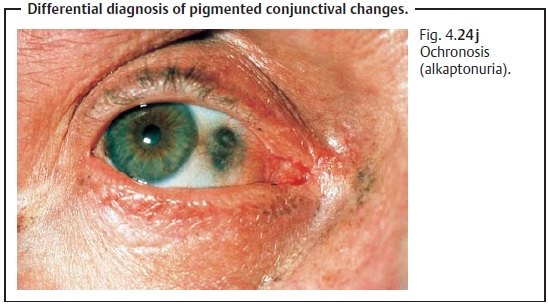
Chapter: Ophthalmology: Conjunctiva
Melanocytic Conjunctival Tumors
Melanocytic Conjunctival Tumors
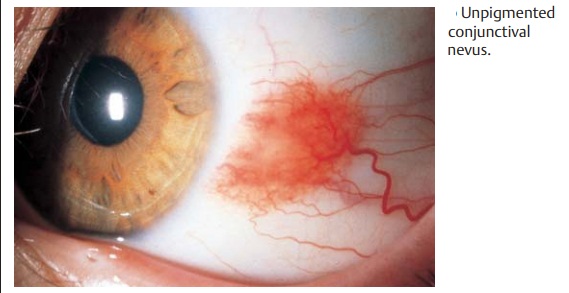
Conjunctival Nevus
Birthmarks can occur on the conjunctiva as on
the skin. They are usually located near the limbus in the temporal portion of
the palpebral fissure, less frequently on the lacrimal caruncle. These benign, slightly raised epithelial or
subepithelial tumors are congenital.
Fifty percent of nevi contain hollow cys-tic spaces (pseudocysts) consisting of
conjunctival epithelium and goblet cells. Conjunctival nevi may be pigmented
(Fig. 4.24a) or unpigmented (Fig. 4.24b), and they may increase in size as the patient
grows older. Increas-ing pigmentation of the nevus as a result of hormonal
changes during preg-nancy or puberty or from exposure to sunlight can simulate
an increase in the size of the nevus, as can proliferation of the pseudocysts. Conjunctival nevi candegenerate into
conjunctival melanomas (50% of conjunctival melanomasdevelop from a nevus).
Therefore, complete excision and histologic diagnostic studies are indicated if
the nevus significantly increases in size or shows signs of inflammation.
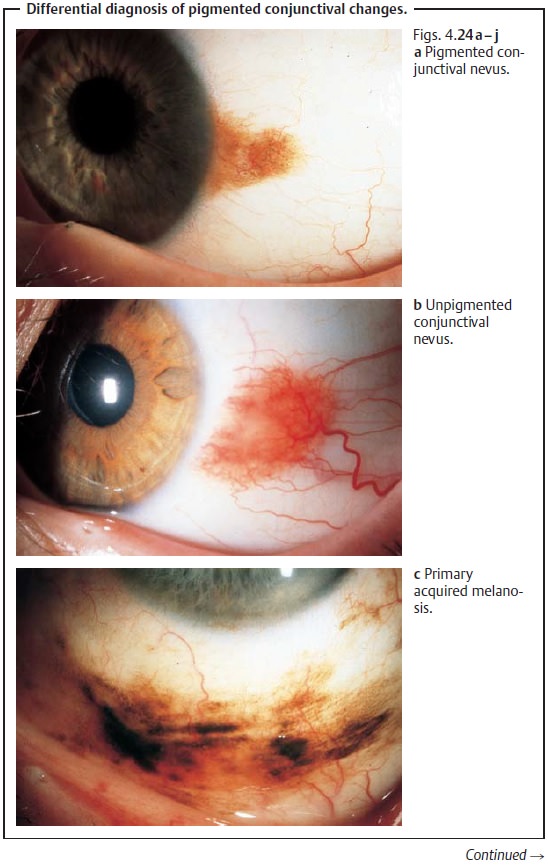
Photographs should always be taken during
follow-up examinations of conjunctival nevi. Small clear watery inclusion cysts
are always a sign of a conjunctival nevus.
