Chapter: Obstetrics and Gynecology: Intrapartum Care
Normal Labor And Delivery: General Management
NORMAL LABOR AND DELIVERY
Ideally, a pregnant woman has a
principal, designated health care provider. Beginning with admission to the
labor and delivery area, the obstetric team monitors the patient’s progress.
Once the patient is in active labor, her provider should be readily available.
General Management
AMBULATION AND POSITION IN LABOR AND AT DELIVERY
Walking may be more comfortable
than being supine dur-ing early labor. Women in early labor are confined to bed
if they are too uncomfortable to move about safely or if care
Supine
labor is common in the United States. The left lateral position keeps the
uterus off the infe-rior vena cava; this obstructs venous return, thence
cardiac output, leading to hypotension (supine hypotensive syn-drome). Thedorsal
lithotomy positionis most commonly usedfor spontaneous and operative
vaginal delivery in the United “birthing chairs,” on labor balls, or in
variously configured tubs of warm water.
FLUID MANAGEMENT AND ORAL INTAKE
Because labor is associated with
decreased gastrointestinal peristalsis, there is concern about aspiration
during the administration of anesthesia. Patients in active labor should avoid
oral ingestion of anything except clear fluids (sips only), occasional ice
chips, and preparations for moisten-ing the mouth and lips.
When oral intake is not possible
or is insufficient, intravenous therapy with 1⁄2 normal saline or D5
1⁄2 normal saline is indicated. Normal saline can be used if
increased oncotic pressure is desired, but lactated fluids are gener-ally
contraindicated because of the metabolic acid deficit incurred by the lactate
administration.
EVALUATION OF FETAL WELL-BEING
Measurement of the fetal heart rate and its changes
dur-ing labor is the primary means of intrapartum assessment of fetal
well-being. This may be done by intermittent aus-cultation with a stethoscope or
hand-held Doppler, or by the use of electronic fetal monitoring. The method
chosen may depend on risk assessment at admission, the prefer-ence of the
patient and the obstetric staff, and department policy. Risk factors include
vaginal bleeding, acute abdom-inal pain, temperature >100.4°F, preterm labor or rupture of
membranes, hypertension, and nonreassuring fetal heart rate pattern.
In the absence of risk factors on
admission, the standard approach to fetal monitoring is to determine, evaluate,
and record the fetal heart rate every 30 minutes in the active phase in the
first stage of labor, and at least every 15 minutes in the second stage. In the
presence of risk factors, fetal sur-veillance should be performed using either
intermittent aus-cultation or continuous fetal monitoring. During the active
first stage of labor, auscultation should be performed every 15 minutes,
preferably before, during, and after a contrac-tion, and continuous monitoring
should be evaluated at least every 15 minutes. During the second stage of
labor, the fetal heart rate should be monitored every 5 minutes using either
the intermittent or continuous procedure. If electronic fetal monitoring is
used, an external tocodynamometer is initially used to assess uterine activity,
providing information regard-ing the frequency and duration of contractions,
but not their intensity. Electronic fetal monitoring is not necessary for a
low-risk term pregnancy.
Control of Pain
Management of discomfort and pain
during labor is an essential part of good obstetric practice. Some patients
tolerate pain by using techniques learned in childbirth preparation programs.
It is important that bedside staff be knowledgeable about these pain management
techniques and be supportive of the patient’s decisions. Unless
con-traindicated, pharmacologic analgesics to ameliorate pain of contractions
should be made available on request to women in labor.
