Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Allergic Disorders
Anaphylaxis - Allergic Disorders
ANAPHYLAXIS
Anaphylaxis is a clinical response to an
immediate (type I hyper-sensitivity) immunologic reaction between a specific
antigen and an antibody. The reaction results from IgE antibody. An
ana-phylactic reaction can be triggered by exposure to an antigen through
inhalation, injection, ingestion, or skin contact. It is a se-vere,
life-threatening allergic reaction. It is estimated that 3.3 to 43 million
persons in the United States (1.24% to 16.8% of the population) are at risk for anaphylaxis
(Neugut, Ghatak & Miller, 2001).
Pathophysiology
Anaphylaxis
is caused by the interaction of a foreign antigen with specific IgE antibodies
found on the surface membrane of mast cells and peripheral blood basophils. The
subsequent re-lease of histamine and other bioactive mediators causes
acti-vation of platelets, eosinophils, and neutrophils and the coagulation
cascade. Smooth muscle spasm, bronchospasm, mucosal edema and inflammation, and
increased capillary per-meability result. These systemic changes
characteristically pro-duce clinical manifestations within seconds or minutes
of antigen exposure (Neugut et al., 2001). Closely related to ana-phylaxis is
an anaphylactoid (anaphylaxis-like) reaction, which is described in Chart 53-2.
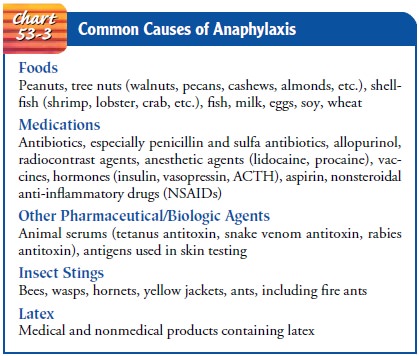
Substances
that most commonly cause anaphylaxis include foods, medications, insect stings,
and latex (Chart 53-3). Foods that are common causes of anaphylaxis include
peanuts, tree nuts, shellfish, fish, milk, eggs, soy, and wheat. Many
medications have been implicated in anaphylaxis. Those that are most frequently
reported include antibiotics (including penicillin), radiocontrast agents,
intravenous anesthetics, aspirin and other nonsteroidal anti-inflammatory drugs
(NSAIDs), and opioids. Antibiotics and radiocontrast agents cause the most
serious anaphylactic reac-tions, producing reactions in about 1 of every 5,000
exposures. Penicillin is the most common cause of anaphylaxis and accounts for
about 75% of fatal anaphylactic reactions in the U.S. each year (Neugut et al.,
2001).
Clinical Manifestations
Anaphylactic
reactions may be categorized as mild, moderate, and severe systemic reactions.
The time from exposure to the antigen to onset of symptoms is a good indicator
of the severity of the re-action: the faster the onset, the more severe the
reaction (Neugut et al., 2001).
Mild
systemic reactions consist of peripheral tingling and a sensation of warmth,
possibly accompanied by fullness in the mouth and throat. Nasal congestion,
periorbital swelling, pruri-tus, sneezing, and tearing of the eyes can also be
expected. Onset of symptoms begins within the first 2 hours of exposure.
Moderate systemic reactions may include flushing, warmth, anxiety, and itching in addition to any of the above symptoms.
More
serious reactions include bronchospasm and edema of the airways or larynx with
dyspnea, cough, and wheezing. The onset of symptoms is the same as for a mild
reaction.
Severe systemic reactions have an abrupt
onset with the same signs and symptoms described above. These progress rapidly
to bronchospasm, laryngeal edema, severe dyspnea, cyanosis, and hy-potension.
Dysphagia (difficulty swallowing), abdominal cramp-ing, vomiting, diarrhea, and
seizures can also occur. Cardiac arrest and coma may follow.
Prevention
Strict
avoidance of potential allergens is an important preventive measure for the
patient at risk for anaphylaxis (Neugut et al., 2001). Patients at risk for
anaphylaxis from insect stings should avoid areas populated by insects and
should use appropriate clothing, insect repellent, and caution to avoid further
stings.
If avoidance of exposure to allergens is
impossible, adminis-tration of epinephrine is a critical measure to prevent an
anaphy-lactic reaction. People sensitive to insect bites and stings, those who
have experienced food or medication reactions, and those who have experienced
idiopathic or exercise-induced anaphylac-tic reactions should always carry an
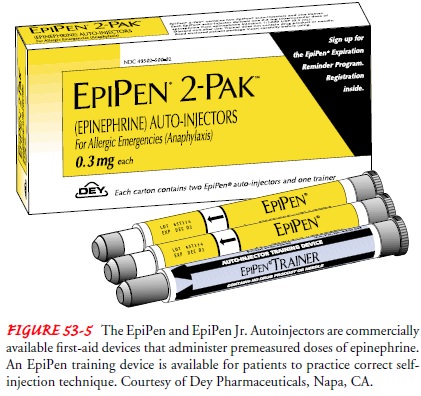
emergency kit that contains epinephrine. The EpiPen from Dey Pharmaceuticals is
a com-mercially available first-aid device that delivers premeasured doses of
0.3 mg (Epipen) and 0.15 mg (Epipen Jr.) of epinephrine (Fig. 53-5). The
autoinjection system requires no preparation, and the self-administration
technique is uncomplicated. The patient must be given an opportunity to
demonstrate the correct tech-nique for use; an Epipen training device is available.
