Chapter: Ophthalmology: Conjunctiva
Infectious Conjunctivitis
Infectious Conjunctivitis
The normal conjunctiva contains
microorganisms. Inflammation usually occurs as a result of infection from direct contact with pathogens (such as
from a finger, towel, or swimming pool) but also from complicating factors (such as a compromised immune system or
injury). There are significant regional differences in the spectrum of
pathogens. Table 4.2 provides an overview of pathogens, symptoms, and treatments.
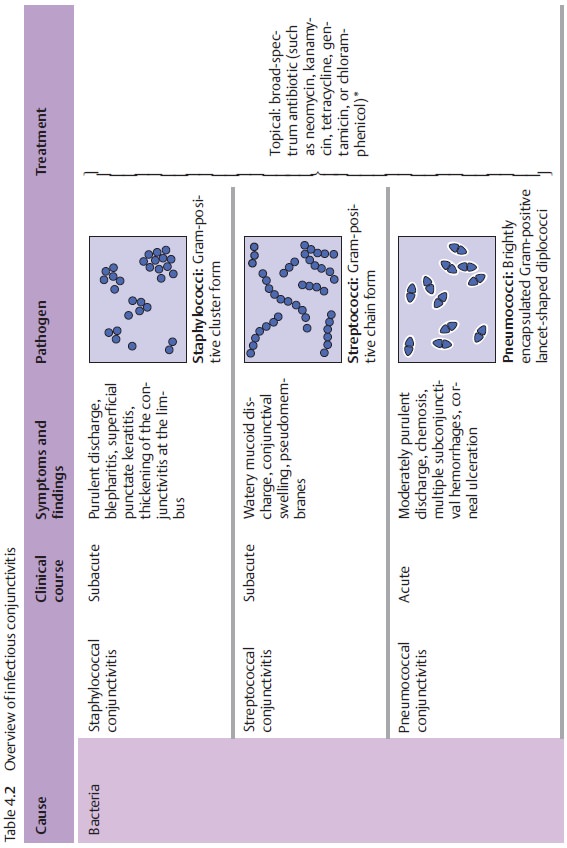
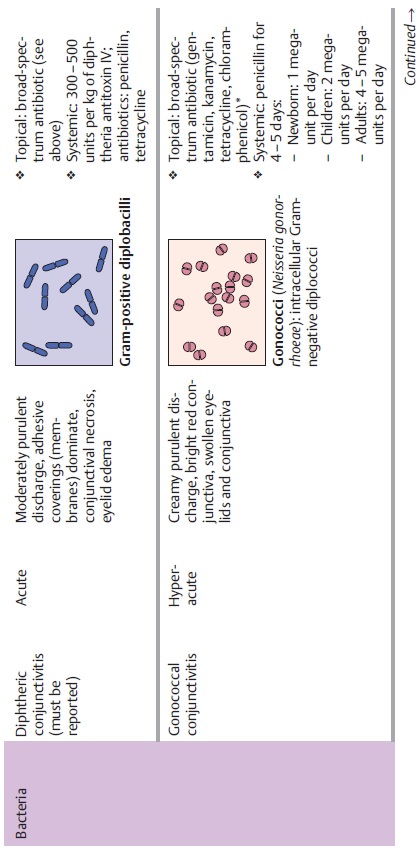
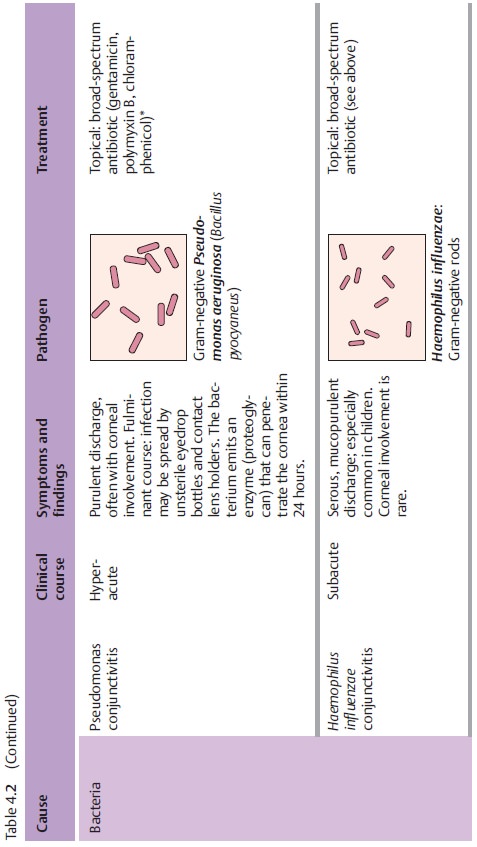
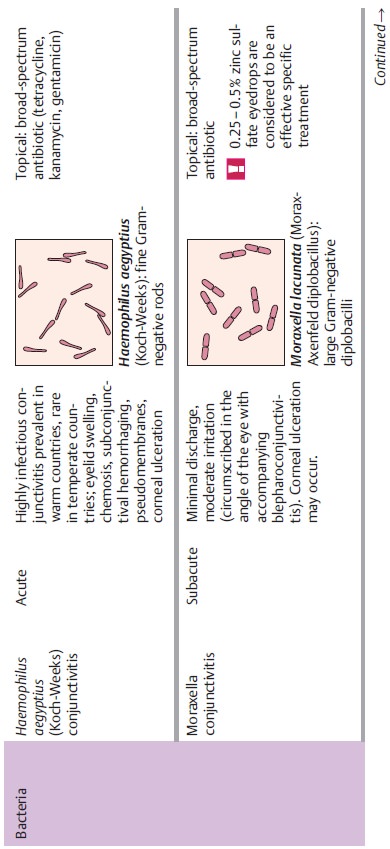
Bacterial Conjunctivitis
Epidemiology: Bacterial conjunctivitis is very frequently encountered.
Etiology: Staphylococcus, streptococcus, and pneumococcus infections
aremost common in temperate countries.
Symptoms: Typical symptoms include severe reddening, swelling of the
con-junctiva, and purulent discharge that leads to formation of yellowish
crusts.
Diagnostic considerations: Bacterial conjunctivitis can usually be reliablydiagnosed from
the presence of typical symptoms. Laboratory tests (conjunc-tival smear) are
usually only necessary when the conjunctivitis fails to respond to antibiotic
treatment.
Bacterial conjunctivitis is diagnosed on the
basis of clinical symptoms.
Smears are obtained only in severe, uncertain,
or persistent cases.
Treatment: Bacterial conjunctivitis usually responds very well to
antibiotictreatment. A wide range of well tolerated, highly effective antibiotic agents is available today.
Most of these are supplied as ointments (which are longer acting and suitable
for overnight therapy) and as eyedrops for topical
