Chapter: Basic & Clinical Pharmacology : Drugs Used in Heart Failure
Drugs Used in Heart Failure
Drugs Used in Heart Failure
Heart
failure occurs when cardiac output is inadequate to provide the oxygen needed
by the body. It is a highly lethal condition, with a 5-year mortality rate
conventionally said to be about 50%. The most common cause of heart failure in
the USA is coronary artery disease, with hypertension also an important factor.
Two major types of failure may be distinguished. Approximately 50% of younger
patients have systolic failure, with
reduced mechanical pumping action (contractility) and reduced ejection
fraction. The remaining group has diastolic
failure, with stiffening and loss of adequate relaxation playing a major
role in reducing filling and cardiac output; ejection fraction may be normal
even though stroke volume is significantly reduced. The proportion of patients
with diastolic failure increases with age. Because other cardiovas-cular
conditions (especially myocardial infarction) are now being treated more
effectively, more patients are surviving long enough for heart failure to
develop, making heart failure one of the cardio-vascular conditions that is
actually increasing in prevalence.Heart failure is a progressive disease that
is characterized by a gradual reduction in cardiac performance, punctuated in
many cases by episodes of acute decompensation, often requiring
hospitalization.
Treatment
is therefore directed at two somewhat different goals: (1) reducing symptoms
and slowing progression as much as possible during relatively stable periods
and (2) managing acute episodes of decompensated failure. These factors are
discussed in Clinical Pharmacology of Drugs Used in Heart Failure.
Although
it is believed that the primary defect in early systolic heart failure resides
in the excitation-contraction coupling machin-ery of the heart, the clinical
condition also involves many other processes and organs, including the baroreceptor
reflex, the sym-pathetic nervous system, the kidneys, angiotensin II and other
peptides, aldosterone, and apoptosis of cardiac cells. Recognition of these
factors has resulted in evolution of a variety of drug treat-ment strategies
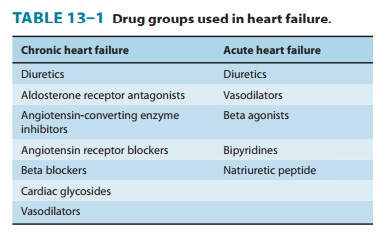
(Table 13–1).
Large clinical trials have shown that therapy directed at
non-cardiac targets is more valuable in the long-term treatment of heart
failure than traditional positive inotropic agents (cardiac glycosides
[digitalis]). Extensive trials have shown that ACE inhibitors, angiotensin
receptor blockers, certain β blockers, aldosterone receptor antagonists,
and combined hydralazine-nitrate therapy are the only agents in current use
that actually prolong life in patients with chronic heart failure. These
strategies are useful in both systolic and diastolic failure. Positive
inotropic drugs, on the other hand, are helpful mainly in acute systolic
fail-ure. Cardiac glycosides also reduce symptoms in chronic systolic heart
failure. Other positive inotropic drugs have consistently reduced survival in chronic failure, and their use is discouraged.
CASE STUDY
65-year-old man has developed shortness of breath with exertion several weeks after experiencing a viral illness. This is accompanied by swelling of the feet and ankles and increasing fatigue. On physical examination he is found to be mildly short of breath lying down, but feels better sitting upright. Pulse is 105 and regular, and blood pressure is 90/60 mm Hg. His lungs show crackles at both bases, and his jugular venous pressure is elevated. The liver is enlarged, and there is 3+ edema of the ankles and feet. An echocardiogram shows a dilated, poorly contracting heart with a left ventricu-lar ejection fraction of about 20% (normal: 60%). The pre-sumptive diagnosis is dilated cardiomyopathy secondary to a viral infection with stage C, class III heart failure. What treat-ment is indicated?
CASE STUDY ANSWER
The
patient has a low ejection fraction with systolic heart failure. He was placed
on a low-sodium diet and treated with a diuretic (furosemide 40 mg twice
daily). On this therapy, he was less short of breath on exertion and could also
lie flat without dyspnea. An angiotensin-converting enzyme (ACE) inhibitor was
added (enalapril 20 mg twice daily), and over the next few weeks, he continued
to feel better. Because of continued shortness of breath on exercise, digoxin
0.25 mg/d was added with a further improvement in exercise tolerance. Addition
of a β
blocker and eplerenone is being considered.
Related Topics