Excretion | Zoology - Answer the following questions | 11th Zoology : Chapter 8 : Excretion
Chapter: 11th Zoology : Chapter 8 : Excretion
Answer the following questions
Zoology
Excretion
Evaluation
Answer the following questions
1. Arrange the following structures in the order that a drop of water entering the nephron would encounter them.
a. Afferent arteriole
b. Bowman’s capsule
c. Collecting duct
d. Distal tubule
e. Glomerulus
f. Loop of Henle
g. Proximal tubule
h. Renal pelvis
Answer:
a. Afferent arteriole
e. Glomerulus
b. Bowman’s capsule
g. Proximal tubule
f. Loop of Henle
d. Distal tubule
c. Collecting duct
h. Renal pelvis
2. Name the three filtration barriers that solutes must come across as they move from plasma to the lumen of Bowman’s capsule. What components of the blood are usually excluded by these layers?
1.
Glomerulus net filtration pressure - 55 mm Hg
2.
Colloidal osmotic pressure - 30 mm Hg
3.
Capsular Hydrostatic pressure -15 mm Hg
Protein
aminoacid glucose urea, uricacid creatiinine etc are excluded by these layers.
3. What forces promote glomerular filtration? What forces opposes them? What is meant by net filtration pressure?
• Glomerulus hydrostatic pressure
• Glomerulus pressure
• Opposing pressure : Colloidal osmotic
pressure, Capsular hydrostatic pressure
• Net filtration pressure = Glomerular
hydrostatic pressure - (Colloidal osmotic pressure + capsular hydrostatic pressure.
4. Identify the following structures and explain their significance in renal physiology?
a. Juxtaglomerular apparatus
b. Podocytes
c. Sphincters in the bladder
d. Renal cortex
a) Juxta glomerular apparatus : It is a specialized
tissue in the afferent arteriole of the nephron that consists of macula densa and
granular cells.
• Action : The macula densa cells sense distal tubular flow
and assect afferent arterisle diameter.
• Actions of Glanular cells : When there is a fall in glomerular
blood flow it can activate Juxta glomerulus cells to release renin fromliver which
converts a angiotensinogen to angiotensin I.
• Angiotensin
converting enzyme converts angiotensin I to angiotensin II.
• It stimulates
Na+ reabsorption in the proximal convoluted tubule by vaso constriction
of the blood vessel and increases the glomerulae blood pressure.
b) Podocytes:
• The visceral
layer of Bowman's capsule is made of epithelial cells called podocytes.
• The podocytes
and the foot processes and the basement membrane of glomerulus acts as a filtering
membrane.
• Podocytes
acts in glomerulus filteration.
c) Sphincters in the bladder :
• The sphincters
of the bladder regulates the urination.
• When the bladder
is full the stretching of the urinary bladder stimulates the CNS through the sensory
neurons of the para sympathetic nervous system and brings about contraction of the
bladder.
• Somatic motor
neurons induces the sphincters to close.
• Smooth muscles
contract results in the opeining of the internal sphincters and relaxing the external
sphincter.
• The sphincter
opens and the urine is expelledout.
5. In which segment of the nephron most of the re-absorption of substances takes place?
• In the proximal convoluted tubule.
6. When a molecule or ion is reabsorbed from the lumen of the nephron, where does it go? If a solute is filtered and not reabsorbed from the tubule, where does it go?
If
a solute is filtered and not reabsorbed from the tubule, where does it go?
• The reabsorbed molecule of the lumen
of the nephron goes to interstial fluid and then goes to blood.
• The filtered molecule when it is not reabsorbed by the tubules it will be excreted out through urine.
7. Which segment is the site of secretion and regulated reabsorption of ions and pH homeostasis?
• 1. Distal tubule; 2. Collecting duct
• In the renal tubules H+
and NH4 are secreted and liberated into the tubules and excreted through
urine thus maintaining acid base balance.
• For each H+ ions from the
liberated filtrate one Na+ is reabsorbed in the tubules.
• The secreted HCO3, PO3
and NH3 combines to form carbonic acid and phosphoric acids.
• Thus the H+ are maintained
and their reabsorption is prevented.
8. What solute is normally present in the body to estimate GFR in humans?
• The glomerulus filtrate consists of
water glucose amino acids creatinine protein salts and urea.
• This solutes decides the glomerular
filtration rate.