therapy. Substances include gentamicin, tobramycin, Aureomycin,
chloramphenicol,1 neomycin, polymyxin B in combination with bacitracin and
neomycin , Ter-ramycin, kanamycin, fusidic acid, ofloxacin, and acidamphenicol.1
Preparations that combine an antibiotic and cortisone can more rapidlyalleviate subjective symptoms
when findings are closely monitored. These include medications such as
gentamicin and dexamethasone; neomycin, polymyxin B, and dexamethasone; or
tetracycline, polymyxin B, and hydro-cortisone.
In severe, uncertain, or persistent cases
requiring microbiological exami-nation to identify the pathogen, treatment with
broad-spectrum antibiotics or topical antibiotic combination preparations that
cover the full range of Gram-positive and Gram-negative pathogens should begin
immediately. This method is necessary because microbiological identification of
the pathogen and resistance testing of the antibiotic are not always successful
and may require several days. It is not advisable to leave the conjunctivitis
untreated for this period.
In the presence of severe, uncertain, or
persistent conjunctivitis, treat-ment with broad-spectrum antibiotics or
topical antibiotic combination preparations should be initiated immediately,
even before the labora-tory results are available.
Clinical course and prognosis: Bacterial conjunctivitis usually responds wellto antibiotic
treatment and remits within a few days.
Chlamydial Conjunctivitis
Chlamydia are Gram-negative bacteria.
Inclusion Conjunctivitis
Epidemiology: Inclusion conjunctivitis isvery
frequentin temperate coun-tries. The incidence in western industrialized
countries ranges between 1.7% and 24% of all sexually active adults depending
on the specific population studied.
