Chapter: Ophthalmology: Ocular Trauma
Mechanical Injuries
Mechanical Injuries
Eyelid Injury
Etiology:
Eyelid injuries can occur in practically every
facial injury. The fol-lowing types warrant special mention:
âť– Eyelid lacerations with involvement of the
eyelid margin.
âť– Avulsions of the eyelid in the medial canthus
with avulsion of the lacrimal canaliculus.
Clinical picture:
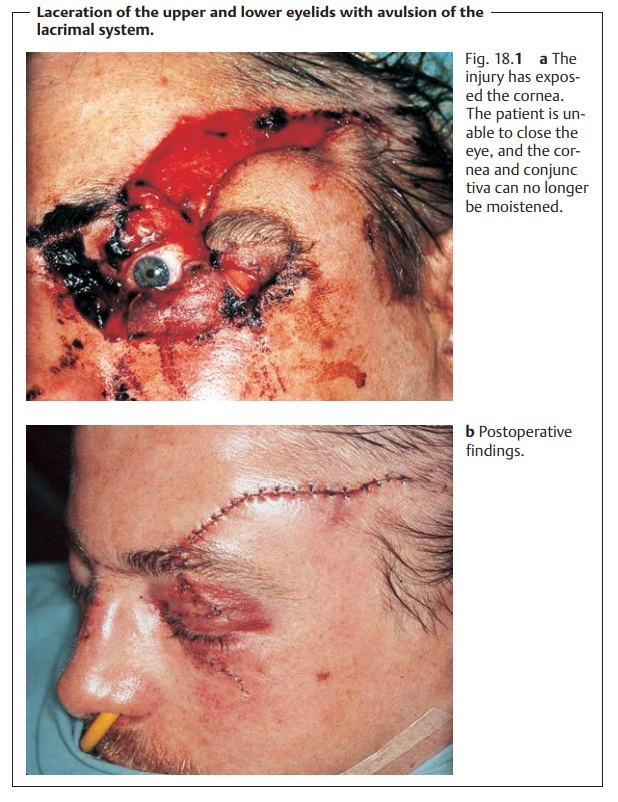
The highly vascularized and loosely textured
tissue of theeyelids causes them to bleed profusely when injured. Hematoma and
swell-ing will be severe (Fig. 18.1).
Abrasions usually involve only the
superficial lay-ers of the skin, whereas punctures,
cuts, and all eyelid avulsions due to blunttrauma (such as a fist) frequently involve all
layers. Bite wounds (such as dogbites) are often accompanied by injuries to the
lacrimal system.
Treatment:
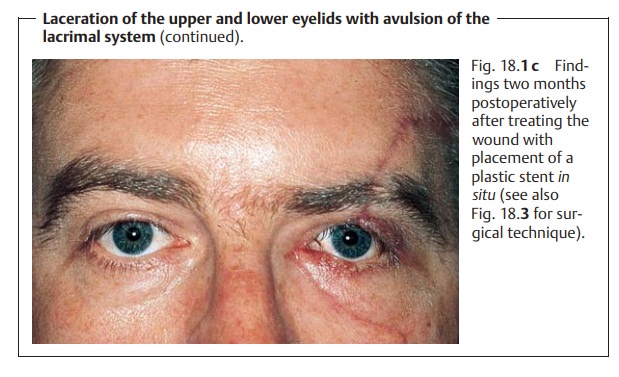
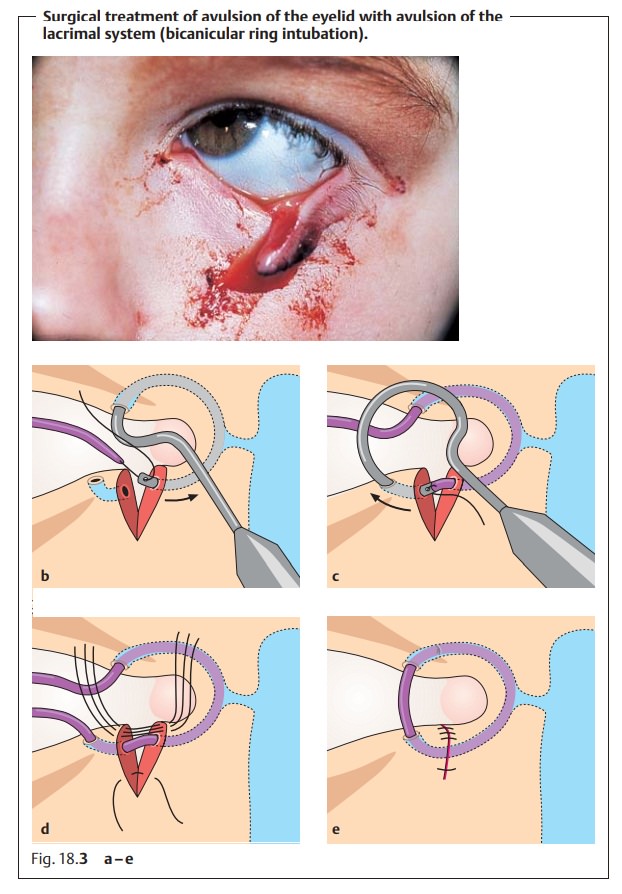
Surgical repair of eyelid injuries, especially
lacerations withinvolvement of the eyelid margin, should be performed with
care. The wound should be closed in layers and the edges properly approximated
to ensure a smooth margin without tension to avoid later complications, such as
cicatri-cial ectropion (Fig. 18.2).
