Chapter: Obstetrics and Gynecology: Intrapartum Care
Evaluation For Labor
EVALUATION FOR LABOR
Patients should be instructed to
contact their health care provider for any of the following reasons: (1) if
their con-tractions occur approximately every 5 minutes for at least 1 hour,
(2) if there is a sudden gush of fluid or a constant leakage of vaginal fluid
(suggesting rupture of membranes),
if there is any significant
vaginal bleeding, or (4) if there is significant decrease in fetal movement.
Initial Evaluation
At the time of initial evaluation, the prenatal records are reviewed to (1) identify complications of pregnancy up to that point, (2) confirm gestational age to differentiate preterm labor from labor in a term pregnancy, and review pertinent laboratory information. A focused history helps in determining the nature and frequency of the patient’s contractions, the possibility of spontaneous rupture of membranes or significant bleeding, or changes in maternal or fetal status.
A focused review of systems should look
for common complications of pregnancy resulting in altered labor management. A
limited general physical examination is performed (with special attention to
vital signs), along with the abdominal and pelvic examinations. If contractions
occur during this physical examination, they may be palpated for intensity and
duration by the examining physician. Auscultation of fetal heart tones is also
of critical importance, particularly immediately fol-lowing a contraction, to
determine the possibility of any fetal heart rate deceleration. A limited
transabdominal ultrasound may also be useful if there is a question of fetal
lie, placental location, or decreased amniotic fluid volume or other
abnormalities.
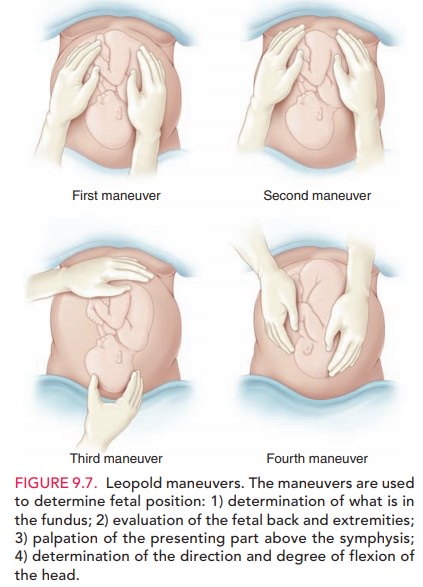
The
initial examination of the patient’s abdomen may be accomplished using Leopold maneuvers, a series of four
palpations of the fetus through the abdominal wall that helps accurately
determine fetal lie, presentation, and position (see Figure 9.7).
Lie is the
relation of the long axis of the fetus with thematernal long axis. It is
longitudinal in 99% of cases, occa-sionally transverse, and rarely oblique
(when the axes cross at a 45-degree angle, usually converting to transverse or
longitudinal lie during labor). Presentation
is determined by the “presenting part,” that is, that portion of the fetus
lowest in the birth canal, palpated during the examination. For example, in a
longitudinal lie, the presenting part is either breech or cephalic. The most
common cephalic presentation is the one in which the head is sharply flexed
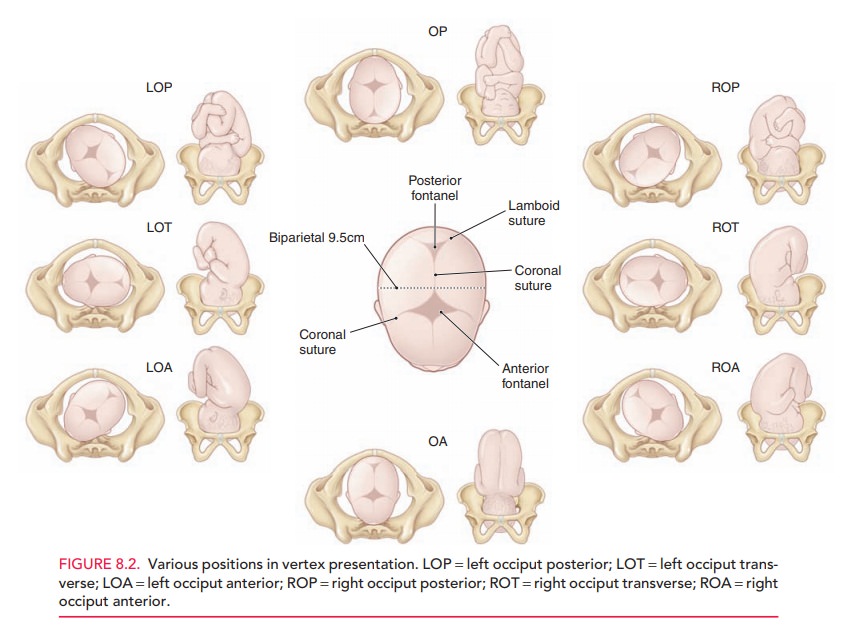
onto the fetal chest such that the occiput or vertex presents. Position is the relation of the fetal
presenting part to the right or left side of the maternal pelvis (Fig. 8.2).