Conjunctival Melanosis
Definition
Conjunctival melanosis is a pigmented
thickening of the conjunctival epi-thelium (Fig. 4.24c).
Epidemiology: Conjunctival melanosis is rare like all potentially malignantor
malignant tumors of the conjunctiva.
Etiology: Unclear.
Symptoms: Acquired conjunctival melanosis usually occurs after the age of
Typical symptoms include irregular diffuse pigmentation and
thickening of the epithelium that may “come and go.”
Diagnostic considerations: Acquired conjunctival melanosis is mobile withthe conjunctiva
(an important characteristic that distinguishes it from con-genital melanosis).
It requires close observation with follow-up examinations every six months as
it can develop into a malignant melanoma
.Differential diagnosis: This disorder should be distinguished frombenigncongenital melanosis (see below), which remains stable throughout thepatient’s lifetime and appears more bluish gray than brownish. In contrast to acquired melanosis, it is not mobile with the conjunctiva.
Treatment: Because the disorder occurs diffusely over a broad area,
treat-ment is often difficult. Usually it combines excision of the prominent
deeply pigmented portions (for histologic confirmation of the diagnosis) with
cryo-coagulation of the adjacent melanosis and in some cases with postoperative
radiation therapy.
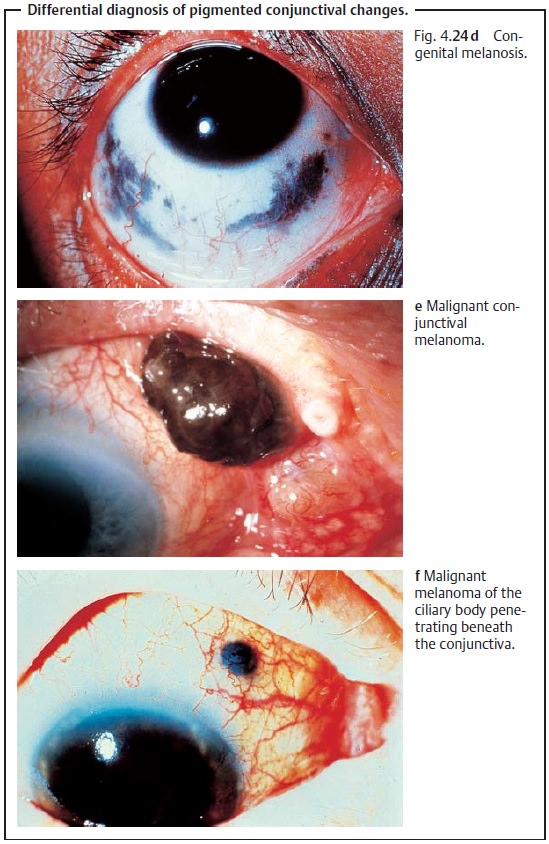
Clinical course and prognosis: About 50% of conjunctival melanomasdevelop from conjunctival melanosis
(the other 50% develop from a conjunc-tival nevus; see above). Conjunctival
melanomas are not usually as aggres-sively malignant as skin melanomas. The
radical resection required to remove the tumor can be a problem. Multiple
recurrences will produce significant conjunctival scarring that can result in
symblepharon with fusion of the eye-lid skin and conjunctiva. Where the tumor
has invaded the eyelids or the deeper portions of the orbit, orbital
exenteration will be unavoidable to completely remove the tumor.
Congenital Ocular Melanosis
Benign congenital melanosis (Fig. 4.24d) is subepithelial in the episclera.
Theconjunctival epithelium is not
involved. Pigmentation is bluish gray. In con-trast to acquired melanosis,
congenital melanosis remains stable
and station-ary throughout the
patient’s lifetime. In contrast to nevi and acquired mela-nosis, congenital
melanosis remains stationary when the conjunctiva above it is moved with
forceps. Congenital ocular melanosis can occur as an isolatedanomaly of the eye or
in association with skin pigmentations (oculodermalmelanosis or Ota’s
nevus). Although the tumor is benign, evidence suggests that malignant
melanomas in the choroid occur more frequently in patients with congenital
melanosis.
Related Topics