Chapter: Clinical Anesthesiology: Clinical Pharmacology: Neuromuscular Blocking Agents
Nondepolarizing Muscle Relaxants: General Pharmacological Characteristics
General Pharmacological Characteristics
Some variables affect all
nondepolarizing muscle relaxants.
A. Temperature
Hypothermia prolongs blockade by
decreasing metabolism (eg, mivacurium, atracurium, and cisa-tracurium) and
delaying excretion (eg, pancuronium and vecuronium).
B. Acid–Base Balance
Respiratory acidosis potentiates the
blockade of most nondepolarizing relaxants and antagonizes its reversal. This
could prevent complete neuro-muscular recovery in a hypoventilating
postop-erative patient. Conflicting findings regarding the neuromuscular effects
of other acid–base changes may be due to coexisting alterations in
extracellu-lar pH, intracellular pH, electrolyte concentrations, or structural
differences between drugs (eg, mono-quaternary versus bisquaternary; steroidal
versus isoquinolinium).
C. Electrolyte Abnormalities
Hypokalemia and hypocalcemia augment a non-depolarizing block. The responses of patients with hypercalcemia are unpredictable. Hypermagnese-mia, as may be seen in preeclamptic patients being managed with magnesium sulfate (or after intra-venous magnesium administered in the operating room), potentiates a nondepolarizing blockade by competing with calcium at the motor end-plate.
D. Age
Neonates have an increased sensitivity
to nondepo-larizing relaxants because of their immature neu-romuscular
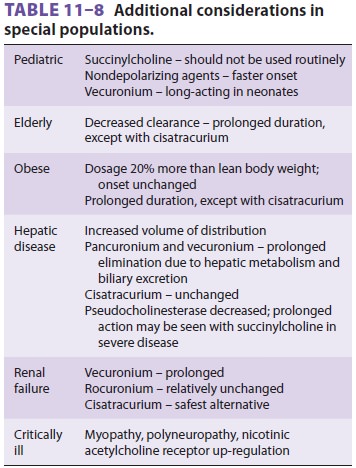
junctions ( Table
11-8). This sensitivity does not necessarily decrease dosage
requirements, as the neonate’s greater extracellular space provides a larger
volume of distribution.
E. Drug Interactions
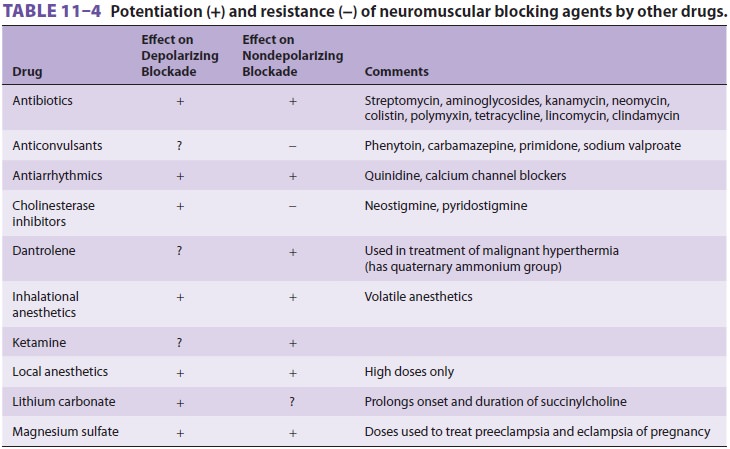
As noted earlier, many drugs augment
nondepo-larizing blockade (see Table 11–4). They have mul-tiple sites of
interaction: prejunctional structures, postjunctional cholinergic receptors,
and muscle membranes.
F. Concurrent Disease
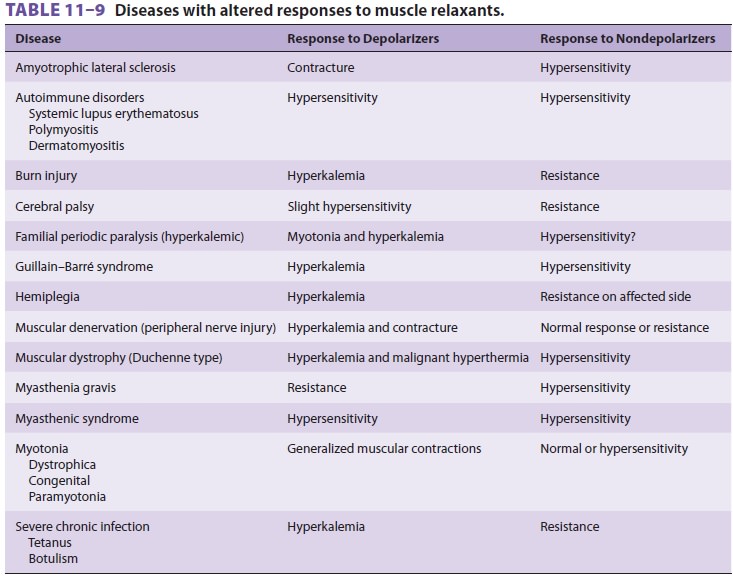
The presence of neurological or muscular disease can have
profound effects on an individual’s response to muscle relaxants ( Table 11–9). Cirrhotic liver
disease and chronic renal failure oftenresult in an increased volume of
distribution and a lower plasma concentration for a given dose of
water-soluble drugs, such as muscle
relaxants. On the other hand, drugs dependent on hepatic or renal excretion may
demonstrate prolonged clearance (Table 11-8). Thus, depending on the drug
chosen, a greater initial (loading) dose—but smaller mainte-nance doses—might
be required in these diseases.
G. Muscle Groups
The onset and intensity of blockade vary
among mus-cle groups. This may be due to differences in blood flow, distance
from the central circulation, or differ-ent fiber types. Furthermore, the
relative sensitivity of a muscle group may depend on the choice of mus-cle
relaxant. In general, the diaphragm, jaw, larynx, and facial muscles
(orbicularis oculi) respond to and recover from muscle relaxation sooner than
the thumb. Although they are a fortuitous safety feature, persistent
diaphragmatic contractions can be dis-concerting in the face of complete
adductor pollicis paralysis. Glottic musculature is also quite resistant to
blockade, as is often confirmed during laryngos-copy. The ED95 for laryngeal muscles is nearly two times that for
the adductor pollicis muscle. Good intubating conditions are usually associated
with visual loss of the orbicularis oculi twitch response.
Considering the multitude of factors
influenc-ing the duration and magnitude of muscle relax-ation, it becomes clear
that an individual’s response to neuromuscular blocking agents should be
moni-tored. Wide variability in sensitivity to nondepolarizing muscle relaxants
is often encountered in clinical practice.
Related Topics