9. Which part of the autonomic nervous system is involved in micturation process?
• Para sympathetic nervous system.
10. If the afferent arteriole of the nephron constricts, what happens to the GFR in that nephron? If the efferent arteriole constricts what happens to the GFR in that nephron? Assume that no auto regulation takes place.
• Blood enters the glomerulus faster
with greater force through the afferent arteriole and leaves the glomerulus through
the efferent arterioles much slower.
• Because afferent arteriole is wider
than efferent arteriole.
• The constriction of this does not
affect the rate of filtration.
23. Indentfiy the biological term Homeostasis, excretion, glomerulus,urea, glomerular filtration, ureters, urine, Bowman’s capsule, urinary system, reabsorption, micturition, osmosis, glomerular capillaries via efferent arteriole, proteins.
a) A liquid which gathers in the bladder - Urine
b) Produced when blood is filtered in a Bowman's capsule - Glomerular filtrate
c) Temporary storage of urine - Urinary bladder
d) A ball of inter twined capillaries - Glomerulus
e) Removal of unwanted subtances from the body - Excretion
f) Each contains a glomerulus - Bowman's Capsule
g) Carry urine from the kidneys to the bladder - Ureter
h) Scientific term for urination - Micturition
i) Regulation of water and dissolved substances in blood and tissue fluid
-
Osmo regulation
j) Consists of the kidneys ureters and bladder - Excretory system
k) Removal of useful substances from glomerular filtrate - reabsorption
l) What solute the blood contains that are not present in the glomerular filtrate? - Plasma Protein
24. With regards to toxicity and the need for dilution in water, how different are ureotelic and uricotelic excretions? Give examples of animals that use these types of excretion?
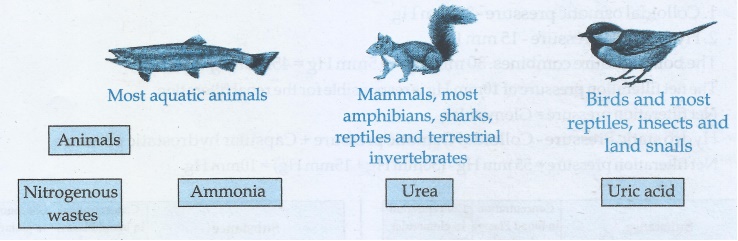
• The type of nitrogenous
end product (Urea or Uric acid or ammonia) of an animal excretion depends upon the
habitat of the animal.
• For Excretion of
Ammonia more water is needed.
• Animals that excrete
most of its nitrogen in the form of ammonia are called ammonoteles.
• Fishes Amphibians.
Uric acid can be eliminated with a minimum loss of water and are called Uricoteles.
• Reptiles, birds
insects, landnails, Mammals and terestrial amphibians excrete urea and are called
ureoteles.
25. Differentiate protonephridia from metanephridia
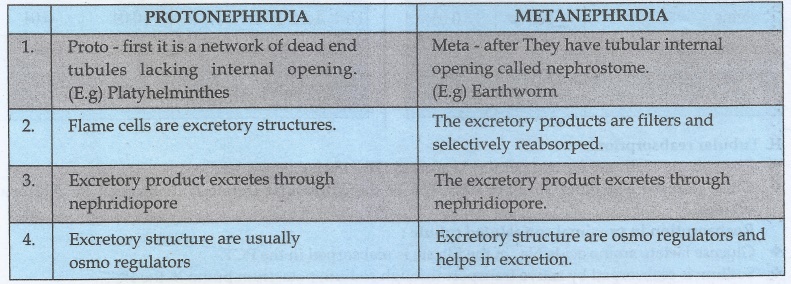
PROTONEPHRIDIA
i.
Proto - first it is a network of dead end tubules lacking internal opening.
(E.g)
Platyhelminthes
ii.
Flame cells are excretory structures.
iii.
Excretory product excretes through nephridiopore
iv.
Excretory structure are usually osmo regulators
METANEPHRIDIA
i.
Meta - after They have tubular internal opening called nephrostome.
(E.g)
Earthworm
ii.
The excretory products are filters and selectively reabsorped.
iii.
The excretory product excretes through nephridiopore.
iv.
Excretory structure are osmo regulators and helps in excretion.
26. What is the nitrogenous waste produced by amphibian larvae and by the adult animal?
• The adult amphibian's excretory product
is urea. The larval form of amphibian's excretory product is ammonia.
