Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Allergic Disorders
Allergic Reaction: Physiologic Overview
Allergic Reaction: Physiologic
Overview
An allergic reaction is a manifestation of
tissue injury resulting from interaction between an antigen and an antibody.
Allergy is an inappropriate and often harmful response of the immune system to
normally harmless substances. In this case, the substance is termed an
allergen. Atopy refers to allergic reactions characterized by the action of IgE
antibodies and a genetic predisposition to allergic reactions.When the body is
invaded by an antigen, usually a protein that the body’s defenses recognize as
foreign, a series of events occurs in an attempt to render the invader
harmless, destroy it, and remove it from the body. When lymphocytes respond to
the antigen, antibodies (protein substances that protect against antigens) are
produced. Common allergic reactions occur when the immune system of a
susceptible person responds aggressively to asubstance that is normally
harmless (eg, dust, weeds, pollen, dander). Chemical mediators released in
allergic reactions may produce symptoms ranging from mild to
life-threatening.The many cells and organs of the immune system secrete various
substances important in the immune response. These parts of the immune system
must work together to ensure adequate defense
against invaders (ie,
virus, bacteria, other
foreign substances) without
destroying the body’s own tissues by an overly aggressive reaction.
FUNCTION AND PRODUCTION OF IMMUNOGLOBULINS
Antibodies formed by lymphocytes and plasma
cells in response to an immunogenic stimulus constitute a group of serum
proteins called immunoglobulins. Grouped into five classes (IgE, IgD, IgG, IgM,
and IgA), antibodies can be found in the lymph nodes, tonsils, appendix, and
Peyer’s patches of the intestinal tract or circulating in the blood and lymph.
Each antibody molecule is composed of two identical heavy (H) chains and two
identical light (L) chains. Each chain contains one variable region and one or
more constant regions. The constant regions determine the class (IgE, IgD,
etc.) of each antibody and allow each class of antibody to interact with
specific effector cells and molecules. The variable regions contain
antigen-binding sites (Porth, 2002). Antibodies are capable of binding with a
wide variety of antigens, which include macromolecules and small chemicals
(Abbas & Lichtman,2001). Antibodies of the IgM, IgG, and IgA classes have
definite and well-established protective functions. These include
neutralization of toxins and viruses and precipitation, agglutination, and
lysis of bacteria and other foreign cellular material. Immunoglobulins of the IgE class are involved in allergic
disorders and some parasitic infections, evidenced by elevation of IgE levels.
IgE-producing cells are located in the respiratory an intestinal mucosa. Two or
more IgE molecules bind together to an allergen and trigger mast cells or
basophils to release chemical mediators, such as histamine, serotonin, kinins,
slow-reacting substance of anaphylaxis (SRS-A), and the neutrophil factor,which
produces allergic skin reactions, asthma, and hay fever.
Antibodies combine with antigens in a special
way, likened to keys fitting into a lock. Antigens (the keys) only fit certain
anti-bodies (the locks). Hence, the term “specificity” refers to the spe-cific
reaction of an antibody to an antigen. There are many variations and
complexities in these patterns. The strength with which one antigen-binding
surface of an antibody binds to one epitope,
an immunologically active site on an antigen, is knownas the affinity of the
interaction (Abbas & Lichtman, 2001).
Antibody molecules are bivalent; that is,
they have two com-bining sites. Therefore, the antibody easily becomes a
cross-link between two antigen groups, causing them to clump together
(ag-glutination). By this action, foreign invaders are cleared from the
bloodstream. Agglutination is the means for determining blood group in
laboratory tests.
Role of B Cells
The B
cell, or B lymphocyte, is programmed
to produce one spe-cific antibody. On encountering a specific antigen, a B cell
stim-ulates production of plasma cells, the site of antibody production. The
result is the outpouring of antibodies for the purpose of de-stroying and
removing the antigen.
Role of T Cells
The T
cell, or T lymphocyte, assists the B
cells in producing an-tibodies. T cells secrete substances known as lymphokines that encourage cell growth,
promote cell activation, direct the flow of cell activity, destroy target
cells, and stimulate the macrophages. Macrophages present the antigen to the T
cells and initiate the immune response. They also digest antigens and assist in
remov-ing cells and other debris. The antigen-binding site of a T cell has a
structure much like that of an immunoglobulin. It recognizes epitopes through
complementary interactions. Unlike a specific antibody, a T cell does not bind
free antigens (Parslow, Stites, Terr & Imboden, 2001).
