Chapter: Ophthalmology: Conjunctiva
Conjunctival Degeneration and Aging Changes
Conjunctival Degeneration and Aging Changes
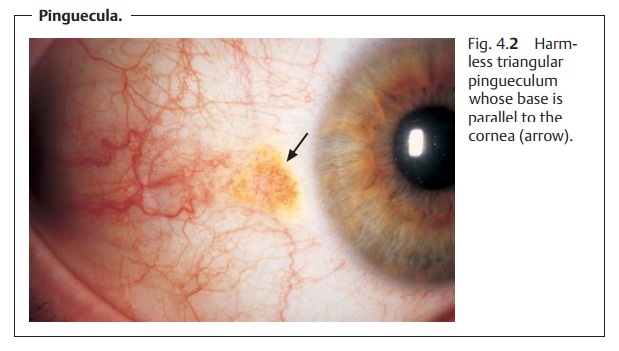
Pingueculum
Definition
Harmless grayish yellow thickening of the
conjunctival epithelium in the palpe-bral fissure.
Epidemiology: Pinguecula are the most frequently observed conjunctivalchanges.
Etiology: The harmless thickening of the conjunctiva is due tohyalinedegeneration of the subepithelial
collagen tissue. Advanced age and exposureto sun, wind, and dust foster the
occurrence of the disorder.
Symptoms: Pingueculum does not cause any symptoms.
Diagnostic considerations: Inspection will reveal grayish yellow thickeningat 3 o’clock and
9 o’clock on the limbus. The base of the triangular thickening (often located
medially) will be parallel to the limbus of the cornea; the tip will be
directed toward the angle of the eye (Fig. 4.2).
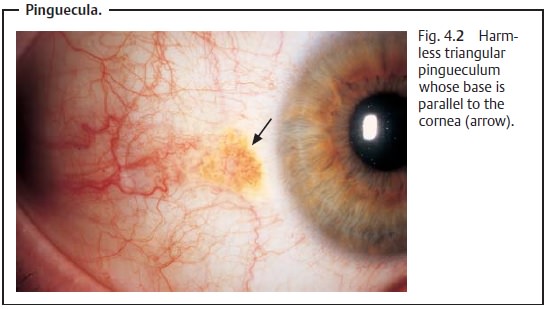
Differential diagnosis: A pingueculum is an unequivocal finding.
Treatment: No treatment is necessary.
Pterygium
Definition Triangular fold of conjunctiva that usually
grows from the medial portion of the palpebral fissure toward the cornea.
Epidemiology: Pterygium is especially prevalent in southern countries dueto increased exposure to intense sunlight.
Etiology: Histologically, a pterygium is identical to a pinguecula.
However, itdiffers in that it can grow on to the cornea; the gray head of the
pterygium will grow gradually toward the center of the cornea (Fig. 4.3a). This progression is presumably the
result of a disorder of Bowman’s layer of
the cornea, which pro-vides the necessary growth substrate for the
pterygium.
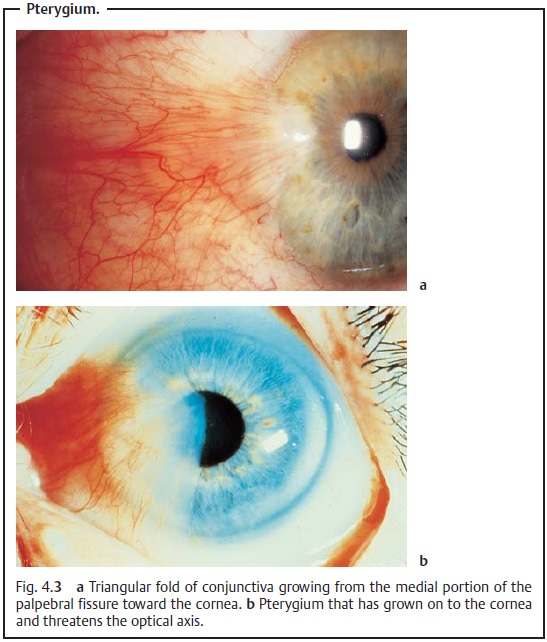
Symptoms and diagnostic considerations: A pterygium only producessymptoms when its
head threatens the center of the cornea and with it the visual axis (Fig. 4.3b). Tensile forces acting on the
cornea can cause severe corneal astigmatism. A steadily advancing pterygium that
includes scarred conjunctival tissue can also gradually impair ocular motility;
the patient will then experience double vision in abduction.
Differential diagnosis: A pterygium is an unequivocal finding.