Etiology: Oculogenital infection (Chlamydia
trachomatisserotype D–K) isalso caused by direct contact. In the newborn
(see neonatal conjunctivitis), this occurs at birth through the cervical
secretion. In adults, it is primarily transmitted during sexual intercourse,
and rarely from infection in poorly chlorinated swimming pools.
Symptoms: The eyes are only moderately red and slightly sticky from
viscousdischarge.
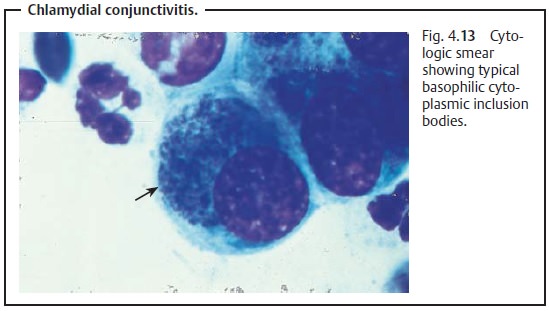
Diagnostic considerations: Tarsal follicles are observed typically on theupper and lower
eyelids, and pannus will be seen to spread across the limbus of the cornea. As
this is an oculogenital infection, it is essential to determine whether the
mother has any history of vaginitis, cervicitis, or urethritis if there is
clinical suspicion of neonatal infection. Gynecologic or urologic examination
is indicated in appropriate cases. Chlamydia may be detected in conjunctival
smears, by immunofluorescence, or in tissue cultures. Typical cytologic signs
include basophilic cytoplasmic inclusion bodies (Fig. 4.13).
Treatment: In adults, the disorder is treated with tetracycline or erythromy-cin eyedrops or ointment over a period of four to six weeks. The oculogenital mode of infection entails a risk of reinfection. Therefore, patients and sexual partners of treated patients should all be treated simultaneously with oral tetracycline. Children should be treated with erythromycin instead of tetracy-cline (see the table in the Appendix for side effects of medications).
Prognosis: The prognosis is good when the sexual partner is included in
ther-apy.
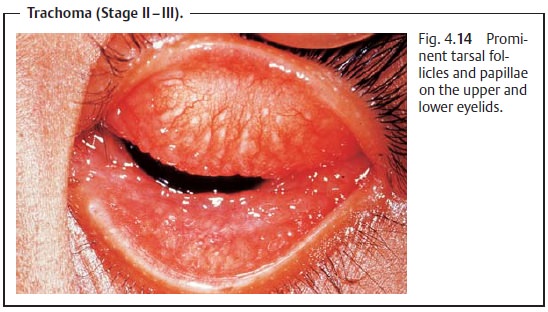
Trachoma
Trachoma (Chlamydia
trachomatis serotype A–C) is rare in temperate coun-tries. In endemic
regions (warm climates, poor standard of living, and poor hygiene), it is among
the most frequent causes of blindness (see Table 4.2 for symptoms, findings, and therapy). Left
untreated, the disorder progresses through four stages (Fig. 4.14):
❖ Stage I: Hyperplasia of the lymph follicles on the
upper tarsus.
❖ Stage II: Papillary hypertrophy of the upper tarsus, subepithelial
cornealinfiltrates, pannus formation, follicles on the limbus.
❖ Stages III and IV: Increasing scarring and symptoms of keratoconjunctivi-tis
sicca. The progression is entropion, trichiasis, keratitis, superinfection,
ulceration, perforation, and finally loss of the eye.
Viral Conjunctivitis
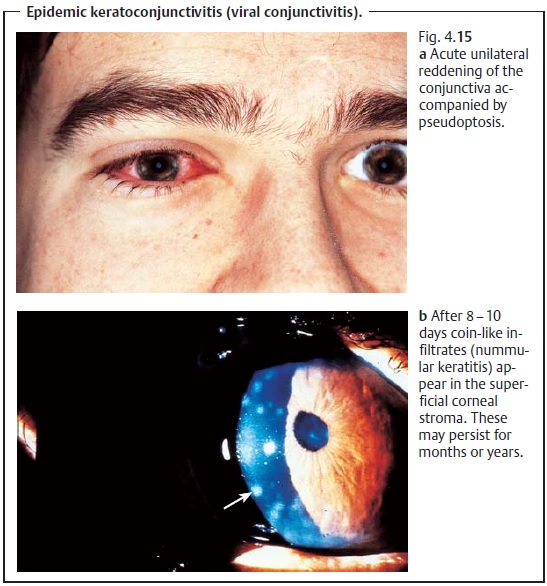
Epidemiology: The incidence ofepidemic keratoconjunctivitisis high ingeneral, and it is by far the most frequently encountered viral conjunctivitis (see Table 4.2)
Etiology: This highly contagious conjunctivitis is usually caused by type
18 or19 adenovirus and is spread by direct contact (see also prophylaxis; Figs.