FUNCTION OF ANTIGENS
Antigens are divided into two groups:
complete protein antigens and low-molecular-weight substances. Complete protein
antigens, such as animal dander, pollen, and horse serum, stimulate a com-plete
humoral response. Low-molecular-weight
substances, such as medica-tions, function as haptens (incomplete antigens), binding to tis-sue or serum proteins
to produce a carrier complex that initiates an antibody response. The term
“hapten” is derived from the Greek word haptien
(to fasten). The proteins or other immuno-gens that haptens are fastened to are
known as carriers (Parslow et al., 2001).
In an allergic reaction, the production of
antigen-specific IgE antibodies requires active communication between
macrophages, T cells, and B cells. When the allergen is absorbed through the
respiratory tract, gastrointestinal tract, or skin, allergen sensitiza-tion
occurs. The macrophage processes the antigen and presents it to the appropriate
T cell. B cells that are influenced by the cell mature into an allergen-specific IgE
immunoglobulin-secreting plasma cell that synthesizes and secretes
antigen-specific IgE antibody.
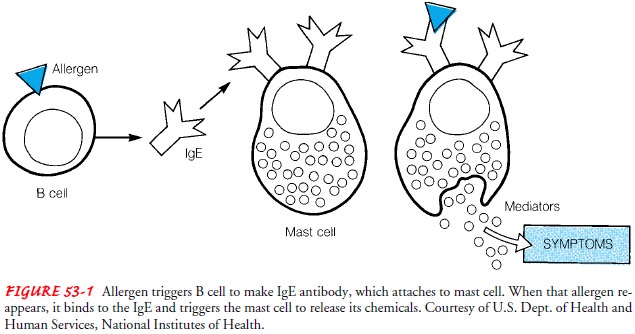
FUNCTION OF CHEMICAL MEDIATORS
Mast
cells, which have a major role in IgE-mediated immediate hypersensitivity, are
located in the skin and mucous mem-branes. When mast cells are stimulated by
antigens, powerful chemical mediators are released that cause a sequence of
physi-ologic events resulting in symptoms of immediate hypersensi-tivity (Fig.
53-1). There are two types of chemical mediators: primary, which are preformed
and found in mast cells or ba-sophils, and secondary, which are inactive
precursors formed or released in response to primary mediators. The most
prevalent known primary and secondary mediators are described next. Table 53-1
summarizes the actions of primary and secondary chemical mediators.
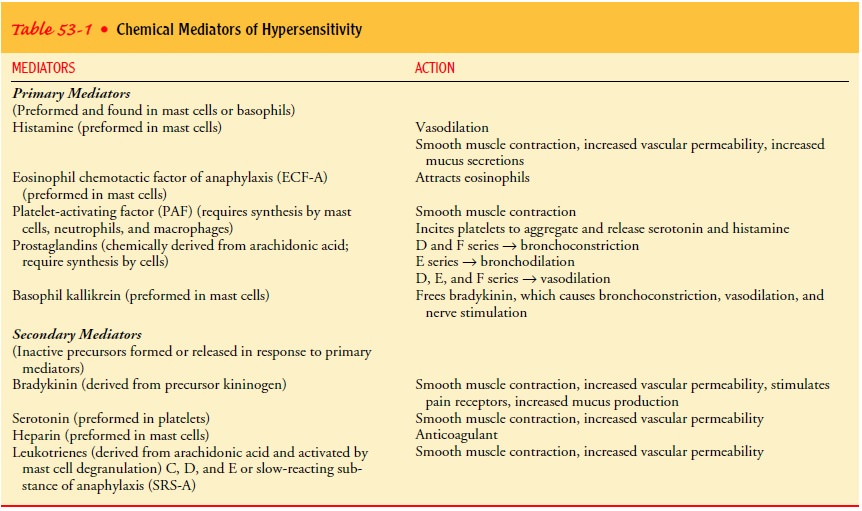
Primary Mediators
IgE-mediated inflammation occurs when an antigen binds to the IgE antibodies that occupy certain receptors on mast cells. Within minutes, this binding causes the mast cell to degranulate, releasing certain preformed mediators. A two-phase response results. There is an initial immediate effect on blood vessels, smooth muscle, and glandular secretion. This is followed a few hours later by cellular infiltration of the involved site. This type of inflammatory response is commonly known as an immediate hypersensitivity response (Parslow et al., 2001).
