Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Allergic Disorders
Allergic Rhinitis - Allergic Disorders
ALLERGIC
RHINITIS
Allergic
rhinitis (inflammation of nasal
mucosa; hay fever, chronic allergic rhinitis, pollinosis) is the most common
form of respiratory allergy presumed to be mediated by an immediate (type I
hypersensitivity) immunologic reaction. It affects about 8% to 10% of the U.S.
population (20% to 30% of adolescents). The symptoms are similar to viral
rhinitis but are usually more persistent and demonstrate seasonal variation
(Tierney, McPhee Papadakis, 2001). It often occurs with other conditions, such
as allergic conjunctivitis, sinusitis, and asthma. Allergic rhinitis is
associated with impaired work and school performance and de-creased quality of
life (Ratner, Ehrlich, Fineman et al., 2002). When untreated, many
complications may result, such as allergic asthma, chronic nasal obstruction,
chronic otitis media with hear-ing loss, anosmia (absence of the sense of
smell), and, in children, orofacial dental deformities. Early diagnosis and
adequate treat-ment are essential to reduce complications and relieve symptoms.
Because
allergic rhinitis is induced by airborne pollens or molds, it is characterized
by the following seasonal occurrences:
· Early spring—tree pollen
(oak, elm, poplar)
· Early summer—rose pollen
(rose fever), grass pollen (Timothy, red-top)
· Early fall—weed pollen
(ragweed)
Each
year, attacks begin and end at about the same time. Air-borne mold spores
require warm, damp weather. Although there is no rigid seasonal pattern, these
spores appear in early spring, are rampant during the summer, and taper off and
disappear by the first frost.
Pathophysiology
Sensitization begins by ingestion or inhalation of an antigen. On re-exposure, the nasal mucosa reacts by the slowing of ciliary ac-tion, edema formation, and leukocyte (primarily eosinophil) in-filtration. Histamine is the major mediator of allergic reactions in the nasal mucosa. Tissue edema results from vasodilation and increased capillary permeability.
Clinical Manifestations
Typical signs and symptoms of allergic
rhinitis include nasal con-gestion; clear, watery nasal discharge; intermittent
sneezing; and nasal itching. Itching of the throat and soft palate is common.
Drainage of nasal mucus into the pharynx initiates multiple at-tempts to clear
the throat and results in a dry cough or hoarseness. Headache, pain over the
paranasal sinuses, and epistaxis can ac-company allergic rhinitis. The symptoms
of this chronic condition depend on environmental exposure and intrinsic host
responsive-ness. Allergic rhinitis may affect quality of life by also producing
fatigue,
loss of sleep, and poor concentration (Ratner et al., 2002).
Assessment and Diagnostic Findings
Diagnosis of seasonal allergic rhinitis is
based on history, physi-cal examination, and diagnostic test results.
Diagnostic tests in-clude nasal smears, peripheral blood counts, total serum
IgE, epicutaneous and intradermal testing, RAST, food elimination and
challenge, and nasal provocation tests. Results indicative of allergy as the
cause of rhinitis include increased IgE and eosinophil levels and positive
reactions on allergen testing. False-positive and false-negative responses to
these tests, particularly skin testing and provocation tests, may occur.
Medical Management
The goal of therapy is to provide relief from
symptoms. Therapy may include one or all of the following interventions:
avoidance therapy, pharmacotherapy, and immunotherapy (Kay, 2001b). Verbal
instructions must be reinforced by written information. Knowledge of general
concepts regarding assessment and therapy in allergic diseases is important so
that patients can learn to manage certain conditions as well as prevent severe
reactions and illnesses.
AVOIDANCE THERAPY
In avoidance therapy, every attempt is made
to remove the aller-gens that act as precipitating factors. Simple measures and
envi-ronmental controls are often effective in decreasing symptoms. Examples
include use of air conditioners, air cleaners, humidifiers and dehumidifiers,
and smoke-free environments. In many cases, it is impossible to avoid exposure
to all environmental allergens, so pharmacologic therapy or immunotherapy is
needed.
PHARMACOLOGIC THERAPY
Antihistamines.
Antihistamines,
now classified as H1-receptorantagonists (or H1-blockers),
are used in managing mild allergic disorders. (H2-receptor antagonists are used to
treat gastric and duodenal ulcers.) H1-blockers bind selectively to H1 receptors,
preventing the actions of histamines at these sites. They do not prevent the
release of histamine from mast cells or basophils. The H1-antagonists
have no effect on H2-receptors, but they do have the
ability to bind to nonhistaminic receptors. The ability of cer-tain
antihistamines to bind to and block muscarinic receptors un-derlies several of
the prominent anticholinergic side effects of these medications.