The four Leopold maneuvers (see
Fig. 9.7) include the following, facilitating several obstetric measurements:
1.
Determining what occupies the
fundus. In a longitudi-nal lie, the fetal head is differentiated from the fetal
breech, the latter being larger and less clearly defined.
2.
Determining location of small
parts. Using one hand to steady the fetus, the fingers on the other hand are
used to palpate either the firm, long fetal spine or the various shapes and
movements indicating fetal hands and feet.
3.
Identifying descent of the
presenting part. Suprapubic palpation identifies the presenting part as the
fetal head, which is relatively mobile, or a breech, which moves the entire
body. The extent to which the presenting part is felt to extend below the
symphysis suggests the station of the presenting part.
4.
Identifying the cephalic
prominence. As long as the cephalic prominence is easily palpable, the vertex
is not likely to have descended to zero station.
Palpation of the uterus during a
contraction may also be helpful in determining the intensity of that particular
con-traction. The uterine wall is not easily indented with firm palpation
during a true contraction, but may be indented during a Braxton Hicks
“contraction.”
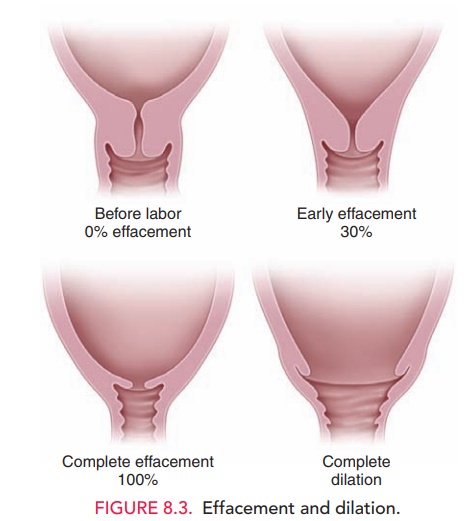
A digital vaginal examination
allows the examiner to determine the consistency and degree of effacement and
degree of dilation of the cervix. This examination should be avoided in women
with premature rupture of membranes or vaginal bleeding. Effacementis the shortening of the cervicalcanal from
a length of about 2 cm to a mere circular orifice with almost paper-thin edges.
Effacement is expressed as a percent of thinning from a perceived uneffaced
state (Fig. 8.3).
A cervix that is not effaced, but is softened,
is more likely to change with contractions than one that is firm, as it is
earlier in preg-nancy. If the cervix is not significantly effaced, it may also
be evaluated for its relative position, that is, anterior, midposi-tion, or
posterior in the vagina. A cervix that is palpable ante-rior in the vagina is
more likely to undergo change in labor sooner than one found in the posterior
portion of the vagina. This suggests that the presenting part has descended
into the pelvis, creating more pressure on the cervix, thereby rotating it
anteriorly. With more effective force on the lower uterine segment,
contractions would cause a greater change in dilation and effacement of the
cervix.