Injuries to the Lacrimal System
Etiology:
Lacerations and tears in the medial canthus
(such as dog bites orglass splinters) can divide the lacrimal duct. Obliteration of the punctum and lacrimal
canaliculus is usually the result of a burn or chemical injury. Injuryto
the lacrimal sac or lacrimal gland usually occurs in conjunction
with severe craniofacial trauma (such as a kick from a horse or a traffic
accident). Dacryocystitis is a common sequela, which often can only be treated
by surgery (dacryocystorhinostomy).
Clinical picture:
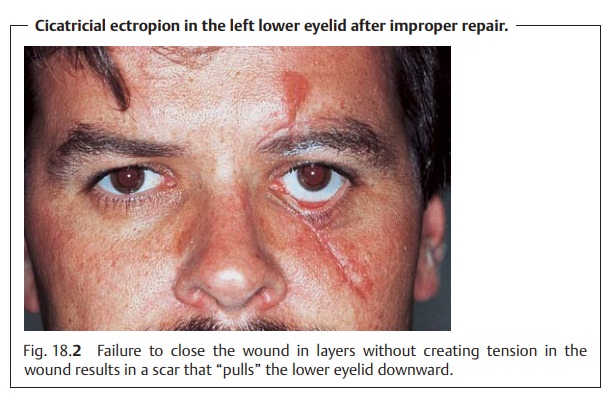
See Fig. 18.3 for avulsion of the lower lacrimal system (avulsions in the medial
canthus).
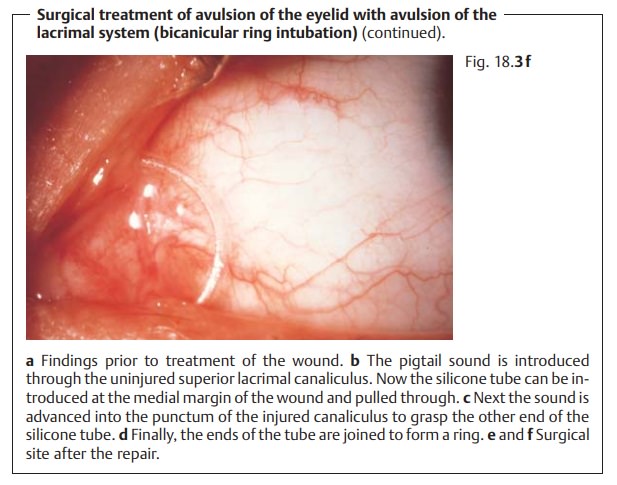
Treatment:
Lacrimal system injuries are repaired under an
operating micro-scope. A ring-shaped silicone stent is advanced into the
canaliculus using a special sound (Figs. 18.3b – f). The silicone stent remains in situ for three to four months and is then removed.
Surgical repair of eyelid and lacrimal system
injuries must be performed by an ophthalmologist.
Conjunctival Laceration
Epidemiology:
Due to its exposed position, thinness, and
mobility, the con-junctiva is susceptible to lacerations, which are usually
associated with sub-conjunctival hemorrhage.
Etiology:
Conjunctival lacerations most commonly occur
as a result of pene-trating wounds (such as from bending over a spiked-leaf
palm tree or from a branch that snaps back on to the eye).
Symptoms and diagnostic considerations:
The patient experiences a for-eign body sensation. Usually this will be rather mild. Examination will reveal circumscribed conjunctival reddening or subconjunctival hemorrhage in the injured area. Occasionally only application of fluorescein dye to the injury will reveal the size of the conjunctival gap.
