Chapter: Basic & Clinical Pharmacology : Drugs Used in Heart Failure
Management of Chronic Heart Failure
MANAGEMENT OF CHRONIC HEART
FAILURE
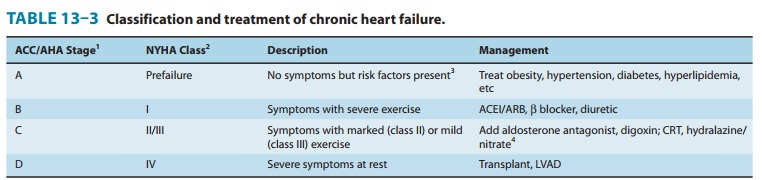
The major steps in the management of patients with chronic heart
failure are outlined in Table 13–3. The 2009 update to the ACC/ AHA 2005
guidelines suggests that treatment of patients at high risk (stages A and B)
should be focused on control of hyperten-sion, hyperlipidemia, and diabetes, if
present. Once symptoms and signs of failure are present, stage C has been
entered, and active treatment of failure must be initiated.
SODIUM REMOVAL
Sodium
removal—by dietary salt restriction and a diuretic—is the mainstay in management
of symptomatic heart failure, especially if edema is present. In very mild
failure a thiazide diuretic may be
tried, but a loop agent such as furosemide
is usually required. Sodium loss causes secondary loss of potassium, which is
particu-larly hazardous if the patient is to be given digitalis. Hypokalemia
can be treated with potassium supplementation or through the addition of an ACE
inhibitor or a potassium-sparing diuretic such as spironolactone.
Spironolactone or eplerenone should probably be considered in all patients with
moderate or severe heart failure, since both appear to reduce both morbidity
and mortality.
ACE INHIBITORS & ANGIOTENSIN RECEPTOR BLOCKERS
In
patients with left ventricular dysfunction but no edema, an ACE inhibitor
should be the first drug used. Several large studies have showed clearly that
ACE inhibitors are superior to both pla-cebo and to vasodilators and must be
considered, along with
VASODILATORS
Vasodilator drugs can be divided into selective arteriolar
dilators, venous dilators, and drugs with nonselective vasodilating effects.
The choice of agent should be based on the patient’s signs and symptoms and
hemodynamic measurements. Thus, in patients with high filling pressures in whom
the principal symptom is dyspnea, venous dilators such as long-acting nitrates will be most helpful in
reducing filling pressures and the symptoms of pulmo-nary congestion. In
patients in whom fatigue due to low left ven-tricular output is a primary
symptom, an arteriolar dilator such as hydralazine
may be helpful in increasing forward cardiac output.In most patients with
severe chronic failure that responds poorly to other therapy, the problem
usually involves both elevated filling pressures and reduced cardiac output. In
these circumstances, dila-tion of both arterioles and veins is required. In a
trial in African-American patients already receiving ACE inhibitors, addition
of hydralazine and isosorbide dinitrate reduced mortality. As a result, a fixed
combination of these two agents has been made available as isosorbide
dinitrate/hydralazine (BiDil), and
this is currently approved for use only in African Americans.
BETA BLOCKERS & ION CHANNEL BLOCKERS
Trials
of β-blocker
therapy in patients with heart failure are based on the hypothesis that
excessive tachycardia and adverse effects of high catecholamine levels on the
heart contribute to the down-ward course of heart failure. The results clearly
indicate that such therapy is beneficial if initiated cautiously at low doses,
even though acutely blocking the supportive effects of catecholamines can
worsen heart failure. Several months of therapy may be required before
improvement is noted; this usually consists of a slight rise in ejection
fraction, slower heart rate, and reduction in symptoms. As noted above, not all
β
blockers have proved useful, but bisoprolol,
carvedilol, metoprolol, and nebivolol
have been shown to reduce mortality.
In
contrast, the calcium-blocking drugs appear to have no role in the treatment of
patients with heart failure. Their depressant effects on the heart may worsen
heart failure. On the other hand, slowing of heart rate with ivabradine (an If blocker)
appears to be of benefit.