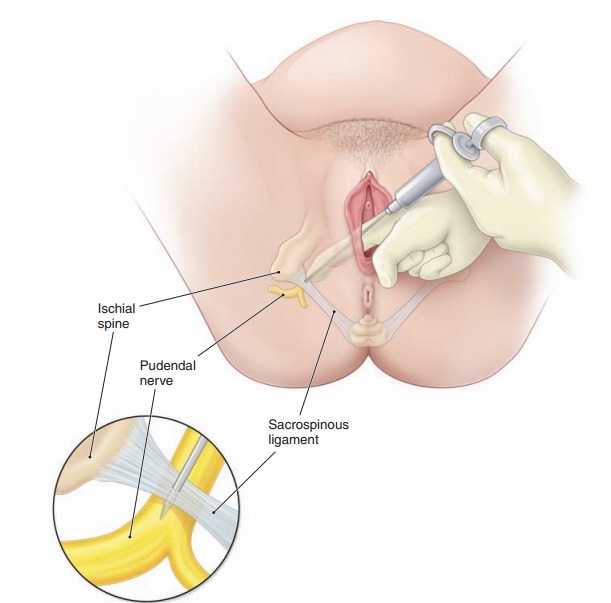
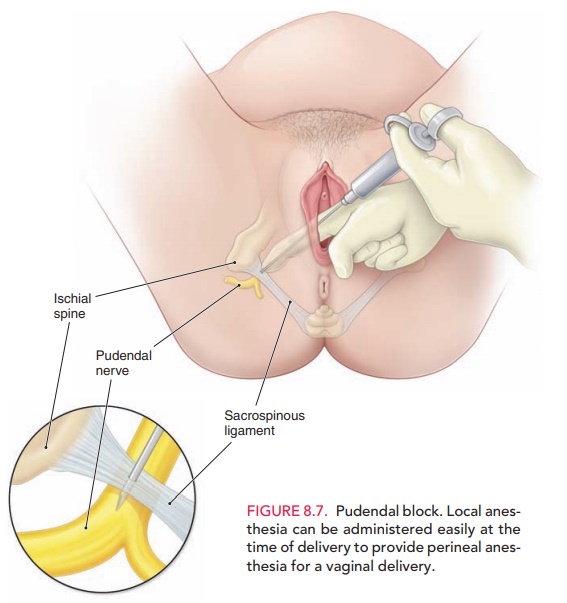
During the first stage of labor,
pain results from the contraction of the uterus and dilation of the cervix. This
pain travels along the visceral afferents, which accompany sympathetic nerves
entering the spinal cord at T-10, T-11, T-12, and L-1. As the fetal head
descends, there is also dis-tension of the lower birth canal and perineum. This
pain is transmitted along somatic afferents that comprise por-tions of the
pudendal nerves that enter the spinal cord at S-2, S-3, and S-4. To provide
relief from obstetric pain, the following methods of anesthesia and analgesia
are used.
· Epidural block: infusion
of local anesthetics or narcoticsthrough a catheter into the epidural space.
The most effective form of intrapartum pain relief in the United States, it can
be used in either vaginal or abdominal deliv-eries and in postpartum procedures
such as tubal ligation.
· Spinal anesthesia: a single
injection of anesthetic
· Combined spinal–epidural: combination
of the abovetwo techniques
· Local block: local
injection of anesthetic into theperineum or vagina. A pudendal block is a local block (Fig. 8.7).
· General anesthesia: inhaled
or intravenous administra-tion of anesthetic agents that results in a loss of
mater-nal consciousness. This technique is reserved only for cesarean
deliveries in selected cases.
To determine which method of
obstetric pain control should be used, the positive and negative aspects of
each should be considered. Of the regional modes of analgesia, epidural
anesthesia is superior to spinal anesthesia in that it can be left as a
continuous source of analgesia and anesthe-sia during both the labor and delivery
process. The advan-tage of this technique is its ability to provide analgesia
during labor as well as excellent anesthesia for delivery, yet main-tain the
patient’s sense of touch, facilitating participation in the birth process.
Spinal anesthesia provides good pain relief for procedures of limited duration,
such as cesarean delivery or vaginal delivery when labor is rapidly
progressing. Combined spinal–epidural anesthesia has advantages: the epidural
catheter to titrate medications throughout labor and the rapid onset associated
with spinal techniques. All of these types of regional anesthesia may be
associated with a postdural puncture headache. However, combined
spinal–epidural anesthesia avoids the risk of spinal headache in the mother and
reduces the risk of sympathetic blockade, which could lead to hypotension.
There is also less motor blockade than with spinal anesthesia. Local block may
pro-vide anesthesia for episiotomy and repair of vaginal and per-ineal
lacerations; however, paracervical block may result in fetal bradycardia.
General anesthesia is associated with complications such as maternal aspiration
and neonatal depression. If properly administered, it is effective for most
cesarean deliveries, but regional anesthesia is preferable.
Related Topics