HISTAMINE
Histamine plays an important role in the immune response. His-tamine is released
from mast cell granules where it is stored. Max-imal intensity is reached
within about 15 minutes after antigen contact (Parslow et al., 2001). The
effects of histamine release in-clude erythema; localized edema in the form of
wheals; pruritus; contraction of bronchial smooth muscle, resulting in wheezing
and bronchospasm; dilation of small venules and constriction of larger vessels;
and increased secretion of gastric and mucosal cells, resulting in diarrhea.
Histamine action results from stimulation of histamine-1 (H1) and histamine-2 (H2) receptors found on dif-ferent types of
lymphocytes, particularly T-lymphocyte suppres-sor cells and basophils. H1 receptors are found predominantly on
bronchiolar and vascular smooth muscle cells. H2 receptors are found on gastric parietal cells.
Certain medications are categorized by their
action at these re-ceptors. Diphenhydramine (Benadryl) is an example of an anti-histamine, which is a medication
displaying an affinity for H1receptors; cimetidine (Tagamet) and ranitidine (Zantac) are ex-amples of
other pharmacologic agents that target H2 receptors to inhibit gastric secretions in peptic ulcer disease.
EOSINOPHIL CHEMOTACTIC FACTOR OF ANAPHYLAXIS
Preformed in the mast cells, this chemotactic
factor, which affects movement of eosinophils
(granular leukocytes) to the site of al-lergens, is released upon degranulation
to inhibit the action of leukotrienes and histamine.
PLATELET-ACTIVATING FACTOR
Platelet-activating
factor (PAF) is responsible for initiating platelet aggregation at sites of
immediate hypersensitivity reac-tions. It also causes bronchoconstriction and
increased vascular permeability. PAF also activates factor XII, or Hageman
factor, which induces the formation of bradykinin.
PROSTAGLANDINS
Prostaglandins, composed of unsaturated fatty acids,
producesmooth muscle contraction as well as vasodilation and increased
capillary permeability. The fever and pain that occur with in-flammation are
due in part to the prostaglandins.
Secondary Mediators
LEUKOTRIENES
Leukotrienes are chemical mediators that initiate the inflamma-tory response. They
are metabolites released by mucosal mast cells. They collectively make up what
was once termed “slow-reacting substance of anaphylaxis” (SRS-A). Leukotrienes
cause smooth muscle contraction, bronchial constriction, mucus secretion in the
airways, and the typical wheal and flare reaction of the skin (Parslow et al.,
2001). Compared with histamine, leukotrienes are 100 to 1,000 times more potent
in causing bronchospasm. Many manifestations of inflammation can be attributed
in part to leukotrienes. Medications categorized as leukotriene antagonists or
modifiers (zileuton [Zyflo], zafirlukast [Accolate], montelukast [Singulair])
block the synthesis or action of leukotrienes and pre-vent the signs and
symptoms associated with asthma.
BRADYKININ
Bradykinin is a polypeptide with the ability to cause increasedvascular
permeability, vasodilation, hypotension, and contraction of many types of
smooth muscle, such as the bronchi (Parslow et al., 2001). Increased
permeability of the capillaries results in edema. Bradykinin stimulates nerve
cell fibers and produces pain.
SEROTONIN
Serotonin is released during platelet aggregation,
acting as a po-tent vasoconstrictor and causing contraction of bronchial smooth
muscle.
HYPERSENSITIVITY
Although
the immune system defends the host against infections and foreign antigens,
immune responses can themselves cause tis-sue injury and disease. An immune
response to an antigen may result in sensitivity to challenge with that
antigen; hypersensi-tivity is a
reflection of excessive or aberrant immune responses(Abbas & Lichtman,
2001).