Digitalis
Digoxin is indicated in patients with heart failure
and atrial fibril-lation. It is usually given only when diuretics and ACE
inhibitors have failed to control symptoms. Only about 50% of patients with
normal sinus rhythm (usually those with documented systolic dysfunction) will
have relief of heart failure from digitalis. Better results are obtained in
patients with atrial fibrillation. If the deci-sion is made to use a cardiac
glycoside, digoxin is the one chosen in most cases (and the only one available
in the USA). When symptoms are mild, slow loading (digitalization) with
0.125–0.25 mg per day is safer and just as effective as the rapid method
(0.5–0.75 mg every 8 hours for three doses, followed by 0.125– 0.25 mg per
day).
Determining
the optimal level of digitalis effect may be diffi-cult. Unfortunately, toxic
effects may occur before the therapeutic end point is detected. Measurement of
plasma digoxin levels is useful in patients who appear unusually resistant or
sensitive; a level of 1 ng/mL or less is appropriate.
Because
it has a moderate but persistent positive inotropic effect, digitalis can, in
theory, reverse all the signs and symptoms of heart failure. Although the net
effect of the drug on mortality is mixed, it reduces hospitalization and deaths
from progressive heart failure at the expense of an increase in sudden death.
It is important to note that the mortality rate is reduced in patients with
serum digoxin concentrations of less than 0.9 ng/mL but increased in those with
digoxin levels greater than 1.5 ng/mL.
Other Clinical Uses of Digitalis
Digitalis
is useful in the management of atrial arrhythmias because of its
cardioselective parasympathomimetic effects. In atrial flutter and
fibrillation, the depressant effect of the drug on atrioventricu-lar conduction
helps control an excessively high ventricular rate. Digitalis has also been
used in the control of paroxysmal atrial andatrioventricular nodal tachycardia.
At present, calcium channel blockers and adenosine are preferred for this
application. Digoxin is explicitly contraindicated in patients with
Wolff-Parkinson-White syndrome and atrial fibrillation .
Toxicity
In
spite of its limited benefits and recognized hazards, digitalis is still
heavily used and toxicity is common. Therapy for toxicity manifested as visual
changes or gastrointestinal disturbances gen-erally requires no more than
reducing the dose of the drug. If cardiac arrhythmia is present and can be
ascribed to digitalis, more vigorous therapy may be necessary. Serum digitalis
and potassium levels and the electrocardiogram should always be monitored
dur-ing therapy of significant digitalis toxicity. Electrolyte status should be
corrected if abnormal (see above). Monitoring of potas-sium levels is
particularly important in patients on renal dialysis.
In
severe digitalis intoxication, serum potassium will already be elevated at the
time of diagnosis (because of potassium loss from the intracellular compartment
of skeletal muscle and other tis-sues). Furthermore, automaticity is usually
depressed, and antiar-rhythmic agents administered in this setting may lead to
cardiac arrest. Such patients are best treated with prompt insertion of a
temporary cardiac pacemaker catheter and administration of digi-talis
antibodies (digoxin immune fab).These
antibodies recog-nize digitoxin and cardiac glycosides from many other plants
in addition to digoxin. They are extremely useful in reversing severe
intoxication with most glycosides.
Digitalis-induced
arrhythmias are frequently made worse by cardioversion; this therapy should be
reserved for ventricular fibrillation if the arrhythmia is glycoside-induced.
CARDIAC RESYNCHRONIZATION THERAPY
Patients
with normal sinus rhythm and a wide QRS interval, eg, greater than 120 ms, have
impaired synchronization of right and left ventricular contraction. Poor
synchronization of ventricular contractionresultsindiminishedcardiacoutput.Resynchronization,
with left ventricular or biventricular pacing, has been shown to reduce
mortality in patients with chronic heart failure who were already receiving
optimal medical therapy.
Related Topics