Chapter: Ophthalmology: Conjunctiva
Noninfectious Conjunctivitis
Noninfectious Conjunctivitis
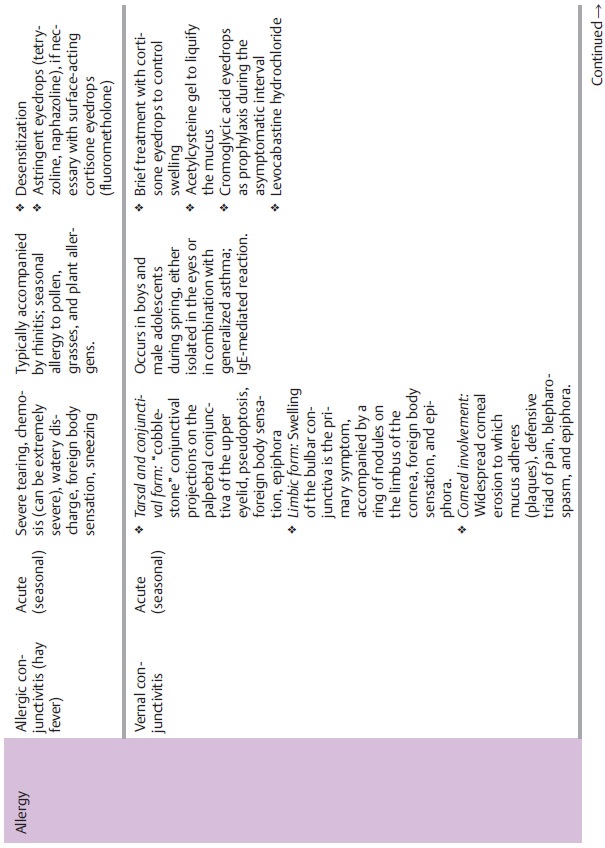
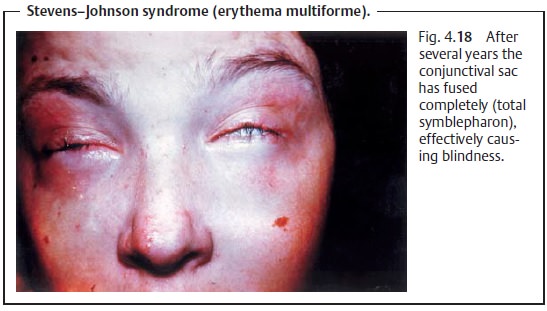
Table 4.4 provides an overview of pathogens, symptoms,
and treatments of noninfectious conjunctivitis.
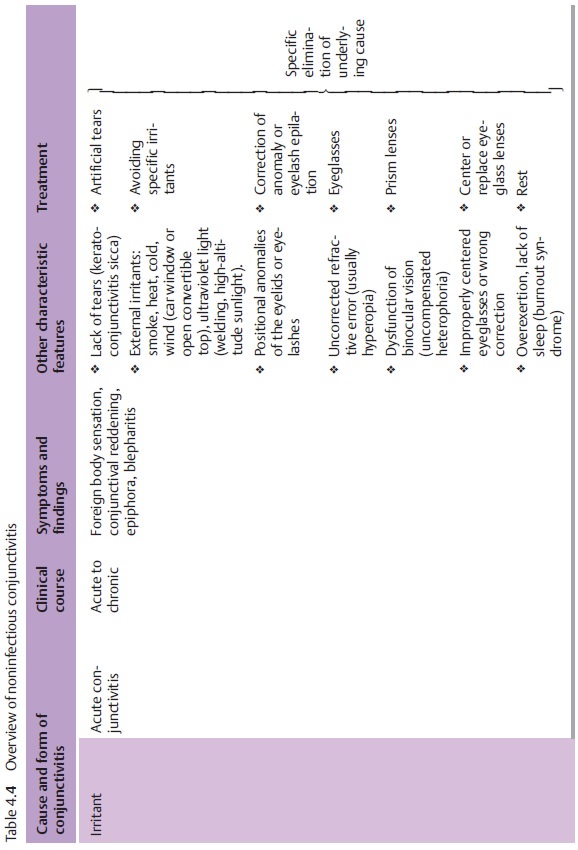
Acute conjunctivitis is frequently attributable to a series of external irri-tants or
to dry eyes (conjunctivitis sicca). The disorder is unpleasant butbenign. Primary symptoms include foreign-body
sensation, reddening of theeyes of varying severity, and epiphora. Therapy
should focus on eliminating the primary irritant and treating the symptoms.