Treatment: Treatment is only necessary when the pterygium produces
thesymptoms discussed above. Surgical removal is indicated in such cases. The
head and body of the pterygium are largely removed, and the sclera is left open
at the site. The cornea is then smoothed with a diamond reamer or an excimer laser
(a special laser that operates in the ultraviolet range at a wavelength of 193
nm).
Clinical course and prognosis: Pterygia tend to recur. Keratoplasty is indi-cated in such cases to replace the diseased Bowman’s layer with normal tissue. Otherwise the diseased Bowman’s layer will continue to provide a growth substrate for a recurrent pterygium.
Pseudopterygium
A pseudopterygium due to conjunctival scarring differs from a pterygium in that there are adhesions between the scarred conjunctiva and the cornea and sclera. Causes include corneal injuries and/or chemical injuries and burns. Pseudopterygia cause pain and double vision. Treatment consists of lysis of the adhesions, excision of the scarred conjunctival tissue, and coverage of the defect (this may be achieved with a free conjunctival graft harvested from the temporal aspect).
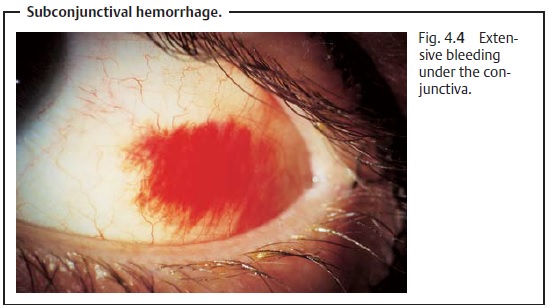
Subconjunctival Hemorrhage
Extensive bleeding under the conjunctiva (Fig.
4.4) frequently occurs
with conjunctival injuries (for obtaining a history in trauma cases, see
conjunctival laceration). Subconjunctival hemorrhaging will also often occur
spontaneously in elderly patients (as a result of compromised vascular
struc-tures in arteriosclerosis), or it may occur after coughing, sneezing,
pressing, bending over, or lifting heavy objects. Although these findings are
often very unsettling for the patient, they are usually harmless and resolve spon-taneously within two weeks. The patient’s
blood pressure and coagulation status need only be checked to exclude
hypertension or coagulation disorders when subconjunctival hemorrhaging occurs
repeatedly.
Calcareous Infiltration
A foreign-body sensation in the eye is often
caused by white punctate concre-ments on the palpebral conjunctiva. These
concrements are the calcified con-tents of
goblet cells, accessory conjunctival and lacrimal glands, or mei-bomian glands
where there is insufficient drainage of secretion. These cal-careous
infiltrates can be removed with a scalpel under topical anesthesia.
Conjunctival Xerosis
Definition
Desiccation of the conjunctiva due to a vitamin A deficiency.
Epidemiology: Due to the high general standard of nutrition, this disorder
isvery rare in the developed world. However, it is one of the most frequent
causes of blindness in developing countries.
Etiology: Vitamin A deficiency results in keratinization of the
superficialepithelial cells of the eye. Degeneration of the goblet cells causes
the surface of the conjunctiva to lose it luster (Fig. 4.5a). The keratinized epithelial cells die and are swept into the
palpebral fissure by blinking, where they accumu-late and create characteristic
white Bitot’s spots (Fig. 4.5b).
Xerosis bacteria frequently proliferate.
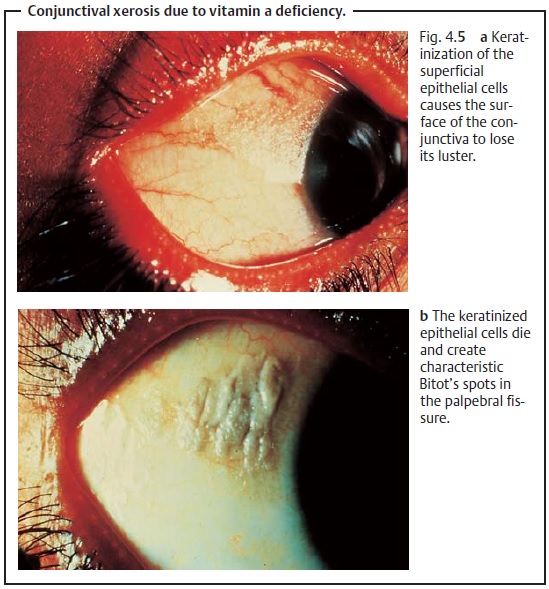
Treatment and prognosis: The changes disappear after local and systemicvitamin A substitution.
Without vitamin A substitution, the disorder will lead to blindness within a
few years.
Related Topics