27. How is urea formed in the human body?
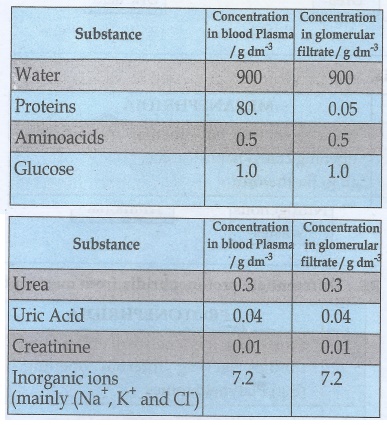
• Urine formation involves in three
main processes namely Glomerular filteration, tubular reabsorption and tubular recretion.
I. Glomerular filteration:
• Blood enters the kidney from the renal
artery into the glomerulus.
• Blood is composed of water colloidal
proteins, sugars and nitrogenous end product.
• The filteration is started in glomerulus.
The fluid that leaves the glomerular capillaries and enters the Bowman's capsule
is called the glomerular filtrate. It formed 170-180 litre within 24 hours.
• Glomerular membrane has large surface
area. Blood enters the glomerulus faster with greater force through the afferent
arteriole and leaves the glomerulus through the efferent arterioles much slower.
• This is because afferent arteriole
is wider than efferent arteriole and the glomerular hydrostatic pressure is around
55 mm Hg.
• Molecules larger than 5mm are barred
from entering the tubule.
• The two opposing forces are contributed
by the plasma proteins in the capillaries.
1.
Colloidal osmotic pressure - 30 mm Hg
2.
Hydrostatic pressure -15 mm Hg
The
both pressure combines. 30 mm Hg + 15mm Hg = 45mm Hg
• The net filteration pressure of 10mm
Hg is responsible for the renal filteration.
• Net filteration pressure = Glomerular
Hydro
static Pressure - Colloidal Osmotic pressure + Capsular hydrostatic pressure.
• Net filteration pressure = 55 mm Hg
- (30mm Hg + 15mm Hg) = 10mm Hg
II. Tubular reabsorption:
• The volume of filtrate formed per
day is around 170 - 180 l.
• Urine released is around 1.5 l per day. 99% of the glomerular filtrate
is reabsorped by the renal tubules.
Reabsorption in proximal convoluted tubule :
• Glucose lactate amino acids Na+
in the filtrate is reabsorped in the PCT.
• Sodium is reabsorped by active transport
through sodium potassium pump in the PCT.
• Small amounts of urea and uric acid
are reabsorped.
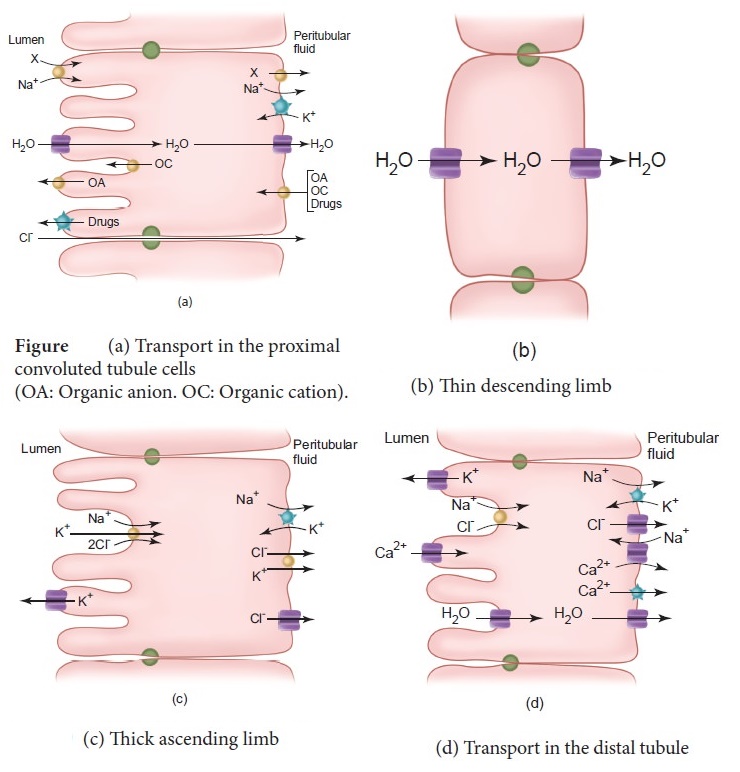
Reabsorption in Henle Loop:
• Descending limb of Henle's loop is
permeable to water due to the presence of aqua porins but not permeable to salts.
