Chapter: Ophthalmology: Eye Optics and Refractive Errors
Myopia (Shortsightedness)
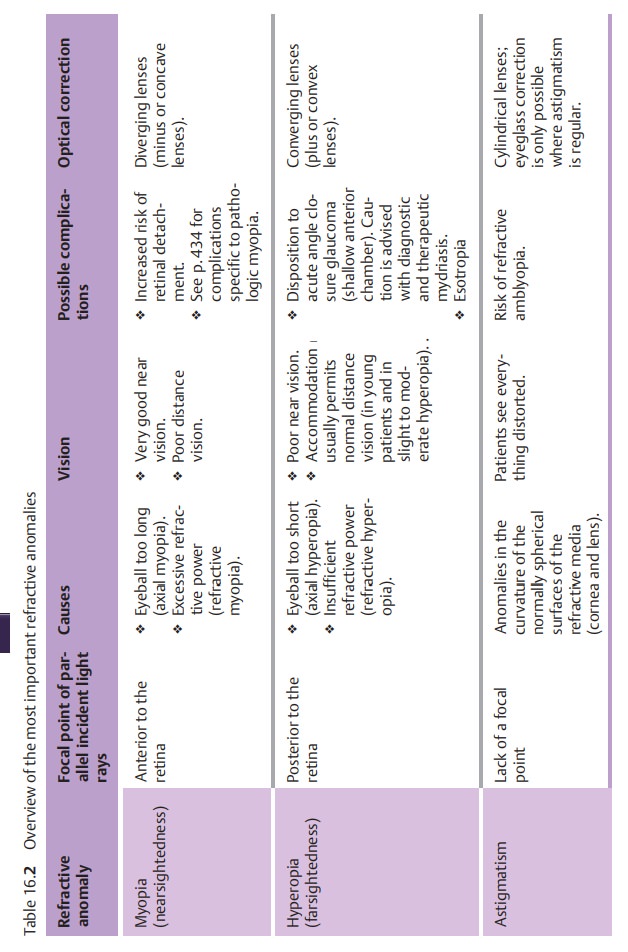
Refractive Anomalies (Table 16.2)
Myopia (Shortsightedness)
Definition
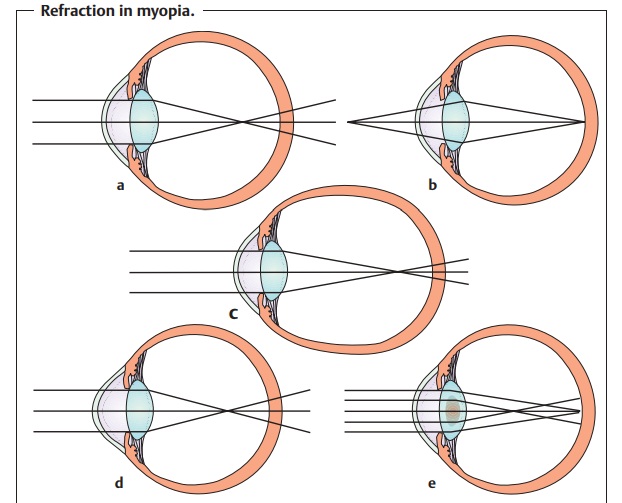
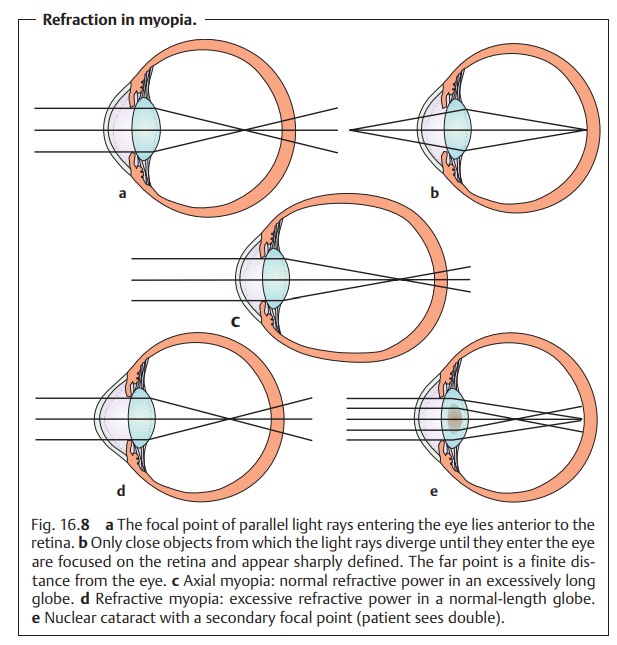
A discrepancy between the refractive power and
axial length of the eye such that parallel incident light rays converge at a focal point anterior to the retina (Fig.
16.8a).
Epidemiology:
Approximately 25% of persons between the ages of 20 and 30have refraction less than –1 diopters.
Etiology:
The etiology of myopia is not clear. Familial patterns of
increasedincidence suggest the influence of genetic factors.
Pathophysiology:
Whereas parallel incident light rays converge at a focalpoint on
the retina in emmetropic eyes, they converge at a focal point anteriorto the retina in myopic eyes
(Fig. 16.8a). This means that no sharply defined images appear on the
retina when the patient gazes into the
distance (Fig. 16.8a). The
myopic eye can only produce sharply
defined images of closeobjects from
which the light rays diverge until they enter the eye (Fig. 16.8b).The far point moves closer; in
myopia of –1 diopter it lies at a distance of 1 m.
In myopia, the far point (distance from the
eye = A) can be calculated using the formula: A (m) = 1/D, where D is myopia in
diopters.
