Chapter: Paediatrics: Endocrinology and diabetes
Paediatrics: Type 1 diabetes mellitus: insulin therapy
Type 1 diabetes mellitus: insulin therapy
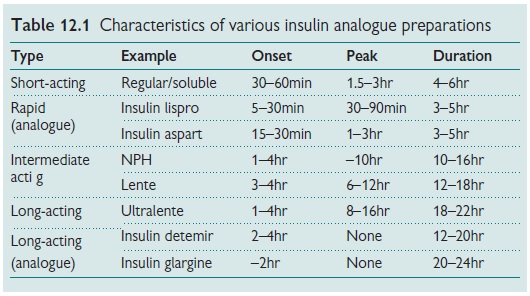
Table 12.1 describes the various
insulin analogue preparations (created by minor amino acid substitutions to the
‘native’ human insulin molecule).
The daily requirement for insulin
varies with age:
· at diagnosis, 0.5U/kg/day;
· childhood/prepubertal,
0.5–1.0U/kg/day;
· puberty, 1.2–2.0U/kg/day;
· post-puberty, 0.7–1.2U/kg/day.
Insulin is administered SC,
usually as a bolus injection. A number of patients receive insulin in the form
of a continuous SC insulin infusion (CSII) deliv-ered by a pump device. Insulin
injection sites include the SC tissues of the upper arm, the anterior and
lateral thigh, the abdomen, and buttocks.
There is a variety of different
daily insulin injection therapy regimens. The choice of regime is a compromise
between achieving optimal therapy and minimizing psychosocial development. The
patient and family must have input into the choice.
Insulin regimens
Two dose regimen
The simplest regimen. Two
injections per day. Each injection is a mix of short/rapid-acting insulin plus an intermediate-acting insulin.
Traditionally 2/3 of the total daily dose is given at breakfast and 1/3 given
before/at the evening meal.
Disadvantages
· Need to mix insulins.
· Peak action of insulin does not
correspond with timing of main meals.
· Increased frequency of between
meal and nocturnal hypoglycaemia.
· Between meal snacks required to
minimize hypoglycaemia.
Note:
Less hypoglycaemia with rapid
analogue insulin use.
Three-dose regimen
Improvement and
intensification of the two-dose regimen:
·At
breakfast: mix of
short or rapid acting insulin plus an
intermediate-acting insulin.
·Before/at
evening meal: short-
or rapid-acting insulin only.
·At
bedtime: intermediate-acting
insulin only.
Advantages
Delayed evening
intermediate-acting insulin results in reduced frequency of nocturnal hypoglycaemia.
Basal bolus regimen
This
regimen attempts to mimic physiological secre-tion. Low level, background,
basal insulin provides for fasting and between meal insulin requirements and
larger acute doses of fast-acting insulin are given to provide for prandial
requirements.
·Basal
insulin: once a day
intermediate- or long-acting insulin (traditionally
at bedtime).
·Fast-acting
insulin: At meal times
(i.e. 3 per day) and with between meal
snacks.
Advantages
·Increased flexibility with meal
times/exercise planning.
·Insulin dose adjustment—
carbohydrate (CHO) counting.
Disadvantages
·Need for more injections.
·Need more frequent blood glucose
monitoring.
CSII
Current insulin infusion pumps are
reliable and portable. CSII therapy can
be used in children of all ages. Short/rapid-acting insulin is adminis-tered as
a continuous insulin infusion. Meal time boluses and ‘blood glu-cose
correction’ boluses are administered when required.
Advantages
·No bolus injections/reduced
injection frequency.
·Increased flexibility meal
times/exercise planning.
·Insulin dose adjustment—CHO
counting.
·Reduced frequency hypoglycaemia.
Disadvantages
·No long-acting insulin. Infusion
interruption: risk of rapid DKA.
·Need more frequent blood glucose
monitoring.
·Greater management expertise
required.
Insulin requirements and dose adjustment
Insulin doses are adjusted based on home blood glucose monitoring. Generally it is best not to
alter the basic insulin regimen every time the blood glucose levels are outside
the target range (4–10mmol/L). Rather, recorded blood glucose levels should be
reviewed and insulin adjustments should be made to correct recurrent profiles
that are either too low or high. Insulin doses are adjusted by 5–10% at a time.
CHO counting: insulin dose adjustment system
Applies the principle that the amounts of fasting/rapid acting insulin given at mealtimes are
adjusted and matched according to the amount of CHO consumed.
Related Topics