Chapter: Paediatrics: Nephrology
Paediatrics: Urinary tract infection
Urinary tract infection
Up to 3% of girls and 1% of boys
suffer from UTI during childhood. A UTI may be defined in terms of the presence
of symptoms (dysuria, fre-quency, loin pain) plus the detection of a
significant culture of organisms in the urine:
ŌĆó
Any
growth on culture of suprapubic aspirate.
ŌĆó
>105
Organisms/mL in pure growth from a carefully collected urine sample (midstream
urine, clean catch urine, or bag urine). Ideally 2 consecutive growths of the
same organism with identical sensitivities, but this is not always practical.
Note:
Bacteriuria in the absence of
symptoms does not necessarily need treatment,
but needs to be considered in the clinical context (e.g. previous UTI,
predisposing urinary tract abnormalities).
Guidance on the investigation,
treatment and management of UTIs have been published.1
Clinical features
Presentation varies; symptoms in
infants may be non-specific:
ŌĆó
vomiting/diarrhoea;
ŌĆó
poor
feeding/failure to thrive;
ŌĆó
prolonged
neonatal jaundice.
Examination
ŌĆó
Height
and weight: plot on growth chart.
┬Ę BP.
ŌĆó
Examination
for abdominal masses.
ŌĆó
Examine
genitalia and spine for congenital abnormalities.
ŌĆó
Examine
lower limbs for evidence of neuropathic bladder.
Diagnosis
Try to distinguish between upper
(fever, vomiting, loin pain) vs. lower uri-nary tract symptoms (dysuria,
frequency, mild abdominal pain, enuresis). Differentiation is often not
possible in the younger child.
ŌĆó
UTI is
a major cause of sepsis in a young infant.
ŌĆó
Ask
about urinary stream in boys and family history of vesicoureteric reflux (VUR)
or other urinary tract abnormality.
ŌĆó
Dipstick
test in the urine. ŌĆśLeucocytesŌĆÖ and ŌĆśnitritesŌĆÖ strongly suggests UTI. Urine
should be sent for microscopy, culture, and sensitivity.
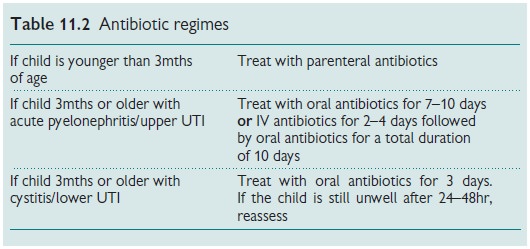
Acute treatment
Antibiotics should be started
after urine collection (see Table 11.2).
Chose antibiotic from:
ŌĆó
Trimethoprim
4mg/kg twice daily.
ŌĆó
Cefradine
25mg/kg twice daily.
ŌĆó
Cefalexin
25mg/kg twice daily.
ŌĆó
Co-amoxiclav
125/31 (1ŌĆō6yrs), 5mL 3 times a day.
ŌĆó
Co-amoxiclav
250/62 (7ŌĆō12yrs) 5mL 3 times a day.
ŌĆó
IV
cefuroxime 25mg/kg 8-hourly; or
ŌĆó
IV
gentamicin 2.5mg/kg/dose 8-hourly.
A repeat urine culture should be
obtained on completion of antibiotics.
Follow-up and investigations
All children presenting with UTI
should be investigated for any renal scar-ring and predisposing urinary tract
abnormalities. Pyelonephritis or recur-rent pyrexial UTIs need more
comprehensive investigation than those at low risk (single, uncomplicated UTI
with lower tract symptoms). Oral an-tibiotic prophylaxis may need to be started and continued until
investigations are complete.
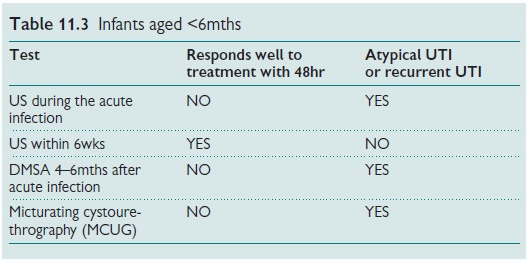
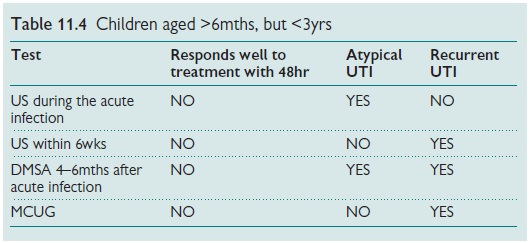
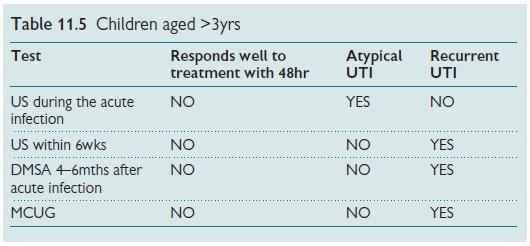
Recommended imaging tests (Tables 11.3ŌĆō11.5)
UTI prevention
Predisposing factors to recurrent
UTIs should be avoided:
ŌĆó
Treat
and prevent constipation.
ŌĆó
Hygiene: clean perineum front to back.
ŌĆó
Avoid
nylon underwear and bubble baths.
┬Ę Encourage fluid intake and regular
toileting with double micturition.
Do not routinely use antibiotic
prophylaxis after first-time UTI, but con-sider it after recurrent UTI.
Oral antibiotic prophylaxis
(trimethoprim 2mg/kg at night or nitrofuran-toin 1mg/kg) is required if:
ŌĆó
VUR.
ŌĆó
Recurrent
UTIs (more than 2ŌĆō3 episodes)
Related Topics