Verbal and written information about the emergency kit, as well as strategies
to avoid exposure to threatening allergens, must also be provided.
Screening for allergies before a medication is prescribed or first administered is an important preventive measure. A careful his-tory of any sensitivity to suspected antigens must be obtained be-fore administering any medication, particularly in parenteral form, because this route is associated with the most severe ana-phylaxis. Nurses caring for patients in any setting (hospital, home, outpatient diagnostic testing sites, long-term care facilities) must assess patients’ risk for anaphylactic reactions. The patient is asked about previous exposure to contrast agents used for diagnostic tests and any allergic reactions, as well as reactions to any medications, foods, insect stings, and latex.
Persons predisposed to anaphylaxis should wear
some form of identification, such as a medical alert bracelet, naming allergies
to medications, food, and other substances.
People who are allergic to insect venom may
require venom im-munotherapy, which is used as a control measure and not a
cure. Immunotherapy following an insect sting is very effective in re-ducing
the risk of anaphylaxis from future stings (Neugut et al., 2001).
Insulin-allergic diabetic patients and penicillin-sensitive patients may
require desensitization. Desensitization is based on controlled anaphylaxis,
with a gradual release of mediators. Pa-tients who undergo desensitization are
cautioned that there should be no lapses in therapy, because this may lead to
the reappearance of an allergic reaction when the medication is reinstituted.
Medical Management
Management depends on the severity of the
reaction. Initially, respiratory and cardiovascular functions are evaluated. If
the pa-tient is in cardiac arrest, cardiopulmonary resuscitation is
insti-tuted. Oxygen is provided in high concentrations during cardiopulmonary
resuscitation or when the patient is cyanotic, dyspneic, or wheezing.
Epinephrine, in a 1 1,000 dilution, is ad-ministered subcutaneously in the
upper extremity or thigh and may be followed by a continuous intravenous
infusion. Antihis-tamines and corticosteroids may also be given to prevent
recur-rences of the reaction and to treat urticaria and angioedema. To maintain
blood pressure and normal hemodynamic status, IV flu-ids (ie, normal saline
solution), volume expanders, and vasopres-sor agents are given. In patients
with episodes of bronchospasm or a history of bronchial asthma or chronic
obstructive pul-monary disease, aminophylline and corticosteroids may also be
administered to improve airway patency and function. If hy-potension is
unresponsive to vasopressors, intravenous glucagon may be given for its acute
inotropic and chronotropic effects. Pa-tients with severe reactions are
observed closely for 12 to 14 hours. Because of the potential for recurrence,
patients with even mild reactions must be educated concerning this risk.
Nursing Management
If a
patient is experiencing an allergic response, the nurse’s initial action is to
assess the patient for signs and symptoms of anaphy-laxis. The nurse assesses
the airway, breathing pattern, and other vital signs. The patient is observed
for signs of increasing edema and respiratory distress. Prompt notification of
the physician and preparation for initiation of emergency measures (intubation,
administration of emergency medications, insertion of intra-venous lines, fluid
administration, oxygen administration) are important to reduce the severity of
the reaction and to restore car-diovascular function. The nurse documents the
interventions used and the patient’s response to treatment, vital signs, and
lab-oratory values.
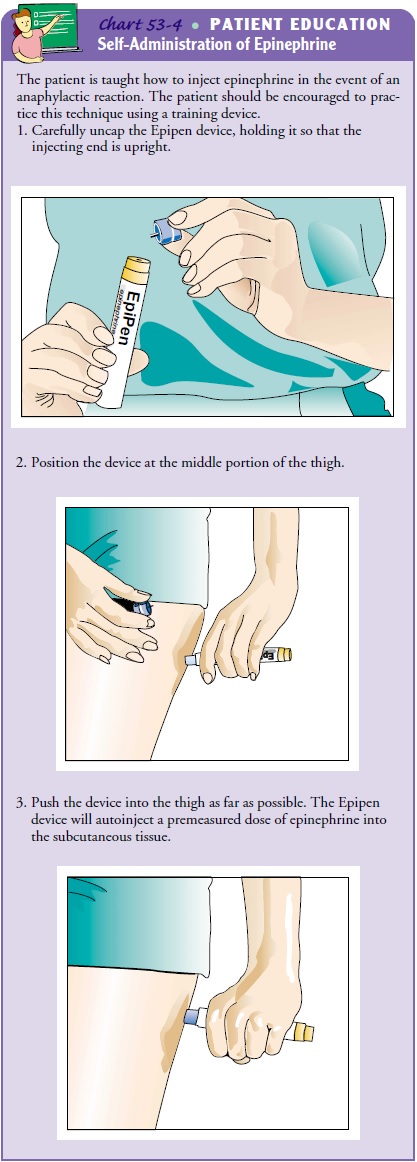
The
patient who has recovered from anaphylaxis needs an ex-planation of what
occurred and instruction about avoiding future exposure to antigens and
administering emergency medications to treat anaphylaxis. The patient must be
instructed about anti-gens that should be avoided and about other strategies to
prevent recurrence of anaphylaxis. All patients who have experienced an
anaphylactic reaction should receive a prescription for preloaded syringes of
epinephrine. The nurse instructs the patient and fam-ily in their use and has
the patient and family demonstrate correct administration (Chart 53-4).
Related Topics