Treatment:
Minor conjunctival injuries do not require
treatment as the con-junctiva heals quickly. Larger lacerations with mobile
edges are approxi-mated with absorbable sutures.
The possibility of a perforating injury should
always be considered in conjunctival injuries. When the wound is treated, the
physician should inspect the underlying sclera after application of topical
anesthetic.
Corneal and Conjunctival Foreign Bodies
Epidemiology:
Foreign bodies on the cornea and conjunctiva
are the com-monest ocular emergency encountered by general practitioners and
ophthal-mologists.
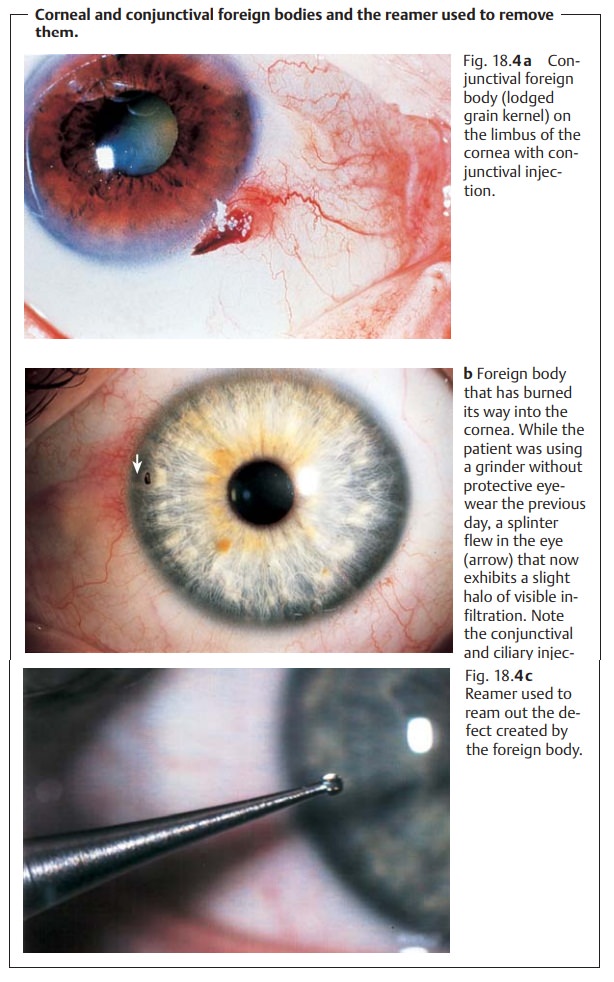
Etiology:
Airborne foreign bodies and metal splinters
from grinding or cut-ting disks in particular often become lodged in the
conjunctiva or cornea or burn their way into the tissue.
Symptoms and diagnostic considerations:
The patient experiences a for-eign-body sensation with every blink of the eye. This is accompanied by epi-phora (tearing) and blepharospasm. Depending on the time elapsed since the injury, i.e., after a few hours or several days, conjunctival or ciliary injection will be present (Figs. 18.4a and b). The foreign bodies on the conjunctiva or cornea are themselves often so small that they are visible only under loupe magnification. There may be visible infiltration or a ring of rust. Where there is no visible foreign body but fluorescein dye reveals vertical corneal stria-tions, the foreign body will be beneath the tarsus (see Fig. 5.11).
A foreign-body sensation with every blink of
the eye accompanied by epiphora, blepharospasm, and vertical striations on the
surface of the cornea are typical signs of a subtarsal foreign body.
Treatment:
Corneal and conjunctival foreign bodies.The foreign body ispried out of its bed with a
fine needle or cannula. The defect created by the foreign body will often be
contaminated with rust or infiltrated with leuko-cytes. This defect is
carefully reamed out with a drill (Fig. 18.4c)
and treated with an antibiotic eye ointment and bandaged if necessary.
Subtarsal foreign bodies.Everting the upper and lower eyelids will usuallyreveal the
foreign body, which may then be removed with a moist cotton swab. An antibiotic
eye bandage is placed until the patient is completely free of symptoms.
Corneal Erosion
Etiology:
This disorder follows initialtraumato the surface cornea, such asthe
fingernail of a child carried in the parent’s arms, a spiked-leaf palm tree, or
a branch that snaps back on to the eye. Properly treated, this epithelial
defect usually heals within a short time, i.e., 24 to 48 hours depending on the
size of the defect. However, occasionally
the epithelial cells do not properly adhere to Bowman’s layer so that the
epithelium repeatedly ruptures at the site of the initial injury. This
characteristically occurs in the morning when the patient wakes up and suddenly
opens his or her eyes. This recurring
ero-sion often creates severe emotional stress for the patient.