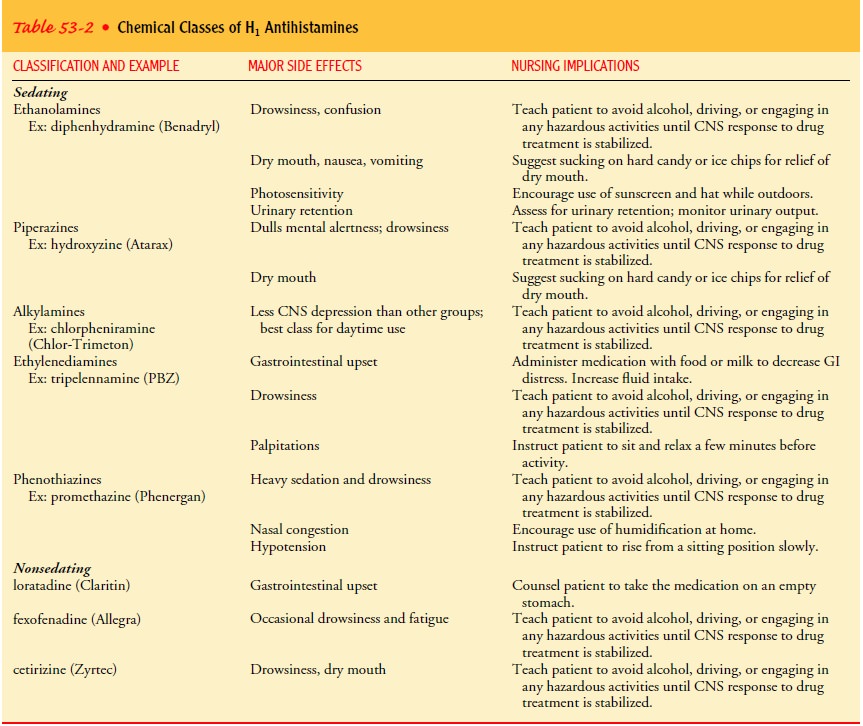
Oral antihistamines, which are readily
absorbed, are most ef-fective when given at the first occurrence of symptoms
because they prevent the development of new symptoms by blocking the actions of
histamine at the H1-receptors. The effectiveness of these medications is limited to certain
patients with hay fever, va-somotor rhinitis, urticaria (hives), and mild asthma. They are rarely effective in
other conditions or in any severe conditions.Antihistamines are the major class of
medications prescribed for the symptomatic relief of allergic rhinitis. The
major side ef-fect is sedation, although histamine H1 antagonists are less
sedat-ing than earlier antihistamines (Kay, 2001b). Additional side effects
include nervousness, tremors, dizziness, dry mouth, palpi-tations, anorexia,
nausea, and vomiting. Antihistamines are con-traindicated during the third
trimester of pregnancy; for nursing mothers and newborns; in children and
elderly people; and in pa-tients whose conditions can be aggravated by
muscarinic blockade (ie, asthma, urinary retention, open-angle glaucoma,
hyperten-sion, and prostatic hyperplasia).
Newer
antihistamines are called second-generation or non-sedating H1-receptor antagonists.
Unlike first-generation H1-receptor antagonists, they do not cross the
blood–brain barrier and do not bind to cholinergic, serotonin, or
alpha-adrenergic re-ceptors. They bind to peripheral rather than central
nervous sys-tem H1-receptors, causing less sedation. Examples of
these medications are loratadine (Claritin), cetirizine (Zyrtec), and
fex-ofenadine (Allegra). These are summarized in Table 53-2.tion to the oral
route. The topical route (drops and sprays) causes fewer side effects than oral
administration; however, the use of drops and sprays should be limited to a few
days to avoid rebound congestion. Adrenergic nasal decongestants are used for
the relief of nasal congestion when applied topically to the nasal mucosa. They
activate the alpha-adrenergic receptor sites on the smooth muscle of the nasal
mucosal blood vessels, reducing local blood flow, fluid exudation, and mucosal
edema. Topical ophthalmic drops are used for symptomatic relief of eye
irritations due to al-lergies. Potential side effects include hypertension,
dysrhythmias, palpitations, central nervous system stimulation, irritability,
tremor, and tachyphylaxis (acceleration of hemodynamic status). Examples of
adrenergic decongestants and their routes of admin-istration are found in Table
53-3.
