Chapter: Modern Medical Toxicology: Hydrocarbons and Pesticides: Pesticides
Organochlorines - Insecticide
Organochlorines
Organochlorine pesticides are one
variety of chlorinated hydro-carbons. There are 4 distinct categories of these
pesticides:
·
DDT and analogues—for example, DDT
(dichlorodiphe-nyltrichloroethane), and methoxychlor.
·
Benzene hexachloride group—for example, benzene hexachlo-ride
(BHC), and gamma-hexachlorocyclohexane (lindane).
·
Cyclodienes and related compounds—for example, aldrin,dieldrin,
endosulfan (thiodan), endrin, isobenzan, chlordane, chlordecone (kepone),
heptachlor, mirex (dechlorane).
·
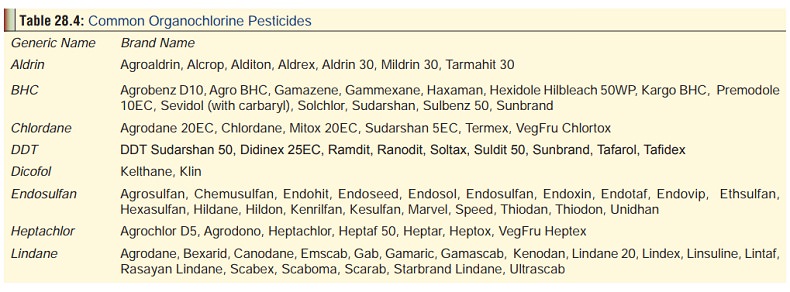
Toxaphene and related compounds—for example, toxaphene.Table 28.4 lists Indian brand names of
organochlorinepesticides.
Physical Appearance
These
compounds are available as dusting powders, wettable powders, emulsions,
granules and solutions.
Uses
·
Insecticide.
·
Gamma benzene hexachloride is used
as a scabicide (treat- ment of scabies), and a pediculocide (eradication of
head lice). It is available as topical ointment, cream, or lotion. Some Indian
brand names include Bexarid
(Shalaks), Gab (Gufic), Gamaric (Euphonic), Scaboma (Glenmark), and Ultrascab
(Perch).
Usual Fatal Dose
·
DDT, lindane: 15 to 30 grams.
·
Aldrin, dieldrin, endrin : 2 to 6 grams.
Toxicity Rating: Dieldrin is placed
in the “extremely toxic” category (LD50:
1 to 50 mg/kg), while DDT, endosulfan, andlindane are considered “highly
toxic”(LD50: 51 to 500 mg/kg), as per
the Insecticide
Rules, 1971.
In addition, the following are extremely toxic: endrin, aldrin, chlordane, and toxaphene, while these are highly toxic: kepone, heptachlor, mirex. The following are least toxic:
![]() methoxychlor, perthane, kelthane,
chlorobenzilate, and hexa-chlorobenzene.
methoxychlor, perthane, kelthane,
chlorobenzilate, and hexa-chlorobenzene.
Acute hazard potential may be ranked
(highest to lowest) approximately as: endrin, aldrin, dieldrin, chlordane,
toxa-phene, kepone, heptachlor, DDT and methoxychlor.
Toxicokinetics
Commercial preparations of
organochlorines are commonly dissolved in petroleum distillates which form
emulsions when added to water. All the organochlorines can be absorbed
trans-dermally, orally, and by inhalation. Gastrointestinal absorption of these
agents is generally efficient, particularly in the pres-ence of absorbable
lipid (animal or vegetable) fat. DDT is the least well absorbed transdermally,
while dieldrin is very well absorbed. Many of these compounds are metabolised
slowly and persist in tissues (especially fat) for prolonged periods. High
residue levels from organochlorine insecticide poisonings are found in adipose
tissue. However, unlike other organochlo-rine pesticides, methoxychlor does not
substantially accumulate in fatty tissues of humans.
Excretion of organochlorine
compounds does not follow first order kinetics. As body stores get lower, the
half-life for the remaining store increases dramatically. This is probably due
to complex lipoprotein binding, wherein different bound forms exhibit different
dissociation characteristics. It is still possible to classify the
organochlorines roughly in terms of the rapidity of excretion from storage
levels that represent an acute toxic threat:
·
Excreted or metabolised within hours to a few days:
o chlordane (except the heptachlor
component)
o chlorobenzilate
o endosulfan
o endrin
o kelthane
o methoxychlor
o perthane
o toxaphene.
·
Excreted within several weeks to a few months:
o Aldrin
o Dieldrin
o Heptachlor
o hexachlorobenzene.
·
Excreted only over several months or years:
o beta isomer of benzene hexachloride
o DDT
o Kepone
o mirex.
Mode of Action
Organochlorines do not depress
cholinesterase enzymes.
These compounds act by various other
mechanisms.
·
DDT and analogues affect the sodium channel and sodium
conductance across the neuronal membrane especially of the axon. They also
alter the metabolism of serotonin, noradrenaline and acetylcholine.
·
The cyclodienes and lindane appear to inhibit the GABA-
mediated chloride channels in the CNS.