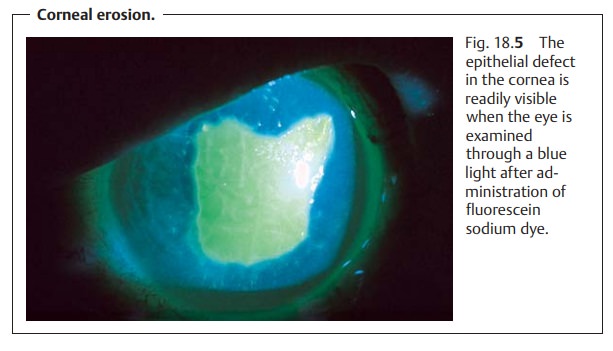
Symptoms and diagnostic considerations:
Immediately after the injury,the patient
experiences a severe foreign-body sensation associated with tear-ing. Because
there is actually a defect in the surface
of the cornea, the patient has the subjective sensation of a foreign body within the eye. The epithelial defect
causes severe pain, which immediately elicits a blepharospasm. Addi-tional
symptoms associated with corneal erosion include immediate eyelid swelling and
conjunctival injection. Fluorescein sodium dye will readily reveal the corneal
defect when the eye is examined through a blue light (Fig. 18.5).
Treatment:
An antibiotic ointment eye bandage is used.
Treatment of recurrent corneal erosion often
requires hospitalization. Bilateral bandages are placed to ensure that the eyes
are completely immobilized.
Blunt Ocular Trauma (Ocular Contusion)
Epidemiology and etiology:
Ocular contusions resulting from blunt
traumasuch as a fist, ball, champagne cork, stone, falling on the eye, or a
cow’s horn are very common. Significant deformation of the globe can result
where the diameter of the blunt object is less than that of the bony structures
of the orbit.
Clinical picture and diagnostic considerations:
