medications with a narrow safety margin (eg,
digitalis gly-cosides) must be administered cautiously.
•
A decline in cardiac output may decrease the
delivery rate to the target organ or storage tissue.
•
The circulatory and central nervous systems of
older people are less able to cope with the effects of certain medications,
even when blood levels are normal.
•
Idiosyncratic or unusual responses to medications
may manifest as toxic reactions and complications.
•
As a result of a slowing metabolism, medication
levels may increase in the tissues and plasma, leading to prolonged medication
action.
•
Many elderly people have multiple medical problems
that require treatment with one or more medications. The pos-sibility of
interactions between medications is further magnified if the older person is
also taking one or more over-the-counter medications.
•
A high-fiber diet and the use of psyllium
(Metamucil) or other laxatives may accelerate gastrointestinal transport and
reduce absorption of medications taken concurrently.
•
If, for any reason, a patient is not dependable
about taking medication, the nurse must be sure that the pill or capsule is
actually swallowed and not retained between the cheeks and the gums or teeth.
Teaching
self-administration of medication requires asking the patient questions and
requesting return demonstrations to en-sure that learning has occurred. Sensory
and memory losses, as well as decreased manual dexterity, can affect the
patient’s ability to carry out instructions properly, and the teaching plan
will need to be adjusted to meet each patient’s needs. The following steps
taken by the nurse can help the patient to manage his or her med-ications and
improve compliance:
· Explain the action, side
effects, and dosage of each medication.
· Write out the medication
schedule.
· Encourage the use of
standard containers without safety lids (if there are no children in the
household).
· Suggest the use of a
multiple-day, multiple-dose medication dispenser to help patients adhere to the
medication sched-ule (Fig. 12-5).
· Destroy old, unused
medications.
· Review the medication
schedule periodically.
· Discourage the use of
over-the-counter medications and herbal agents without consulting a health
professional.
· Encourage the patient to
take all medications, including over-the-counter medications, with him or her
regularly when visiting the primary health care provider.
Related Topics