Chapter: Ophthalmology: Ocular Trauma
Eye Open-Globe Injuries
Open-Globe Injuries
Etiology:
Together with severe chemical injuries,
open-globe injuries are themost devastating forms of ocular trauma. They are
caused by sharp objects that penetrate the cornea and sclera. A distinction is
made between penetra-tion with and without an intraocular foreign body.
However, even blunt trauma can cause an open-globe injury in an eye weakened by
previous surgery or injury where extremely high-energy forces are involved
(such as falling on a cane or a blow from a cow’s horn).
Clinical picture and diagnostic considerations:
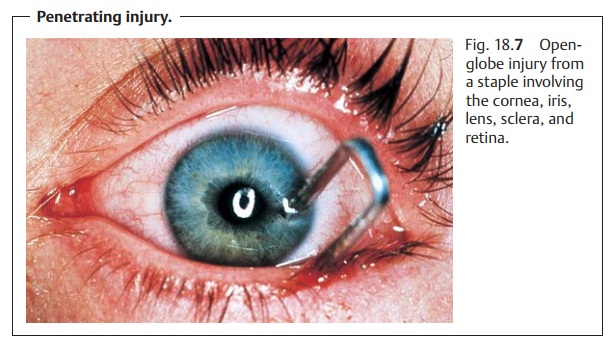
Penetrating injuries coverthe entire spectrum
of clinical syndromes. Symptoms can range from massive penetration of the
cornea and sclera (Fig. 18.7) with
loss of the anterior cham-ber to tiny, nearly invisible injuries that close
spontaneously. The latter may include a fine penetrating wound or the entry
wound of a foreign body. Depending on the severity of the injury, the patient’s
visual acuity may be severely compromised or not influenced at all.
One of the most common sequelae is a traumatic cataract. The rupture in the lens capsule allows aqueous humor to
penetrate, causing the lens to swell. This results in lens opacification of
varying severity. Large defects will lead to total opacification of the lens
within hours or a few days. Smaller defects that close spontaneously often
cause a circumscribed opacity. Typically, penetra-tion results in a
rosette-shaped anterior or posterior subcapsular opacity.
Depending on the severity of the injury, the
following diagnostic signs will be present in an open-globe injury:
âť– The
anterior chamber will be shallow or absent.
âť– The pupil will be displaced toward the penetration site.
âť– Swelling of the lens will be present
(traumatic cataract).
âť–There will be bleeding in the anterior chamber and vitreous body.
âť– Hypotonia of the globe will be present.
The rupture of the lens capsule and vitreous
hemorrhage often render exami-nation difficult as they prevent direct
inspection. These cases, and any patient whose history suggests an intraocular
foreign body, require one or both of the following diagnostic imaging studies:
âť– Radiographs in two planes to determine
whether there is a foreign body in the eye.
âť– CT studies, that permit precise localization
of the foreign body and can also image radiolucent foreign bodies such as
plexiglas.
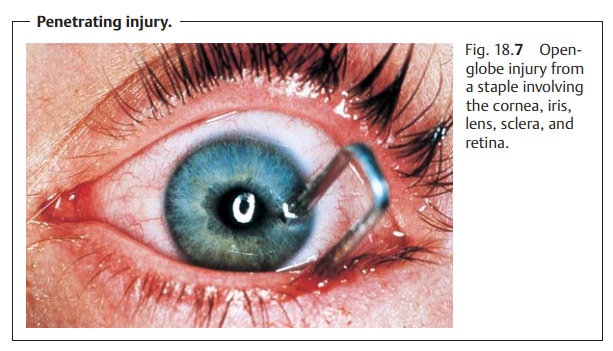
An injury sustained while working with a
hammer and chisel suggests an intraocular foreign body. The diagnosis may be
confirmed by exa-mining the fundus in mydriasis and obtaining radiographic
studies.
Treatment:
First aid.Where penetrating trauma is suspected, a sterile band-age should
be applied and the patient referred to an eye clinic for treatment. Tetanus
immunization or prophylaxis and prophylactic antibiotic treatment are indicated
as a matter of course.
Surgery.Surgical treatment of penetrating injuries must include suturing
theglobe and reconstructing the anterior chamber. Any extruded intraocular
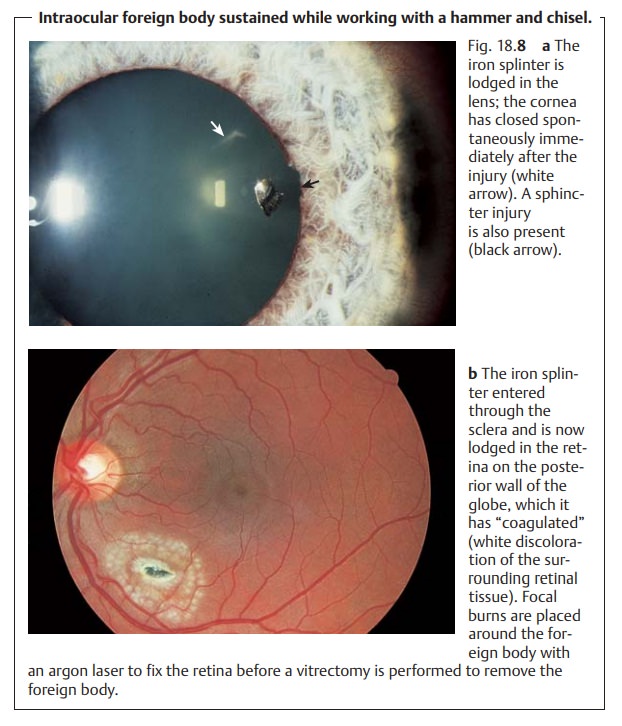
tissue (such as the iris) must be removed. Intraocular foreign bodies (Figs.
18.8a and b) should be removed when the wound is repaired (i.e., by
vit-rectomy and extraction of the foreign body).
Late sequelae:
âť–Improper reconstruction of the anterior chamber may lead to adhesionsbetween the iris and the
angle of the anterior chamber, resulting in sec-ondary angle closure glaucoma.
âť–Aretinal injury (for example at the site of the impact of the foreign body) can
lead to retinal detachment.
âť– Failure to remove iron foreign bodies can lead to ocular siderosis, which causes
irreparable damage to the receptors and may manifest itself years later.
âť– Copper foreign bodies cause severe inflammatory reactions in the eye(ocular chalcosis)
within a few hours. Symptoms range from uveitis and hypopyon to phthisis bulbi
(shrinkage and hypotonia of the eyeball).
âť– Organic foreign bodies (such as wood) in the eye lead to fulminantendophthalmitis.
Related Topics