Fetal Station
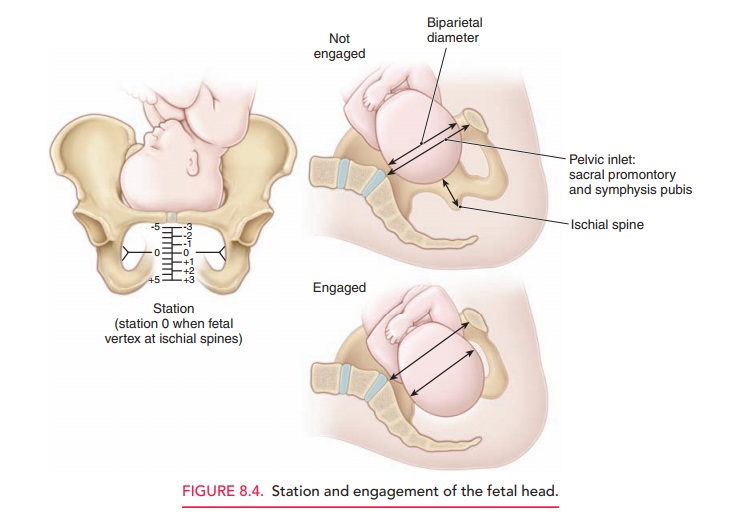
Fetal station is determined by
identifying the level of the fetal presenting part in the birth canal in
relation to the ischial spines which are located approximately halfway between
the pelvic inlet and the pelvic outlet (Fig. 8.4). If the presenting part has reached the level
of the ischial spines, it is termed zero station. The distance between the
ischialspines to the pelvic inlet above and the distance from the spines to the
pelvic outlet below are divided into fifths, andthese measurements are used to
further define station. These divisions represent centimeters above and below
the ischial spines. Thus, as the presenting fetal part descends from the pelvic
inlet toward the ischial spines, the designa-tion is −5, −4, −3, −2, −1, then 0 station. Below the
ischial spines, the presenting fetal part passes +1, +2, +3, +4, with +5 station corresponding to the
fetal head being visible at theintroitus. The clinical significance of the
fetal head present-ing at zero station is that the biparietal diameter of the
fetal head, the greatest transverse diameter of the fetal skull, is assumed to
have negotiated the pelvic inlet.
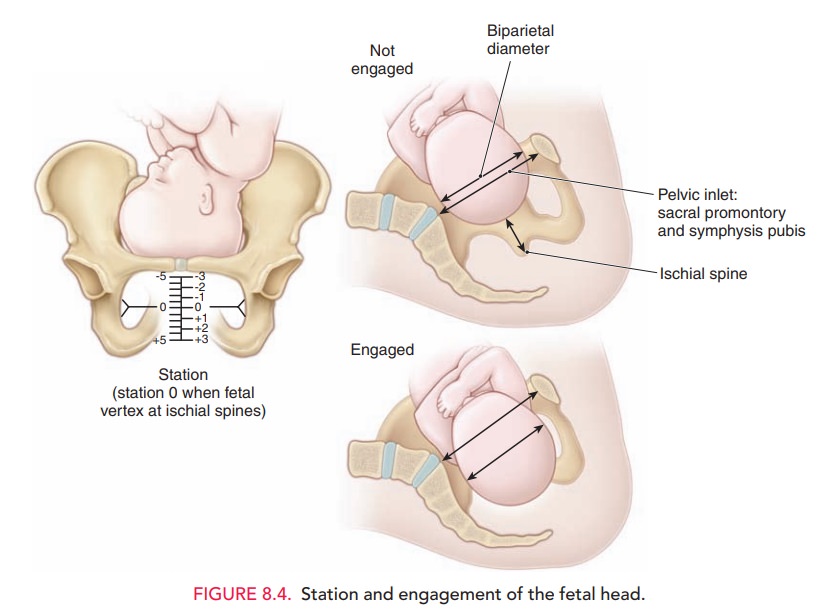
The fetal
head is said to be engaged at zero station, a crucial functional “landmark” in
the labor path.
However, caput succedaneum,
cephalohematoma, and molding of the fetal head may mislead the examiner to a
greater station than has been obtained.
Related Topics