A hypersensitivity reaction is an abnormal,
heightened reaction to any type of stimuli. It usually does not occur with the
first ex-posure to an allergen. Rather, the reaction follows a re-exposure
after sensitization in a predisposed individual. Sensitization initi-ates the
humoral response or buildup of antibodies. To promote understanding of the
immunopathogenesis of disease, hypersen-sitivity reactions have been classified
into four specific types of reactions (Fig. 53-2). Most allergies are identified
as either type I or type IV hypersensitivity reactions.
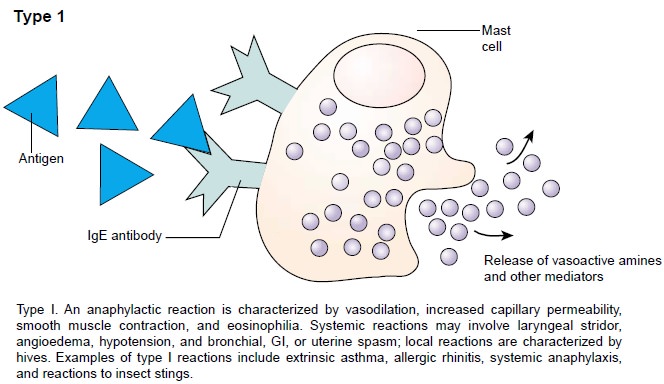
Anaphylactic (Type I) Hypersensitivity
The most severe form of a hypersensitivity reaction is anaphy-laxis. This systemic reaction is characterized by edema in manytissues, including the larynx, and is often accompanied by hy-potension (Abbas & Lichtman, 2001). Type I or anaphylactic hy-persensitivity is an immediate reaction beginning within minutes of exposure to an antigen. This reaction is mediated by IgE anti-bodies rather than IgG or IgM antibodies. Type I hypersensitiv-ity requires previous exposure to the specific antigen. In turn, the plasma cells produce IgE antibodies in the lymph nodes, where helper T cells aid in promoting this reaction. The IgE antibodies bind to membrane receptors on mast cells found in connective tissue and basophils.
During re-exposure, the antigen binds to ad-jacent IgE antibodies, activating a
cellular reaction that triggers degranulation and the release of chemical
mediators (histamine, leukotrienes, and eosinophil chemotactic factor of
anaphylaxis [ECF-A]).
Primary
chemical mediators are responsible for the symptoms of type I hypersensitivity
because of their effects on the skin, lungs, and gastrointestinal tract. When
chemical mediators con-tinue to be released, a delayed reaction may occur
lasting for up to 24 hours. Clinical symptoms are determined by the amount of
the allergen, the amount of mediator released, the sensitivity of the target
organ, and the route of allergen entry. Type I hyper-sensitivity reactions may
include both local and systemic anaphylaxis.
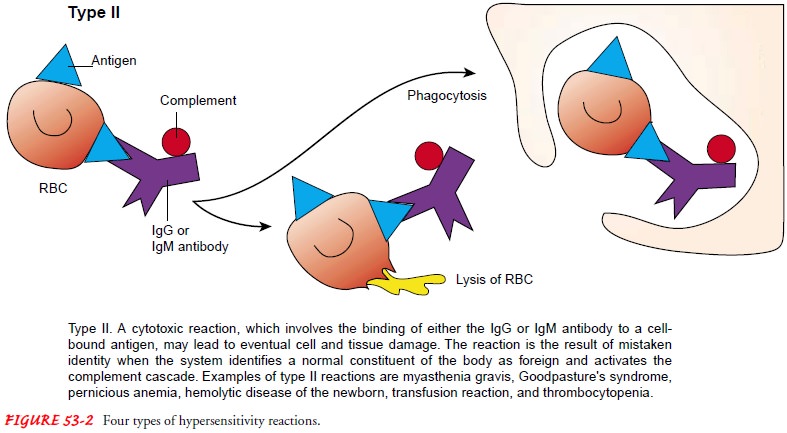
Cytotoxic (Type II) Hypersensitivity
Type II, or cytotoxic, hypersensitivity
occurs when the system mistakenly identifies a normal constituent of the body
as foreign. This reaction may be a result of a cross-reacting antibody,
possi-bly leading to cell and tissue damage. Type II hypersensitivity involves
the binding of either IgG or IgM antibody to the cell-bound antigen. The result
of antigen–antibody binding is activa-tion of the complement cascade and
destruction of the cell to which the antigen is bound.
