Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Allergic Disorders
Nursing Process: The Patient With Allergic Rhinitis
NURSING
PROCESS: THE PATIENT WITH ALLERGIC RHINITIS
Assessment
The examination and history of the patient
reveal sneezing, often in paroxysms, thin and watery nasal discharge, itching
eyes and nose, lacrimation, and occasionally headache. The health history
includes a personal or family history of allergy. The allergy as-sessment
identifies the nature of antigens, seasonal changes in symptoms, and medication
history. The nurse also obtains sub-jective data about how the patient feels
just before symptoms be-come obvious, such as the occurrence of pruritus,
breathing problems, and tingling sensations. In addition to these symp-toms,
hoarseness, wheezing, hives, rash, erythema, and edema are noted. Any
relationship between emotional problems or stress and the triggering of allergy
symptoms is assessed.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
· Ineffective breathing
pattern related to allergic reaction
· Deficient knowledge
about allergy and the recommended modifications in lifestyle and self-care
practices
· Ineffective individual
coping with chronicity of condition and need for environmental modifications
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on assessment data, potential complications may include the following:
· Anaphylaxis
· Impaired breathing
· Nonadherence to the
therapeutic regimen
Planning and Goals
The
goals for the patient may include restoration of normal breathing pattern,
increased knowledge about the causes and con-trol of allergic symptoms,
improved coping with alterations and modifications, and absence of
complications.
Nursing Interventions
IMPROVING BREATHING PATTERN
The
patient is instructed and assisted to modify the environment to reduce the
severity of allergic symptoms or to prevent their oc-currence. The patient is
instructed to reduce exposure to people with upper respiratory infections
(URIs). If a URI occurs, the pa-tient is encouraged to take deep breaths and
cough frequently to ensure adequate gas exchange and prevent atelectasis. The
patient is instructed to seek medical attention because allergy symptoms along
with a URI may compromise adequate lung function. Compliance with medications
and other treatment regimens is encouraged and reinforced.
PROMOTING UNDERSTANDING OF ALLERGY AND ALLERGY CONTROL
Instruction includes strategies to minimize
exposure to allergens, desensitization procedures, and correct use of
medications. The nurse informs and reminds the patient of the importance of
keep-ing appointments for desensitization procedures because usually dosages
are adjusted on a weekly basis, and missed appointments may interfere with the
dosage adjustment.
Patients
also need to understand that medications for allergy control should be used
only when the allergy is apparent. This is usually on a seasonal basis.
Continued use of medications when not required may cause an increased tolerance
to the med-ication, with the result that the medication is not effective when
needed.
COPING WITH A CHRONIC DISORDER
Although allergic reactions are infrequently
life-threatening, they require constant vigilance to avoid allergens and
modification of the lifestyle or environment to prevent recurrence of symptoms.
Allergic symptoms are often present year-round and create dis-comfort and
inconvenience for the patient. Although patients may not feel ill during
allergy seasons, they often do not feel well either. The need to be alert for
possible allergens in the environ-ment may be tiresome, placing a burden on the
patient’s ability to lead a normal life. Stress related to these difficulties
may in turn increase the frequency or severity of symptoms.
To
assist the patient in adjusting to these modifications, the nurse must have an
appreciation of the difficulties encounteredby the patient. The patient is
encouraged to verbalize feelings and concerns in a supportive environment and
to identify strategies to deal with them effectively.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Anaphylaxis and Impaired Breathing
Respiratory and cardiovascular functioning
can be significantly altered during allergic reactions by the reaction itself
or by the medications used to treat reactions. The respiratory status is
eval-uated by monitoring the respiratory rate and pattern and by as-sessing for
breathing difficulties or abnormal lung sounds. The pulse rate and rhythm and
blood pressure are monitored to assess cardiovascular status regularly or any
time the patient reports symptoms such as itching or difficulty breathing. In
the event of signs and symptoms suggestive of anaphylaxis, emergency
med-ications and equipment must be available for immediate use.
Nonadherence to Therapeutic Regimen
Knowing
about the treatment regimen does not ensure adher-ence. Having the patient
identify potential barriers and explore acceptable solutions for effective
management of the condition (eg, installing tile floors rather than carpet, not
gardening in the spring) can increase adherence to the treatment regimen.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
patient is instructed about strategies to minimize exposure to allergens, the
actions and adverse effects of medications, and the correct use of medications.
The patient should know the names, dose, frequency, actions, and side effects
of all medications taken.
Instruction
about strategies to control allergic symptoms is based on the needs of the
patient as determined by the results of tests, the severity of symptoms, and
the motivation of the patient and family to deal with the condition.