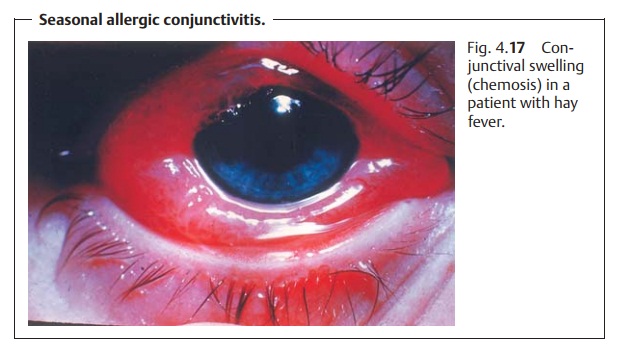
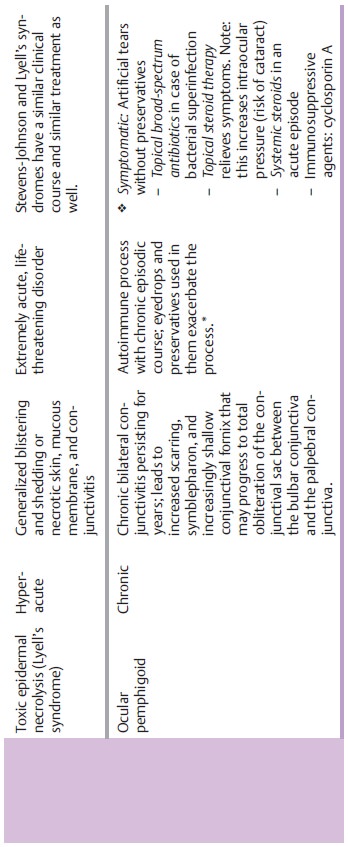
Acute conjunctivitis should be distinguished from the group of allergicforms of conjunctivitis, which can be due to seasonal influences and oftenaffect the nasal mucosa. Examples include allergic conjunctivitis (hay fever; Fig. 4.17) and vernal conjunctivitis. In giant papillary conjunctivitis, the inflam-mation is triggered by a foreign body (hard or soft contact lenses. There may also be an additional chronic microbial irritation such microbial contamina-tion of contact lenses. Phlyctenular keratoconjunctivitis is a delayed allergicreaction to microbial proteins or toxins (staphylococcal inflammation). Thisdisease occurs frequently in atopic individuals and is promoted by poor hygiene. The cardinal rule in allergic conjunctivitis is to avoid the causative agent. Desensitization should be performed as a prophylactic measure by a dermatologist or allergist. Long-term treatment includes cromoglycic acid eyedrops to prevent mast cell degranulation. Treatment of acute allergic conjunctivitisconsists of administering cooling compresses, artificial tears withpreservatives, astringent eyedrops (tetryzoline and naphazoline), and, if nec-essary, surface-acting cortisone eyedrops (fluorometholone).
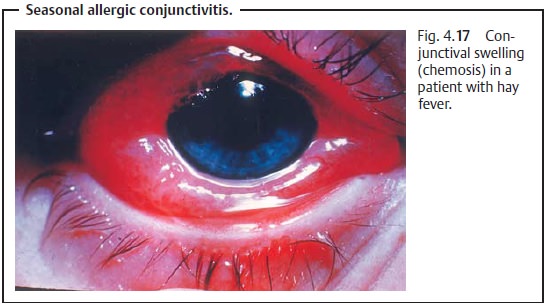
Ocular-mucocutaneous syndromes such asStevens–Johnson
syndrome(erythema multiforme), Lyell’s
syndrome (toxic epidermal necrolysis), and ocular pemphigoid (progressive shrinkage of the conjunctiva) are
clinical syn-dromes that involve multiple toxic and immunologic causative
mechanisms. The clinical course of the disorder is severe, therapeutic options
are limited, and the prognosis for eyesight is poor (Fig. 4.18).
junctivitisconsists of administering cooling compresses, artificial tears
withpreservatives, astringent eyedrops (tetryzoline and naphazoline), and, if
nec-essary, surface-acting cortisone eyedrops (fluorometholone).
Ocular-mucocutaneous syndromes such asStevens–Johnson syndrome(erythema multiforme), Lyell’s syndrome (toxic epidermal necrolysis), and ocular pemphigoid (progressive shrinkage of the conjunctiva) are clinical syn-dromes that involve multiple toxic and immunologic causative mechanisms. The clinical course of the disorder is severe, therapeutic options are limited, and the prognosis for eyesight is poor (Fig. 4.18).
Conjunctival irritation symptoms can occur withGraves’
orbitopathy,gout, rosacea, neurodermatitis, erythema multiforme, Sjögren’s
syndrome, and Reiter’s syndrome (triad:
conjunctivitis or iridocyclitis, urethritis, and polyar-thritis). Parinaud’s oculoglandular syndrome
describes a clinical syndrome of widely varied etiology. Granulomatous conjunctivitis always occurs uni-laterally and in
conjunction with swollen preauricular and submandibularlymph nodes in the
presence of tuberculosis, syphilis, viruses, bacteria, fungi, and parasites.
The excisional biopsy of the conjunctival granuloma is itself part of the treatment of granulomatous conjunctivitis.
The specific medica-tions will depend on the underlying disorder.
Related Topics