Possible causes include an excessively long globe with normal
refractive power (axial myopia; Fig. 16.8c) and, less frequently, excessive
refractive power in a normal-length globe (refractive myopia; Fig. 16.8d).
A difference in globe length of 1 mm with
respect to a normal eye corre-sponds to a difference of about 3 diopters in
refractive power.
Special forms of refractive myopia:
❖ Myopic sclerosis of the nucleus of the lens (cataract) in advanced age. This causes a
secondary focal point to develop, which can lead to monocular diplopia (double
vision).
❖ Keratoconus (increase in the refractive power
of the cornea).
❖ Spherophakia (spherically shaped lens).
Forms:
These include:
❖ Simple myopia (school-age myopia): Onset is at the age of 10 – 12
years.Usually the myopia does not progress after the age of 20. Refraction
rarely exceeds 6 diopters. However, a benign
progressive myopia also exists, which stabilizes only after the age of 30.
❖ Pathologic myopia: This disorder is largely hereditary and progresses con-tinuously independently of external influences.
Symptoms and diagnostic considerations:
The diagnosis is made on thebasis of a typical
clinical picture and refraction testing. Myopic patients have very good near
vision. When gazing into the distance, they squint in an attempt to improve
their uncorrected visual acuity by further narrowing the optic aperture of the
pupil. The term “myopia” comes from this squinting; the Greek word “myein”
means to squint or close the eyes. Older
myopic patients can read without corrective lenses by holding the reading
material at about the distance of the far point.
The typical morphologic changes occurring in myopia are referred to as myopia syndrome. Progressive myopia in particular is characterized bythin-ning of the sclera. The elongation of the globe causes a shift in the axes of the eye.
This often simulates esotropia. The anterior chamber is deep. Atrophy of theciliary muscle is present
as it is hardly used. The volume of the vitreous body istoo small for the large
eye, and it may collapse prematurely. This results in vit-reous opacifications that the patient perceives as floaters.
Morphologic fundus changes in myopia, such as
maculopathy and Fuchs’ spot..
The risk of retinal
detachment is increased in
myopia. However, it does not increase
in proportion to the severity of the myopia.
Because of the increased risk of retinal
detachment, patients with myopia should be examined particularly thoroughly for
prodromal signs of retinal detachment, such as equatorial degeneration or
retinal tears. Therefore, examination of the fundus with the pupil dilated is
indicated both when the first pair of eyeglasses is prescribed and at reg-ular
intervals thereafter.
Glaucoma is more difficult to diagnose in patients with myopia.
Measure-ments of intraocular pressure obtained with a Schiøtz tonometer will be
lower than normal due to the decreased rigidity of the sclera.
Applanation tonometry yields the most accurate
values in patients with myopia because the rigidity of the sclera only slightly
influences results.
The optic cup is also difficult to evaluate in patients
with myopia because the optic nerve enters the eye obliquely. This also makes
glaucoma more difficult to diagnose.
Treatment:
The excessive refractive power of the refractive media must bereduced. This is achieved through the use of diverging lenses (minus or con-cave lenses; Fig. 16.9a). These lenses cause parallel incident light rays to diverge behind the lens. The divergent rays converge at a virtual focal point in front of the lens. The refractive power (D) is negative (hence the term “minus lens”) and is equal to 1/f, where f is the focal length in meters.
Previously, biconcave
or planoconcave lens blanks were
used in the manufacture of cor-rective lenses. However, these entailed a number
of optical disadvantages. Today lenses are manufactured in a positive meniscus shape to reduce lens
aberrations.
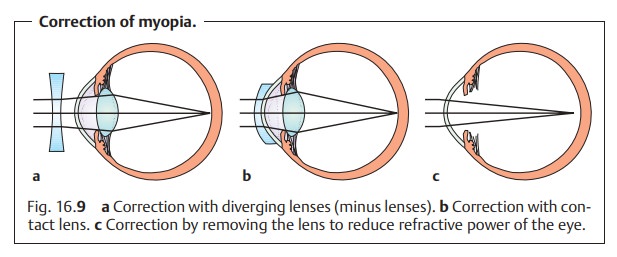
Correction with contact lenses (Fig. 16.9b) offers optical advantages. Thereduction in the size of the
image is less than with eyeglass correction. Aber-rations are also reduced.
These advantages are clinically relevant with myopia exceeding 3 diopters.
The closer the “minus” lens is to the eye, the
weaker its refractive power must be to achieve the desired optic effect.
Minus lenses to be used to correct myopia
should be no stronger than abso-lutely necessary. Although accommodation could
compensate for an overcor-rection, patients usually do not tolerate this well.
Accommodative asthenopia (rapid ocular fatigue) results from the excessive stress
caused by chronic con-traction of the atrophic ciliary muscle.
Myopic patients have “lazy” accommodation due
to atrophy of the cili-ary muscle. A very slight undercorrection is often
better tolerated than a perfectly sharp image with minimal overcorrection.
In certain special cases, removal of the crystalline lens (Fig. 16.9c) may be performed to reduce the refractive power of the myopic
eye. However, this operation is associated with a high risk of retinal
detachment and is rarely performed. There is also the possibility of implanting
an anterior chamberintraocular lens (diverging lens) anterior to the natural lens to reduce
refrac-tive power.
Popular health books describe exercises that
can allegedly treat refractive errors such as nearsightedness without
eyeglasses or contact lenses. Such exercises cannot influence the sharpness of
the retinal image; they can only seemingly improve uncorrected visual acuity by
training the patient to make better use of additional visual information.
However, after puberty no late sequelae of chronically uncorrected vision are
to be expected.
Related Topics