Mast Cell Stabilizers.
Intranasal cromolyn sodium (Nasalcrom)is a spray that acts by
stabilizing the mast cell membrane, thus re-ducing the release of histamine and
other mediators of the aller-gic response. In addition, it inhibits
macrophages, eosinophils, monocytes, and platelets involved in the immune
response (Ratner et al., 2002). Cromolyn interrupts the physiologic response to
nasal antigens and is used prophylactically before exposure to
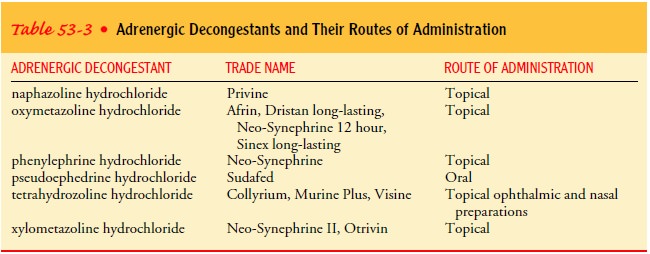
Adrenergic Agents.
Adrenergic agents, vasoconstrictors of mu-cosal vessels, are used
topically (nasal and ophthalmic) in addition to the oral route. The topical route
(drops and sprays) causes fewer side effects than oral administration; however,
the use of drops and sprays should be limited to a few days to avoid rebound
congestion. Adrenergic nasal decongestants are used for the relief of nasal
congestion when applied topically to the nasal mucosa. They activate the
alpha-adrenergic receptor sites on the smooth muscle of the nasal mucosal blood
vessels, reducing local blood flow, fluid exudation, and mucosal edema. Topical
ophthalmic drops are used for symptomatic relief of eye irritations due to
al-lergies. Potential side effects include hypertension, dysrhythmias,
palpitations, central nervous system stimulation, irritability, tremor, and
tachyphylaxis (acceleration of hemodynamic status). Examples of adrenergic
decongestants and their routes of admin-istration are found in Table 53-3.
Mast Cell Stabilizers.
Intranasal cromolyn sodium (Nasalcrom)is a spray that acts by stabilizing the mast cell membrane, thus re-ducing the release of histamine and other mediators of the aller-gic response. In addition, it inhibits macrophages, eosinophils, monocytes, and platelets involved in the immune response (Ratner et al., 2002). Cromolyn interrupts the physiologic response to nasal antigens and is used prophylactically before exposure to allergens to prevent the onset of symptoms and to treat symptoms once they occur.
It is also used therapeutically in
chronic allergic rhinitis. This spray is as effective as antihistamines but
less effec-tive than intranasal corticosteroids in the treatment of seasonal
allergic rhinitis. Patients must be informed that the beneficial ef-fects of
the medication may take a week or so to occur. The med-ication is of no benefit
in the treatment of nonallergic rhinitis. Adverse effects (ie, sneezing, local
stinging, and burning sensa-tions) are usually mild.
Corticosteroids.
Intranasal corticosteroids are indicated in moresevere cases of allergic
and perennial rhinitis that cannot be con-trolled by more conventional
medications such as decongestants, antihistamines, and intranasal cromolyn.
These medications include beclomethasone (Beconase, Vancenase), budesonide
(Rhinocort), dexamethasone (Decadron Phosphate Turbinaire), flunisolide
(Nasalide), fluticasone (Cutivate, Flonase), and tri-amcinolone (Nasacort).
Because of their anti-inflammatory actions,
these medications are equally effective in preventing or suppressing the major
symp-toms of allergic rhinitis. Corticosteroids are administered by
metered-spray devices. If the nasal passages are blocked, a topical
decongestant can be used to clear the passages before the adminis-tration of
the intranasal corticosteroid. Patients must be aware that full benefit may not
be achieved for several days to 2 weeks. Ad-verse effects of intranasal
corticosteroids are mild and include dry-ing of the nasal mucosa and burning
and itching sensations caused by the vehicle used to administer the medication.
Systemic effects are more likely with dexamethasone. Recommended use of this
medication is limited to 30 days. Beclomethasone, budesonide, flu-nisolide,
fluticasone, and triamcinolone are deactivated rapidly after absorption, so
they do not achieve significant blood levels. Corticosteroids suppress host
defenses, so they must be used with caution in patients with tuberculosis or
untreated bacterial infec-tions of the lungs. Patients on corticosteroids are
at risk for infec-tion and for suppression of typical manifestations of
inflammation because host defenses are compromised. Inhaled corticosteroids do
not affect the immune system to the same degree as systemic cor-ticosteroids
(ie, oral corticosteroids). As corticosteroids are inhaled into the upper
respiratory tract, tuberculosis or untreated bacte-rial infections of the lungs
may become apparent and progress. Whenever possible, patients with tuberculosis
and other bacterial infections of the lungs should avoid inhaled
corticosteroids.
