Chapter: 11th Zoology : Chapter 8 : Excretion
Mechanism of urine formation in human
Mechanism of urine formation in human
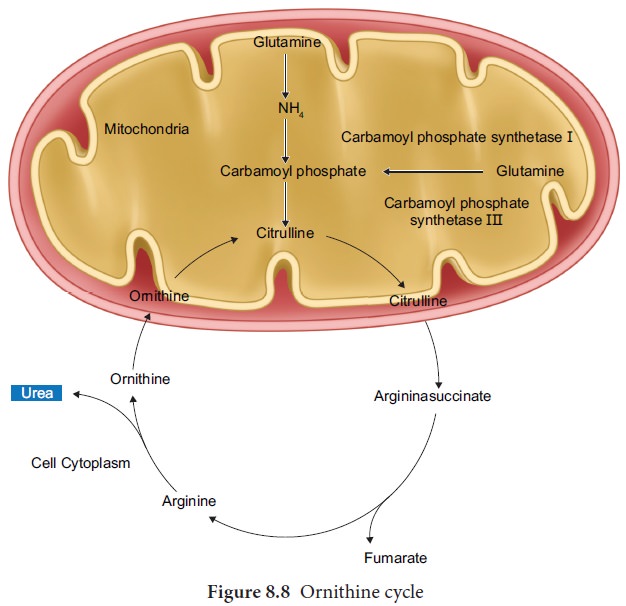
The nitrogenous waste formed as a result of
breakdown of amino acids is converted to urea in the liver by the Ornithine
cycle or urea cycle (Figure 8.8).
Urine formation involves three main processes
namely, glomerular filtration, tubular reabsorption and tubular secretion.
i) Glomerular Filtration:
Blood enters the kidney from the renal artery, into the glomerulus. Blood is composed of large quantities of water, colloidal proteins, sugars, salts and nitrogenous end product. The first step in urine formation is the filtration of blood that takes place in the glomerulus. This is called glomerular filtration which is a passive process. The fluid that leaves the glomerular capillaries and enters the Bowman’s capsule is called the glomerular filtrate. The glomerular membrane has a large surface area and is more permeable to water and small molecules present in the blood plasma. Blood enters the glomerulus faster with greater force through the afferent arteriole and leaves the glomerulus through the efferent arterioles, much slower.
This force is because of the difference in sizes between the afferent
and efferent arteriole (afferent arteriole is wider than efferent arteriole)
and glomerular hydrostatic pressure which is around 55mm Hg.
Kidneys produce about 180L of glomerular filtrate
in 24 hours. The molecules such as water, glucose, amino acids and nitrogenous
substances pass freely from the blood into the glomerulus. Molecules larger
than 5nm are barred from entering the tubule. Glomerular pressure is the chief
force that pushes water and solutes out of the blood and across the filtration
membrane. The glomerular blood pressure (approximately 55
mmHg) is much higher than in other capillary beds.
The two opposing forces are contributed by the plasma proteins in the
capillaries. These includes, colloidal osmotic pressure (30 mmHg) and the capsular
hydrostatic pressure (15 mmHg) due to the fluids in the glomerular capsule. The
net filtration pressure of 10 mmHg is responsible for the renal filtration.
Net filtration Pressure = Glomerular
hydrostatic pressure = (Colloidal osmotic pressure +
Capsular hydrostatic pressure).
Net filtration pressure = 55 mmHg - (30 mmHg + 15
mmHg) = 10mmHg
The effective glomerular pressure of 10 mmHg
results in ultrafiltration.
Glomerular
filtration rate (GFR) is the volume of filtrate
formed min-1 in all nephrons (glomerulus) of both the kidneys. In adults the
GFR is approximately 120-
125mL/min. Blood from the glomerulus is passed out
through the efferent arteriole.
The smooth muscle of the efferent arteriole
contract resulting in vasoconstriction.
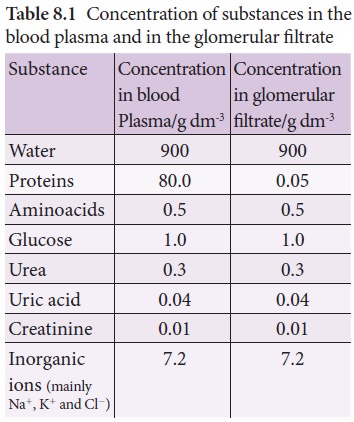
Table 8.1 shows the relative concentrations of substances in the blood plasma and the glomerular filtrate. The glomerular filtrate is similar to blood plasma except that there are no plasma proteins.