Deformation exerts signifi-cant traction on intraocular structures and can cause them to tear. Often there will be blood in the anterior chamber, which will initially prevent the examiner from evaluating the more posterior intraocular structures.
Do not administer medications that act on the
pupil as there is a risk of irreversible mydriasis from a sphincter tear, and
pupillary movements increase the risk of subsequent bleeding. The posterior
intraocular structures should only be thoroughly examined in mydriasis to
deter-mine the extent of injury after a week to ten days.Common injuries are
listed in Table 18.1 and Fig. 18.6.
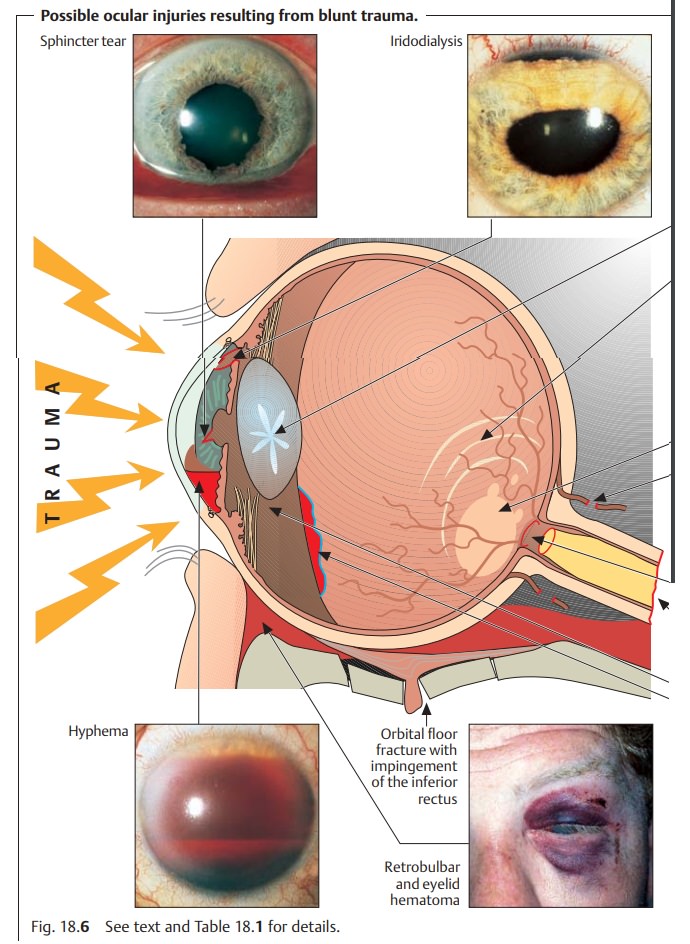
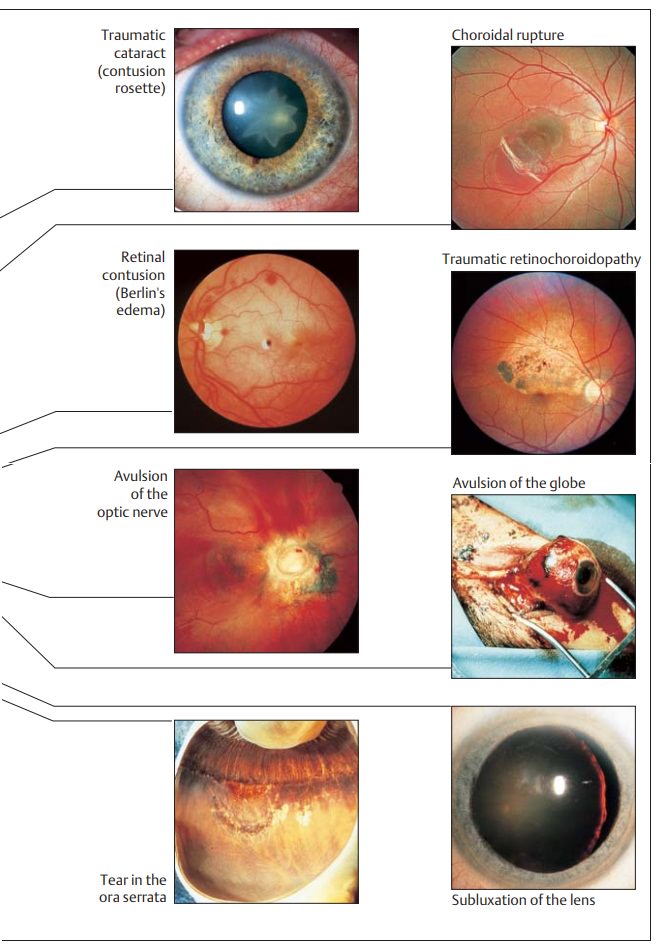
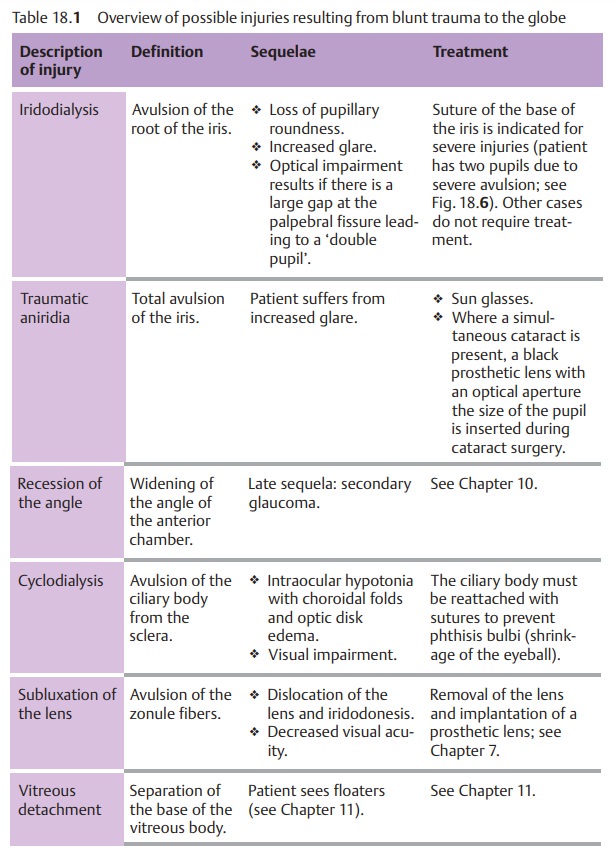
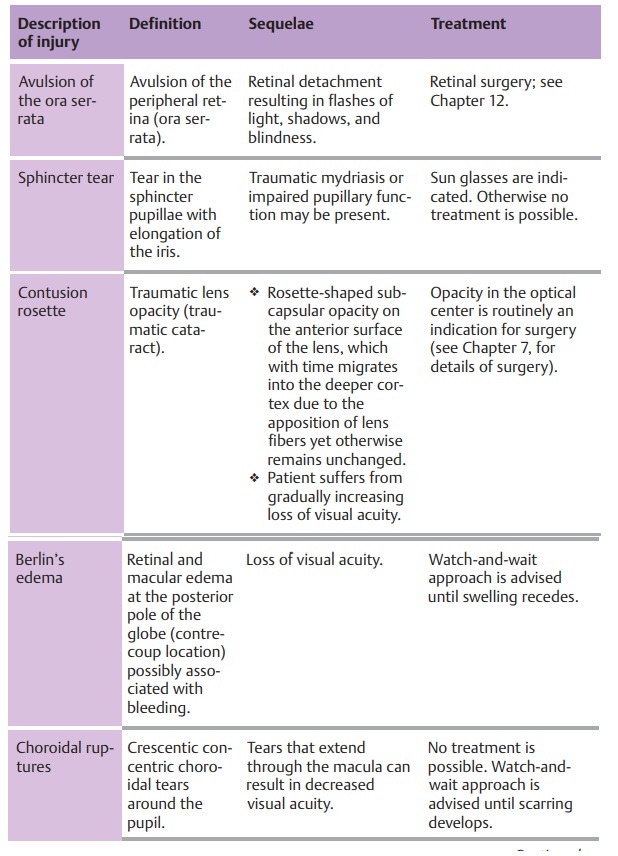
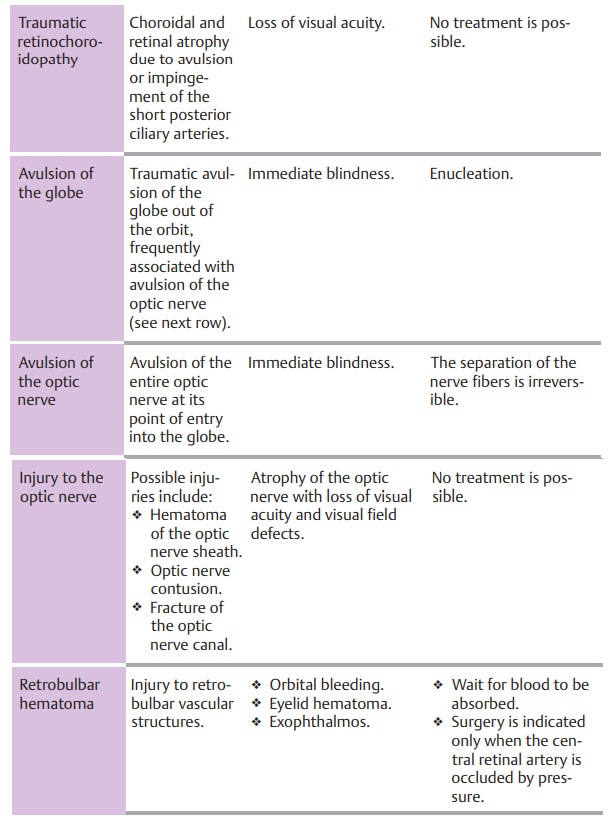
Late sequelae of blunt ocular trauma include:
âť– Secondary glaucoma.âť– Retinal detachment.âť– Cataract.
Late sequelae of blunt ocular trauma may occur
years after the injury.
Treatment:
This involves immobilizing the eye initially,
to allow intraocularblood to settle. See Table 18.1 for details.
Subsequent bleeding three or four days after
the injury is common.
Blow-out Fracture
Etiology (see also blunt ocular trauma):
Blow-out fractures of the orbit resultfrom
blunt trauma. Blunt objects of small diameter, such as a fist, tennis ball, or
baseball, can compress the contents of the orbit so severely that orbital wall
fractures. This fracture usually occurs where the bone is thinnest, alongthe paper-thin floor of the orbit over
the maxillary sinus. The ring-shaped bonyorbital rim usually remains
intact. The fracture can result in protrusion and impingement of orbital fat
and the inferior rectus and its sheaths in the frac-ture gap. Where the medial ethmoid wall fractures instead of
the orbital floor, emphysema in the eyelids will result.
Symptoms and diagnostic considerations:
The more severe the contusion,the more severe
the intraocular injuries and resulting visual impairment will be. Impingement
of the inferior rectus can result in diplopia,
especially in upward gaze. Initially, the diplopia may go unnoticed when the
eye is still swollen shut. A large bone defect may result in displacement of
larger por-tions of the contents of the orbital cavity. The eye may recede into
the orbit (enophthalmos) and the palpebral fissure may narrow. Injury to
the infraor-bital nerve, which courses along the floor of the orbit, may
result. This can cause hypesthesia of
the facial skin.