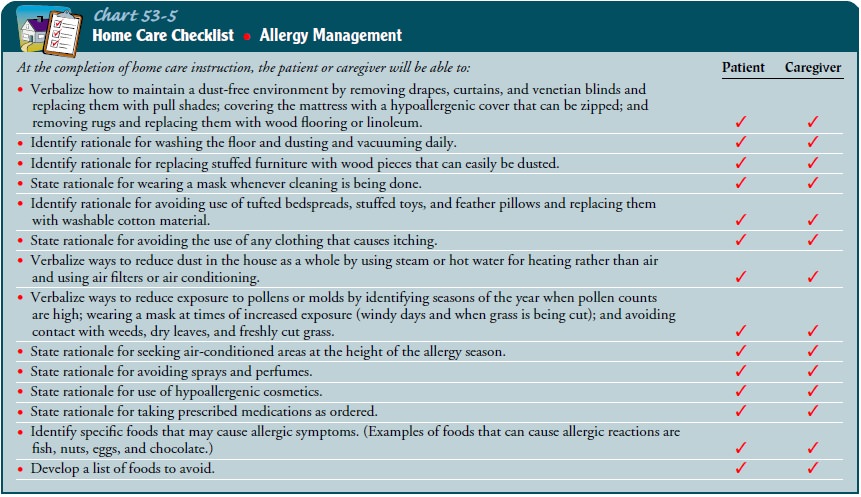
Suggestions for patients sensitive to dust and mold in the home are given in
Chart 53-5.
If the
patient is to undergo immunotherapy, the nurse re-inforces the physician’s
explanation regarding the purpose and procedure. Instructions are given
regarding the series of injec-tions, usually given initially every week and
then at 2- to 4-week intervals. These instructions include remaining in the
physician’s office or the clinic at least 30 minutes after the injection so
that emergency treatment may be given if the patient has a reaction; avoiding
rubbing or scratching the injection site; and continuing with the series for
the period of time required. In addition, the patient and family are instructed
about emergency treatment of severe allergic symptoms.
Because
antihistamines often produce drowsiness, the patient is cautioned about this
and other side effects of the particular medication. Operating machinery,
driving a car, and performing activities requiring intense concentration should
be postponed. The patient is also informed about the dangers of drinking
alco-hol when taking these medications because they tend to exagger-ate the
effects of alcohol.
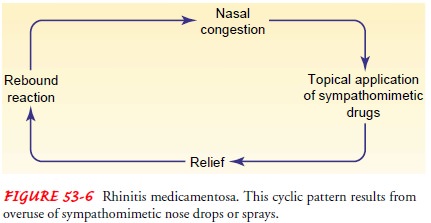
The patient must be aware of the effects
caused by overuse of the sympathomimetic agents in nose drops or sprays. A
condition referred to as rhinitis medicamentosa may result (Fig. 53-6). After topical
application of the medication, a rebound period may occur in which the nasal
mucous membranes become more ede-matous and congested than they were before the
medication was used. Such a reaction encourages the use of more medication, and
a cyclical pattern results. The topical agent must be discontinued immediately
and completely to correct this problem.
Continuing Care
Follow-up
telephone calls to the patient are often reassuring to the patient and family
and provide an opportunity for the nurse to answer any questions. The patient
is reminded to keep follow-up appointments and is informed about the importance
of con-tinuing with treatment. The importance of participating in health
promotion activities and health screening is emphasized to the patient.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Exhibits
normal breathing patterns
a) Demonstrates
lungs clear on auscultation
b) Exhibits
absence of adventitious breath sounds (crack-les, rhonchi, wheezing)
c) Has
a normal respiratory rate and pattern
d) Reports
no complaints of respiratory distress (shortness of breath, difficulty on inspiration
or expiration)
2) Demonstrates
knowledge about allergy and strategies to control symptoms
a) Identifies
causative allergens, if known
b) States
methods of avoiding allergens and controlling in-door and outdoor precipitating
factors
c) Removes
from the environment items that retain dust
d) Wears
a dampened mask if dust or mold may be a problem
e) Avoids
smoke-filled rooms and dust-filled or freshly sprayed areas
f) Uses
air conditioning for a major part of the day
g) Takes
antihistamines as prescribed; participates in hypo-sensitization program, if
applicable
h) Describes
name, purpose, side effects, and method of administration of prescribed
medications
i) Identifies
when to seek immediate medical attention for severe allergic responses
j) Describes
activities that are possible, including ways to participate in activities
without activating the allergies
3) Experiences
relief of discomfort while adapting to the in-conveniences of an allergy
a) Relates
the emotional aspects of the allergic response
b) Demonstrates
use of measures to cope positively with allergy
4) Absence
of complications
a) Exhibits
vital signs within normal limits
b) Reports
no symptoms or episodes of anaphylaxis (ur-ticaria, itching, peripheral
tingling, fullness in the mouth and throat, flushing, or difficulty swallowing)
or cough-ing, wheezing, or difficulty breathing
c) Demonstrates
correct procedure to self-administer emer-gency medications to treat severe
allergic reaction
d) Correctly
states medication names, dose and frequency of administration, and medication
actions
e) Correctly
identifies side effects and untoward signs and symptoms to report to physician
f) Discusses
acceptable lifestyle changes and solutions for identified potential barriers
for compliance with treat-ment and medication regimen
Related Topics