In cortical nephrons, blood from efferent arteriole
flows into peritubular capillary beds and enters the venous system carrying
with it recovered solutes and water from the interstitial fluid that surrounds
the tubule.
ii) Tubular Reabsorption
This involves movement of the filtrate back into the
circulation. The volume of filtrate formed per day is around 170-180 L and the
urine released is around 1.5 L per day, i.e., nearly 99% of the glomerular
filtrate that has to be reabsorbed by the renal tubules as it contains certain
substances needed by the body. This process is called selective reabsorption.
Reabsorption takes place by the tubular epithelial cells in different segments
of the nephron either by active transport or passive transport, diffusion and
osmosis.
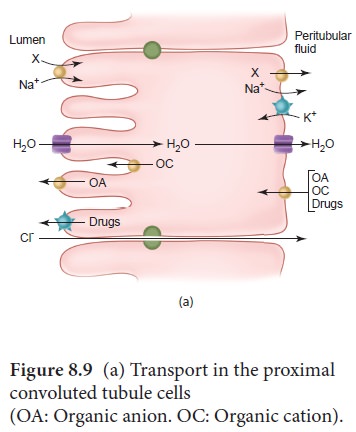
Proximal convoluted Tubule (PCT)-Glucose, lactate, amino acids, Na+ and water in the filtrate is reabsorbed in the PCT. Sodium is reabsorbed by active transport through sodium- potassium (Na+ K+) pump in the PCT. Small amounts of urea and uric acid are also reabsorbed.
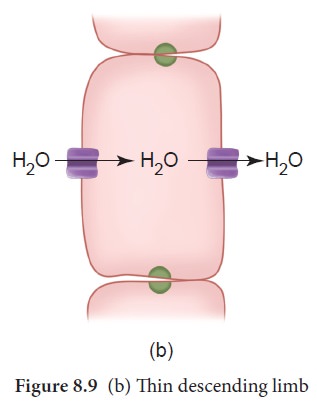
Descending
limb of Henle’s loop is permeable
to water due the presence of aquaporins,
but not permeable to salts. Water is lost in the descending limb, hence Na+
and Cl- gets concentrated in the filtrate (Figure 8.9(b)).
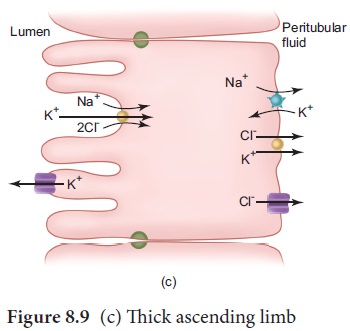
Ascending
limb of Henle’s loop is impermeable to water but permeable to solutes such as Na+, Cl-
and K+ (Figure 8.9(c)).
The distal
convoluted tubule recovers water and secretes potassium into the tubule.
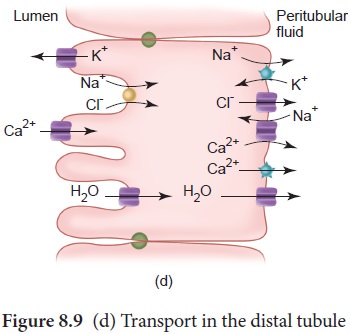
Na+, Cl- and water remains in the filtrate of the DCT (Figure 8.9(d)). Most of
the reabsorption from this point is dependent on the body’s need and is
regulated by hormones. Reabsorption of bicarbonate (HCO 3-)
takes place to regulate the blood pH. Homeostasis of K+ and Na+
in the blood is also regulated in this region.
Collecting duct is permeable to water, secretes K+ (potassium ions are actively transported into the tubule) and reabsorbs Na+ to produce concentrated urine. The change in permeability to water is due to the presence of number of water-permeable channels called aquaporins.
Tubular secretion- Substances such as H+,
K+, NH4+, creatinine and organic acids move
into the filtrate from the peritubular capillaries into the tubular fluid. Most
of the water is absorbed in the proximal convoluted tubule and Na+
is exchanged for water in the loop of Henle. Hypotonic fluid enters the distal
convoluted tubule and substances such as urea and salts pass from peritubular
blood into the cells of DCT. The urine excreted contains both filtered and
secreted substances. Once it enters the collecting duct, water is absorbed and
concentrated hypertonic urine is formed. For every H+ secreted into the tubular filtrate, a Na+ is
absorbed by the tubular cell. The H1 secreted combines with HCO3-,
HPO3- and NH3- and gets fixed as H2CO4-,
H2PO4+ and NH4-
respectively. Since H+ gets fixed in the fluid, reabsorption of H+
is prevented.