• Water is lost in the descending limb.
Hence Na+ and Cl− gets concentrated in the filtrate.
• Ascending limb of Henle's loop is
impermeable to water but permeable to Na+,Cl− and K+.
Distal Convoluted Tubule:
• It recovers water and secretes potassium
into tubule.
• Na+ Cl− and
water remains in the DCT.
• Reabsorption of HCO3 takes
place to regulate the blood pH.
• Collecting tubule is permeable to
water potassium ions are actively transported into the tubule and Na+
to produce concentrated urine.
Tubular Secretion:
• Once it enters the collecting duct
water is absorped and concentrated hypertonic urine is formed.
• For every H+ secreted into
the tubular filtrate a Na+ is absorbed by the tubular cell.
• The H+ secreted combines
with HCO3−, HPO3− and NH−
and gets fixed as H2CO3+, H2PO4+
and NH4+.
• Since H+ gets fixed in
the fluid reabsorption of H+ is prevented.
28. Differentiate cortical from medullary nephrons
• In the renal tubules proximal convoluted
tubule and distal convoluted tubule are situated in the cortical region of the kidney
and the loop of Henle is in the medullary region.
Cortical Nephron
1.
The loop of Henle is too short and extends only very little into the medulla.
2.
There is no vasarecta.
Medullary
Nephron
1.
Nephrons have long loop of Henle that run deep in to the medulla.
2.
Vasa recta is present.
29. What vessels carry blood to the kidneys? Is this blood arterial or venous?
• Renal artery right and left artery.
The blood is arterial.
30. Which vessels drain filtered blood from the kidneys?
• Renal vein. The filtered blood is
taken from the kidney to inferior vena cava through renal vein.
31. What is tubular secretion? Name the substances secreted through the renal tubules
• In the distal convoluted tubule the
urine becomes hypotonic.
• It contains urea and salts pass from
peri tubular blood in to the cells of DCT.
• For every H+ secreted a
Na+ is absorbed by the tubular cell.
• The H+ secreted combines
HCO3−, HPO3− and NH3−
and becomes carbonic acid phosphoric acid and ammonium.
• Since H+ gets fixed in
the fluid reabsorption of H+ is prevented.
32. How are the kidneys involved in controlling blood volume? How is the volume of blood in the body related to arterial pressure?
• When the volume of blood decreases
the flow pressure, decreases.
• This can be sensed by hypothalamus
and osmo receptors are stimulated and anti diuretic hormone is secreted from the
neuro hypophysis.
• The aquaporins in the proximal convoluted
tubules and collecting tubule reabsorb water. Hence the blood volume increases and
the blood pressure increases.
33. Name the three main hormones are involved in the regulation of the renal function?
• Renin
• AngioTensin I
• AngioTensin II
34. What is the function of antidiuretic hormone? Where is it produced and what stimuli increases or decreases its secretion?
• ADH which is also called as vasopressin
or Anti diuretic hormone is secreted from neuro hypophysis.
• Fluid loss or if blood pressure increases
the osmoreceptors of hypothalamus is stimulated and hence neuro hypophysis is stimulated
and secretes ADH.
• When the fluid level and pressure
is maintained due to the negative feed back mechanism ADH secretion stops.
35. What is the effect of aldosterone on kidneys and where is it produced?
• Due to the stimulation of Angiotensin
II the adrenal cortex secretes aldosterone. That causes reabsorption of Na+,
K+ excretion and absorption of water from distal convoluted tubule and
collecting tubule.
• This mechanism is known as Renin -
Angio tensin Aldosterone system.
36. Explain the heart's role in secreting a hormone that regulates renal function? What hormone is this?
• Excessive stretch of cardiac atrial
cells cause an increase in blood flow to the atria of the heart and release Atrial
Natriuretic Peptide or factor (ANF) travels to the kidney where H increases Na+
excretion and increases the blood flow to the glomerulus,
• Acting on the afferent glomerular
arterioles as a vasodilator or an efferent arterioles as a vasoconstrictor.
• The first identical natri uretic hormone
is atrial natriuretic horome of heart.
Related Topics