·
The neurotoxic mechanism of endosulfan involves inhibi-tion
of the calmodulin-dependant Ca2+ -ATPase activity,alterations in the
serotoninergic system, and inhibition ofGABA receptors.
·
An important property of the chlorinated
hydrocarbons,particularly toxaphene, chlordane, DDT, and lindane is
theircapacity to induce the drug-metabolising enzymes of theliver. Most of these
agents cause liver necrosis and they arepotent enzyme inducers. Evidence
suggests an importantrole of benzoquinones in the hepatotoxicity of
chlorin-ated hydrocarbons as opposed to traditional epoxides. Cytochrome P450
appears to be associated with covalent protein binding of reactive metabolites.
Clinical Features
Acute Poisoning:
·
GIT:
nausea, vomiting, abdominal pain, hyperaesthesiaor paraesthesia of the mouth
and face.
·
CNS:
headache, vertigo, myoclonus, tremor, ataxia,nervousness, amnesia, rapid and dysrhythmic
eye movements, mydriasis, weakness, agitation, confusion, and convulsions.
Occasional reports have associated peripheral neuropathy with exposure to
organochlo-rines.
·
Other
systems: fever, aspiration pneumonitis, renalfailure. Coronary
spasm, hypotension, and sinus tachycardia may occur following exposure.
Dieldrin, endrin, chlordane, toxaphene, and DDT are direct respiratory
depressants. Severe metabolic acidosis has been reported.
·
Organochlorine pesticides such as
DDT pass through the placenta, with an average level in the newborn blood
reaching around a third of that in maternal blood. They can also be found in
breast milk.
Chronic Poisoning:
Long-term exposure to some of these
compounds (chlordecone, chlordane, heptachlor) results in cumulative toxicity
with manifestations such as weight loss, tremor, weak-ness, opsoclonus, ataxia,
pseudotumour cerebri, abnormal mental changes, oligospermia, and increased
tendency to leukaemias, thrombocytopenic purpura, aplastic anaemia,
hepatomegaly, centrilobular hepatic necrosis and liver cancer.
The International Agency for
Research on Cancer (IARC) has listed some of these agents (e.g. DDT) as
“possibly carci-nogenic to humans”, although it also categorises them as being
inadequately assessed for human carcinogenic potential. For other agents (e.g.
aldrin), carcinogenicity has been demon-strated in animal studies, but
insufficient data has accrued from human studies.
Diagnosis
·
Abdominal radiograph may reveal the
presence of certain organochlorines which are radiopaque.
·
Organochlorines can be detected in
serum, adipose tissue, and urine by gas chromatography.
· Blood chlorinated hydrocarbon levels
are not clinically useful following acute exposure. For most compounds they
reflect cumulative exposure over a period of months or years rather than recent
exposure.
·
Measurement of organic halogen
compounds in urine is suggested as an indicator of exposure. Sensitivity is as
low as 1 mcg of organic halogen per 100 ml of urine.
Treatment
·
Decontamination—the same measures as detailed under
organophosphate poisoning must be undertaken.
o Move patient from the toxic
environment to fresh air.
o Monitor for respiratory distress. If
cough or difficulty in breathing develops, evaluate for hypoxia, respiratory
tract irritation, bronchitis, or pneumonitis. Administer 100% humidified
supplemental oxygen, perform endotracheal intubation and provide assisted
ventilation as required. Administer inhaled beta adrenergic agonists if
bronchospasm develops.
o Exposed skin and eyes should be flushed
with copious amounts of water. Remove contaminated clothing and jewelry; wash
skin, hair and nails vigorously with repeated soap washings. Leather absorbs
pesticides; all contaminated leather should be discarded. Rescue personnel and
bystanders should avoid direct contact with contaminated skin, clothing, or
other objects.
·
Do NOT give oils by mouth. They tend to increase intestinal
absorption of these lipophilic toxicants.
·
Seizures should be controlled with benzodiazepines,
phenytoin, or phenobarbitone in the usual way. If they are not effective
enough, sodium thiopentone can be adminis-tered IV, or neuromuscular blockade
is done.
·
Monitor for respiratory depression, hypotension,
arrhyth-mias, and the need for endotracheal intubation. Evaluate for hypoxia,
electrolyte disturbances, and hypoglycaemia (if present, treat with intravenous
dextrose: 50 ml IV (adult), or 2 ml/kg (child) of 25% dextrose).
·
Cholestyramine, a non-absorbable bile acid binding anion
exchange resin is effective in enhancing the faecal excretion of organochlorine
compounds, particularly chlordecone. It is administered at a dose of 16 gm/day
for several days. It can be mixed with fruit juice and given orally (4 gm, 6th
hourly). It can interfere with absorption of other therapeutic drugs which must
therefore be administered either 1 hour before, or 4 hours after each dose of
cholestyramine.
·
Hyperthermia should be managed aggressively with cooling.
·
Supportive measures—special attention must be paid to the
airway and breathing, and adequate circulation should be maintained.
·
The following are contraindicated—oil-based cathartics,
adrenaline, and atropine. Do NOT administer adrenergic amines, which further
increase myocardial irritability and produce refractory ventricular
arrhythmias.
·
Haemodialysis and haemoperfusion have not been proven
effective.
Related Topics