Osmolarity - The solute concentration
of a solution of water is known as the solutions osmolarity, expressed as
milliosmoles /liter (mOsm/L)
Formation of concentrated urine
Formation of concentrated urine is accomplished by kidneys using counter current mechanisms. The major function of Henle’s
loop is to concentrate Na+ and Cl-. There is low
osmolarity near the cortex and high osmolarity towards the medulla. This
osmolarity in the medulla is due to the presence of the solute transporters and
is maintained by the arrangement of the loop of Henle, collecting duct and vasa
recta. This arrangement allows movement of solutes from the filtrate to the
interstitial fluid. At the transition between the proximal convoluted tubule
and the descending loop of Henle the osmolarity of the interstitial fluid is
similar to that ofthe blood – about 300mOsm. Ascending and descending limbs of
Henle, create a counter current multiplier (interaction between flow of filtrate through the
limbs of Henle’s and JMN) by active transport. Figure 8.10
(a) shows the counter current multiplier created by the long loops of Henle of
the JM nephrons which creates medullary osmotic gradient. As the fluid enters
the descending limb, water moves from the lumen into the interstitial fluid and
the osmolarity decreases. To counteract this dilution the region of the
ascending limb actively pumps solutes from the lumen into the interstitial
fluid and the osmolarity increases to about 1200mOsm in medulla. This mismatch
between water and salts creates osmotic gradient in the medulla. The osmotic
gradient is also due to the permeability of the collecting duct to urea.
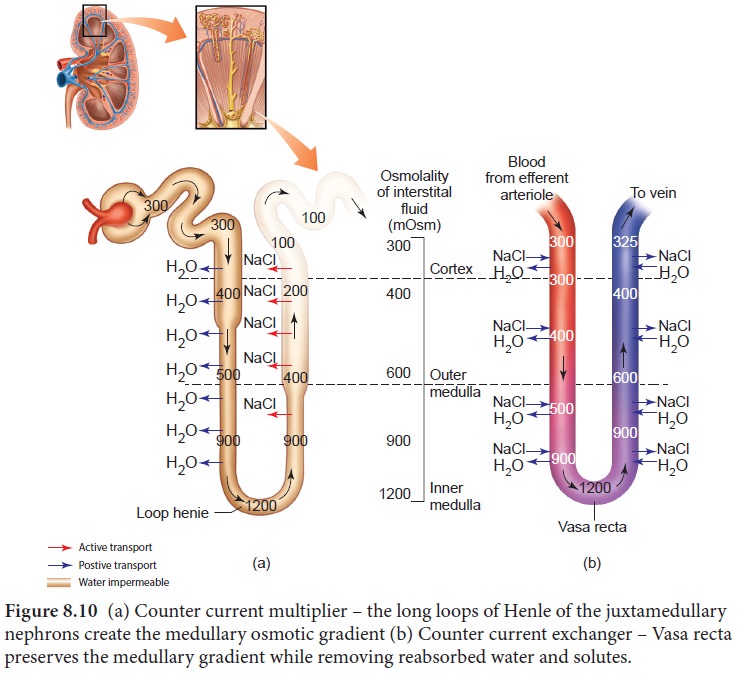
The vasa recta, maintains the medullary osmotic
gradient via counter current exchanger (the flow of blood through
the ascending and descending vasa recta blood vessels) by passive transport. Figure 8.10 shows counter current
exchanger where the vasa recta preserves the medullary gradient while removing
reabsorbed water and solutes. This system does not produce an osmotic gradient,
but protects the medulla by removal of excess salts from the interstitial fluid
and removing reabsorbed water. The vasa recta leave the kidney at the junction
between the cortex and medulla. The interstitial fluid at this point is
iso-osmotic to the blood. When the blood leaves the efferent arteriole and
enters vasa recta the osmolarity in the medulla increases (1200mOsm)
and results in passive uptake of solutes and loss of water. As the blood enters
the cortex, the osmolarity in the blood decreases (300mOsm) and the blood loses
solutes and gains water to form concentrated urine (hypertonic). Human kidneys
can produce urine nearly four times concentrated than the initial filtrate
formed.
Related Topics