4.15a and b). The incubation period is eight to ten days.
Symptoms: Onset is usually unilateral. Typical signs include severe
illacri-mation and itching accompanied by a watery mucoid discharge. The eyelid
and often the conjunctivitis are swollen. Patients often also have a moderate
influenza infection.
Diagnostic considerations: Characteristic findings include reddening andswelling of the plica semilunaris and lacrimal caruncle and nummular ker-atitis (Fig. 4.15b) after 8 – 15 days, during the healing phase..
Differential diagnosis: The disease runs a well defined clinical course that isnearly
impossible to influence and resolves after two weeks. No specific ther-apy is
possible. Treatment with artificial tears and cool compresses helps relieve
symptoms. Cortisone eyedrops should usually be avoided as they can compromise
the immune system and prolong the clinical symptoms.
Prophylaxis: This is particularly important. Because the disease is spread bycontact,
the patient should refrain from rubbing his or her eyes despite a severe
itching sensation and avoid direct contact with other people such as shaking
hands, sharing tools, or using the same towels or wash cloths, etc.
Special hygiene precautions should be taken when examining patients with
epidemic keratoconjunctivitis in ophthalmologic care facilities and doc-tors’
offices to minimize the risk of infecting other patients. Patients with
epi-demic keratoconjunctivitis should not be seated in the same waiting room as
other patients. They should not be greeted with a handshake, and they should be
requested to refrain from touching objects where possible. Examination should
be by indirect means only, avoiding applanation tonometry, contact lens examination,
or gonioscopy. After examination, the examiner should clean his or her hands
and the work site with a surface disinfectant.
Neonatal Conjunctivitis
Epidemiology: Approximately 10% of the newborn contract conjunctivitis.
Etiology (Table 4.3): The most
frequent pathogens areChlamydia,followedby
gonococci. Neonatal conjunctivitis is less frequently attributable to otherbacteria such as Pseudomonas aeruginosa, Haemophilus, Staphylococcus aureus and
Streptococcus pneumoniae, or to herpes simplex. The infectionoccurs at
birth. Chlamydia infections are particularly important because they are among
the most common undetected maternal genital diseases in Europe, affecting 5% of
all pregnant women. Neonatal conjunctivitis some-times occurs as a result of Credé’s
method of prophylaxis with silver nitrate, required by law in Europe to prevent
bacterial infection.
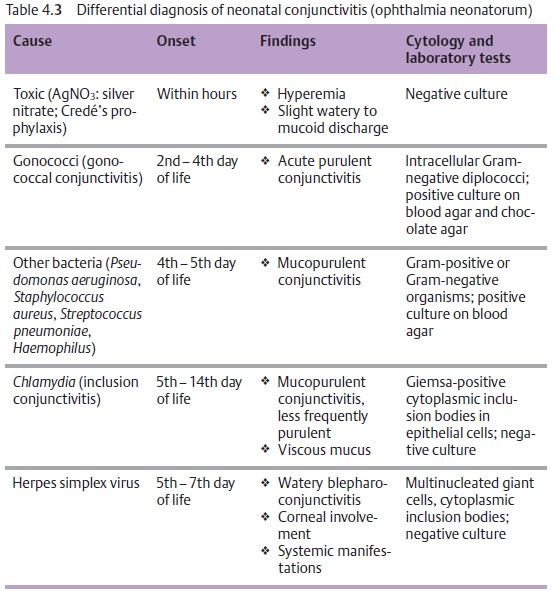
Symptoms: Depending on the pathogen, the inflammation will manifestitself
between the second and fourteenth day of life (Table 4.3). The spectrum ranges from mild conjunctival irritation to
life-threatening infection (especially with gonococcal infection).