Crepitus upon palpation during examination of the eyelid swelling is a sign of emphysema due to collapse of the ethmoidal air cells. The crepitus is caused by air entering the orbit from the paranasal sinuses. The patient should refrain from blowing his or her nose for the next four or five days to avoid forcing air or germs into the orbit. Radiographs should be obtained and an ear, nose, and throat specialist consulted to help determine the exact location of the fracture. CT studies are more precise and may be indicatedto evaluate difficult cases.
Tissue displaced into the maxillary sinus will
resemble a hanging drop of water in the CT image.
Treatment:
Surgery to restore normal anatomy and the
integrity of the orbitshould be performed within ten days. This minimizes the
risk of irreversible damage from scarring of the impinged inferior rectus.
Where treatment is prompt, the prognosis is good.
Tetanus prophylaxis and treatment with
antibiotics are crucial.
Open-Globe Injuries
Etiology:
Together with severe chemical injuries,
open-globe injuries are themost devastating forms of ocular trauma. They are
caused by sharp objects that penetrate the cornea and sclera. A distinction is
made between penetra-tion with and without an intraocular foreign body.
However, even blunt trauma can cause an open-globe injury in an eye weakened by
previous surgery or injury where extremely high-energy forces are involved
(such as falling on a cane or a blow from a cow’s horn).
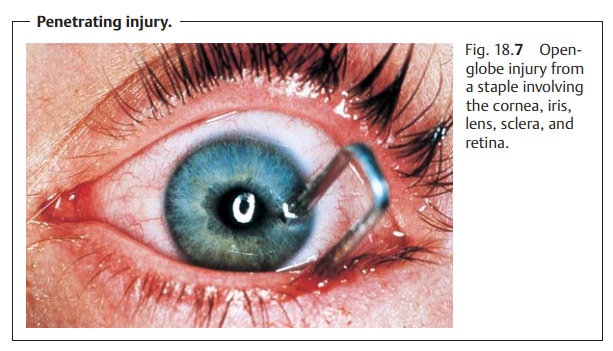
Clinical picture and diagnostic considerations:
Penetrating injuries coverthe entire spectrum
of clinical syndromes. Symptoms can range from massive penetration of the
cornea and sclera (Fig. 18.7) with
loss of the anterior cham-ber to tiny, nearly invisible injuries that close
spontaneously. The latter may include a fine penetrating wound or the entry
wound of a foreign body. Depending on the severity of the injury, the patient’s
visual acuity may be severely compromised or not influenced at all.
One of the most common sequelae is a traumatic cataract. The rupture in the lens capsule allows aqueous humor to
penetrate, causing the lens to swell. This results in lens opacification of
varying severity. Large defects will lead to total opacification of the lens
within hours or a few days. Smaller defects that close spontaneously often
cause a circumscribed opacity. Typically, penetra-tion results in a
rosette-shaped anterior or posterior subcapsular opacity.
Depending on the severity of the injury, the
following diagnostic signs will be present in an open-globe injury:
âť– The
anterior chamber will be shallow or absent.
âť– The pupil will be displaced toward the penetration site.
âť– Swelling of the lens will be present
(traumatic cataract).
âť–There will be bleeding in the anterior chamber
and vitreous body. âť– Hypotonia of the globe will be present.
The rupture of the lens capsule and vitreous
hemorrhage often render exami-nation difficult as they prevent direct
inspection. These cases, and any patient whose history suggests an intraocular
foreign body, require one or both of the following diagnostic imaging studies:
âť– Radiographs in two planes to determine
whether there is a foreign body in the eye.
âť– CT studies, that permit precise localization
of the foreign body and can also image radiolucent foreign bodies such as
plexiglas.
An injury sustained while working with a
hammer and chisel suggests an intraocular foreign body. The diagnosis may be
confirmed by exa-mining the fundus in mydriasis and obtaining radiographic
studies.
Treatment:
First aid.Where penetrating trauma is suspected, a sterile band-age should
be applied and the patient referred to an eye clinic for treatment. Tetanus
immunization or prophylaxis and prophylactic antibiotic treatment are indicated
as a matter of course.