A type II hypersensitivity reaction is associated with several disorders. For example, in myasthenia gravis, the body mistak-enly generates antibodies against normal nerve ending receptors. In Goodpasture syndrome, antibodies against lung and renal tis-sue are generated, producing lung damage and renal failure.
A type
II hypersensitivity reaction resulting in red blood cell de-struction is
associated with drug-induced immune hemolytic ane-mia, Rh-hemolytic disease of
the newborn, and incompatibility reactions in blood transfusions.
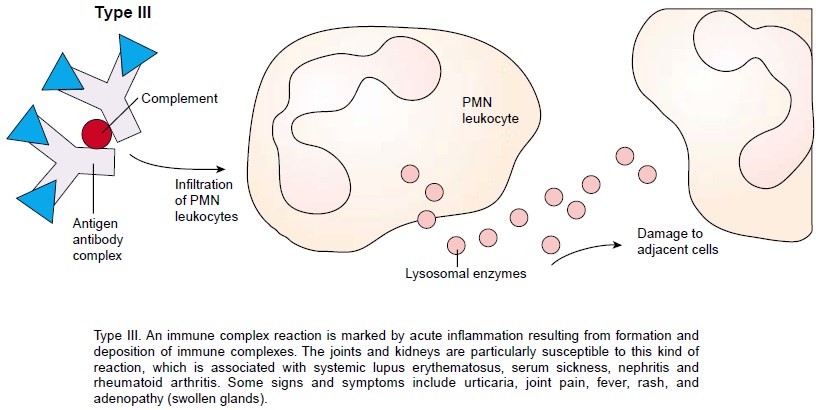
Immune Complex (Type III) Hypersensitivity
Type III, or immune complex, hypersensitivity
involves immune complexes formed when antigens bind to antibodies. These
com-plexes are then cleared from the circulation by phagocytic action. When
these type III complexes are deposited in tissues or vascu-lar endothelium, two
factors contribute to injury: the increased amount of circulating complexes and
the presence of vasoactive amines. As a result, there is an increase in
vascular permeability and tissue injury. The joints and kidneys are
particularly suscep-tible to this type of injury. Type III hypersensitivity is
associated with systemic lupus erythematosus, rheumatoid arthritis, certain
types of nephritis, and some types of bacterial endocarditis. These are
discussed elsewhere in this text.
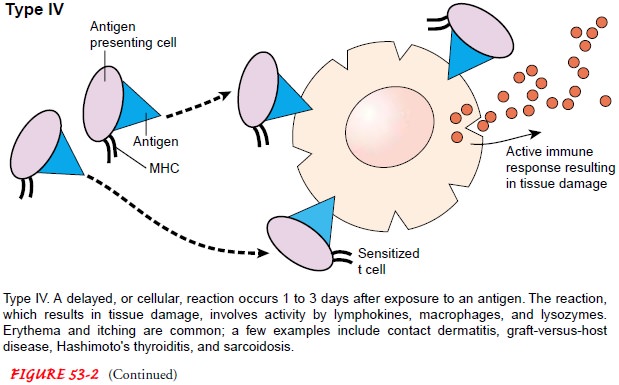
Delayed-Type (Type IV) Hypersensitivity
Type
IV, or delayed-type hypersensitivity, also known as cellular hypersensitivity,
occurs 24 to 72 hours after exposure to an aller-gen. It is mediated by
sensitized T cells and macrophages. An ex-ample of this reaction is the effect
of an intradermal injection of tuberculin antigen or purified protein derivative
(PPD). Sensitized T cells react with the antigen at or near the injection site.
Lym-phokines are released and attract, activate, and retain macrophages at the
site. These macrophages then release lysozymes, causing tis-sue damage. Edema
and fibrin are responsible for the positive tu-berculin reaction.
An
example of a type IV hypersensitivity reaction is contact dermatitis resulting
from exposure to allergens such as cosmetics, adhesive tape, topical
medications, medication additives, and plant toxins. The primary exposure
results in sensitization. Re-exposure causes a hypersensitivity reaction
composed of low-molecular-weight molecules (haptens) that bind with proteins or
carriers and are then processed by Langerhans cells in the skin. The symptoms
that occur include itching, erythema, and raised lesions.
Related Topics