Oral and parenteral corticosteroids are used
when conven-tional therapy has failed and symptoms are severe and of short
du-ration. They can control symptoms of allergic reactions such as hay fever,
medication-induced allergies, and allergic reactions toinsect stings. Because
the response to corticosteroids is delayed, they have little or no value in
acute therapy for severe reactions such as anaphylaxis. Patients who receive
corticosteroids must be cautioned not to stop taking the medication suddenly or
without specific instructions from the physician. The patient is also
in-structed about side effects, which include fluid retention, weight gain,
hypertension, gastric irritation, glucose intolerance, and adrenal suppression.
IMMUNOTHERAPY
Allergen desensitization (allergen
immunotherapy, hyposensitiza-tion) is primarily used to treat IgE-mediated
diseases by injections of allergen extracts. This type of therapy provides an
adjunct to symptomatic pharmacologic therapy and can be used when aller-gen
avoidance is not possible (Parslow et al., 2001). Specific im-munotherapy has
been used in the treatment of allergic disorders for about 100 years. It
consists of administering increasing con-centrations of extracts of specific
allergens over a long period (Kay, 2001b). Goals of immunotherapy include
reducing the level of circulating IgE, increasing the level of blocking
antibody IgG, and reducing mediator cell sensitivity. Immunotherapy has been
most effective for ragweed pollen; however, treatment for grass, tree pollen,
cat, and house dust mite allergens has also been effective.
Correlation of a positive skin test with a
positive allergy his-tory is an indication for immunotherapy if the allergen
cannot be avoided. The value has been fairly well established in instances of
allergic rhinitis and bronchial asthma that are clearly due to sen-sitivity to
one of the common pollens, molds, and household dust. Although helpful in most
patients, immunotherapy does not cure the condition. Before immunotherapy is
initiated, the patient must understand what to expect and the importance of
continuing therapy for several years. When skin tests are per-formed, the
results are correlated with clinical manifestations; treatment is based on the
patient’s needs rather than on skin tests.
The most common method of treatment is the
serial injection of one or more antigens that are selected in each particular
case on the basis of skin tests. This method provides a simple and ef-ficient
technique for identifying IgE antibodies to specific anti-gens. Specific
treatment consists of injecting extracts of the pollens or mold spores that
cause symptoms in a particular pa-tient. Injections begin with very small amounts
and are gradually increased, usually at weekly intervals, until a maximum
tolerated dose is attained. Maintenance booster injections are given at 2- to
4-week intervals, frequently for a period of several years, before maximum
benefit is achieved There are three methods of injection therapy: coseasonal,
pre-seasonal, and perennial. When treatment is given on a coseasonal basis,
therapy is initiated during the season in which the patient experiences
symptoms. This method has been proved ineffective and is used infrequently.
Also, there is an increased risk of sys-temic reactions. Preseasonal therapy
injections are given 2 to 3 months before symptoms are expected, allowing time
for hypo-sensitization to occur. This treatment is discontinued after the
season begins. Perennial therapy is administered all year round, usually on a
monthly basis, and is the preferred method because it has more effective,
longer-lasting results.
Any
patient who receives specific immunotherapy is at risk for general, and
potentially fatal, anaphylaxis. This occurs most fre-quently at the induction
or “up-dosing” phase. Attempts have been made to minimize the risk of systemic
reactions by pre-treating allergen extracts with agents such as formaldehyde.
This approach decreases the binding of the allergen by IgE, but it also results
in decreased immunogenicity (Kay, 2001b).
Because of the risk for anaphylaxis,
injections should not be given by a lay person or by the patient. The patient
remains in the office or clinic for at least 30 minutes after the injection and
is ob-served for possible systemic symptoms. If a large, local swelling
de-velops at the injection site, the next dose should not be increased, because
this may be a warning sign of a possible systemic reaction.
Therapeutic
failure is evident when a patient does not experi-ence a decrease of symptoms
within 12 to 24 months, fails to de-velop increased tolerance to known
allergens, and cannot decrease the use of medications to reduce symptoms.
Potential causes of treatment failure include misdiagnosis of allergies,
inadequate doses of allergen, newly developed allergies, and inadequate
en-vironmental controls.
Related Topics