Conjunctivitis as a result of Credé’s method of prophylaxis appears with hours
but only leads to mild conjunctival irritation.
Acute purulent conjunctivitis in the newborn (gonococcal conjunctivi-tis) is considered a medical emergency. The patient should be referred to an ophthalmologist for specific diagnosis.
Diagnostic considerations: The tentative clinical diagnosis is made on thebasis of the
onset of the disease (Table 4.3) and
the clinical syndrome. For example, gonococcal infections (gonococcal
conjunctivitis) are typified by particularly severe accumulations of pus (Figs.
4.16a and b). The newborn’s eyelid are tight and swollen because the pus
accumulates under them. When the baby’s eyes are opened, the pus can squirt out
under pressure and cause dangerous conjunctivitis in the examiner’s own eyes.
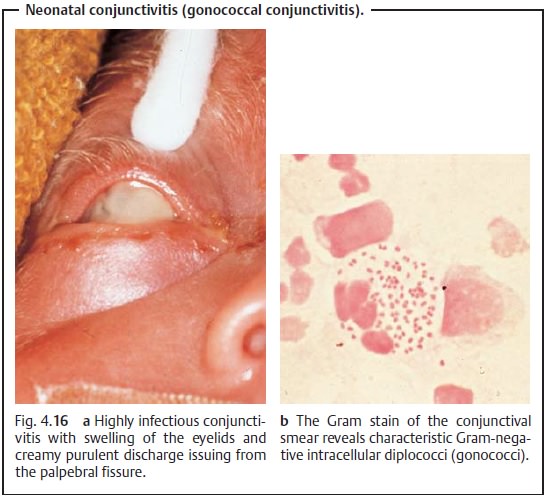
The examiner should always wear eye protection in the presence of sus-pected gonococcal conjunctivitis to guard against infection from pus issuing from the newborn’s eyes. Gonococci can penetrate the eye even in the absence of a corneal defect and lead to loss of the eye.
The diagnosis should be confirmed by cytologic
and microbiological studies. However, these studies often fail to yield
unequivocal results, so that treat-ment must proceed on the basis of clinical
findings.
Differential diagnosis: The onset of the disease is crucial to differential diag-nosis
(Table 4.3). Neonatal conjunctivitis
must be distinguished from neonatal dacryocystitis. This disorder differs from
the specific forms of con-junctivitis in it only becomes symptomatic two to
four weeks after birth, with reddening and swelling of the region of the
lacrimal sac and purulent dis-charge from the puncta. It can be readily
distinguished from neonatal con-junctivitis because of these symptoms.
Treatment: Toxic conjunctivitis(Credé’s method of prophylaxis): When theeye
is regularly flushed and the eyelids cleaned, symptoms will abate
spon-taneously within one or two days.
Gonococcal conjunctivitis: Topical administration of broad-spectrum anti-biotics
(gentamicin eyedrops every hour) and systemic penicillin (penicillin G IV 2
mill. IU daily) or cephalosporin in the presence of penicillinase-produc-ing
strains.
Chlamydial conjunctivitis: Systemic erythromycin and topical erythromy-cin eyedrops five
times daily. There is a risk of recurrence where the dosage or duration of
treatment is insufficient. It is essential to examine the parents and include
them in therapy.
Herpes simplex conjunctivitis: Therapy involves application of acyclovirointment to the
conjunctival sac and eyelids as herpes vesicles will usually be present there,
too. Systemic acyclovir therapy is only required in severe cases.
Prophylaxis: Credé’s method of prophylaxis(application of 1% silver nitratesolution)
prevents bacterial inflammation but not chlamydial or herpes infec-tion.
Prophylaxis of chlamydial infection consists of regular examination of the
woman during pregnancy and treatment in appropriate cases.
Parasitic and Mycotic Conjunctivitis
Parasitic and mycotic forms of conjunctivitis
(see Table 4.2) are less
important in temperate climates. They are either very rare or occur primarily as co-morbidities associated with a
primary corneal disorder, such as mycotic infections of corneal ulcers.
Related Topics