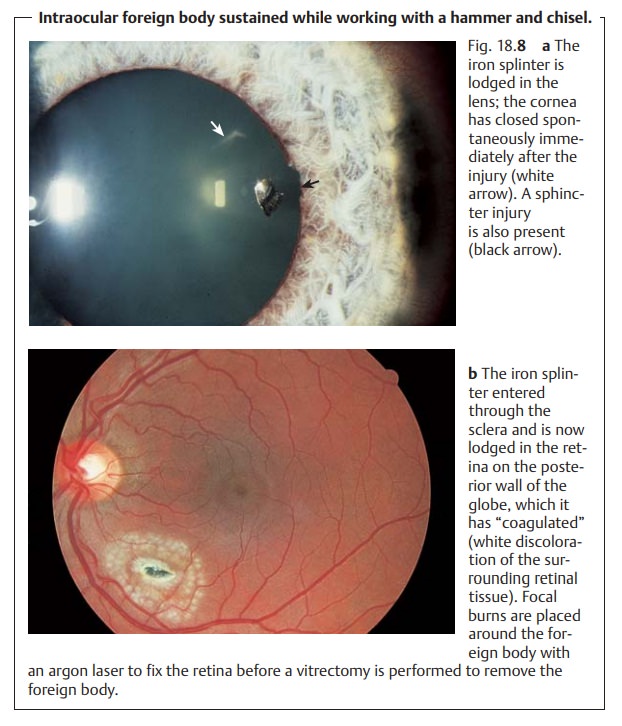
Surgery.Surgical treatment of penetrating injuries must include suturing
theglobe and reconstructing the anterior chamber. Any extruded intraocular
tissue (such as the iris) must be removed. Intraocular foreign bodies (Figs.
18.8a and b) should be removed when the wound is repaired (i.e., by
vit-rectomy and extraction of the foreign body).
Late sequelae:
âť–Improper reconstruction of the anterior chamber may lead to adhesionsbetween the iris and the
angle of the anterior chamber, resulting in sec-ondary angle closure glaucoma.
âť–Aretinal injury (for example at the site of the impact of the foreign body) can
lead to retinal detachment.
âť– Failure to remove iron foreign bodies can lead to ocular siderosis, which causes
irreparable damage to the receptors and may manifest itself years later.
âť– Copper foreign bodies cause severe inflammatory reactions in the eye(ocular chalcosis)
within a few hours. Symptoms range from uveitis and hypopyon to phthisis bulbi
(shrinkage and hypotonia of the eyeball).
âť– Organic foreign bodies (such as wood) in the eye lead to fulminantendophthalmitis.
Impalement Injuries of the Orbit
Etiology:
Impalement injuries occur most frequently in situations such asthese:
âť– Children may fall on pencils held in their
hands (Fig. 18.9).
âť– Injuries may result from the actions of other
persons (such as arrows or darts).
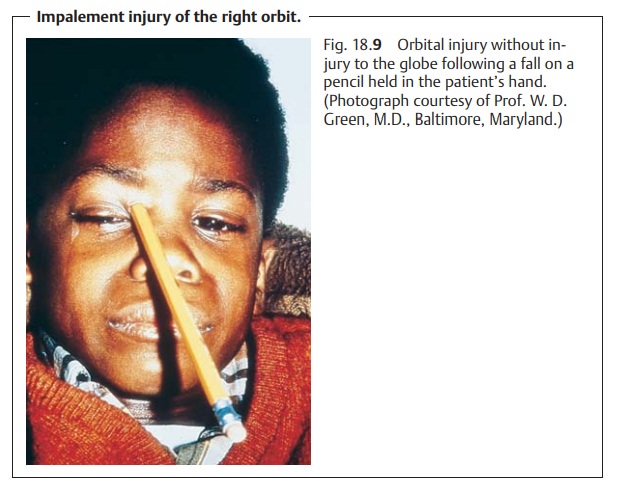
âť–A knife may slip while a butcher is removing a
bone from a cut of meat. Often the impaling “stake” will glance off the round
hard outer layer of the globe (cornea and
sclera) and lodge in the soft tissue of the orbit.
Symptoms and diagnostic considerations:
The stake can cause displace-ment of the globe. Often there will be minimal bleeding in the surrounding tissue. Diagnostic studies used to ascertain possible damage to intraocular structures include ophthalmoscopy, radiographic studies, and ultrasound.
Treatment:
First aid treatment should leave the stakein situ. Removing thestake could cause
severe bleeding and orbital hematoma. If necessary, the stake should be
stabilized before the patient is transported to the eye clinic. Once the
patient is in the clinic, the foreign body is removed from the orbit and the
integrity of the globe is verified, depending on specific findings. Any
bleeding is controlled. Prophylactic antibiotic treatment is indicated
routinely to minimize the risk of orbital cellulitis.
Related Topics