Chapter: Basic & Clinical Pharmacology : Drugs Used in Heart Failure
Drugs Without Positive Inotropic Effects Used in Heart Failure
DRUGS WITHOUT POSITIVE INOTROPIC
EFFECTS USED IN HEART FAILURE
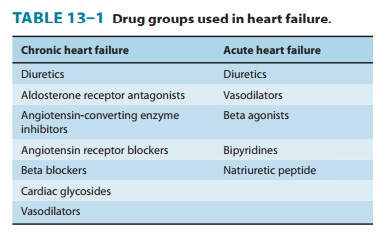
These agents—not positive inotropic drugs—are the first-line
therapies for chronic heart failure. The drugs most commonly used are
diuretics, ACE inhibitors, angiotensin receptor antago-nists, aldosterone
antagonists, and β
blockers (Table 13–1). In acute failure, diuretics and vasodilators play
important roles.
DIURETICS
Diuretics,
especially furosemide, are drugs of choice in heart failure. They have no
direct effect on cardiac contractility; their major mechanism of action in
heart failure is to reduce venous pressure and ventricular preload. This
results in reduction of salt and water retention and edema and its symptoms.
The reduction of cardiac size, which leads to improved pump efficiency, is of
major importance in systolic fail-ure. Spironolactone
and eplerenone, the aldosterone
antagonist diuretics , have the additional benefit of decreasing morbidity and
mortality in patients with severe heart failure who are also receiving ACE
inhibitors and other standard therapy. One possible mechanism for this benefit
lies in accumulating evidence that aldosterone may also cause myocardial and
vascular fibrosis and baroreceptor dysfunction in addition to its renal
effects.
ANGIOTENSIN-CONVERTING ENZYME INHIBITORS, ANGIOTENSIN RECEPTOR BLOCKERS, & RELATED AGENTS
ACE
inhibitors such as captopril are
introduced in earily. These versatile drugs reduce peripheral resistance and
thereby reduce afterload; they also reduce salt and water retention (by
reducing aldosterone secretion) and in that way reduce preload. The reduction
in tissue angiotensin levels also reduces sympathetic activity through
diminution of angio-tensin’s presynaptic effects on norepinephrine release.
Finally, these drugs reduce the long-term remodeling of the heart and vessels,
an effect that may be responsible for the observed reduction in mortal-ity and
morbidity (see Clinical Pharmacology).
Angiotensin
AT1 receptor blockers such as losartan appear to have similar but more limited
beneficial effects. Angiotensin receptor blockers should be consid-ered in
patients intolerant of ACE inhibitors because of incessant cough. In some
trials, candesartan was beneficial
when added to an ACE inhibitor.
Aliskiren, a renin inhibitor recently approved for
hyperten-sion, is in clinical trials for heart failure. Preliminary results
sug-gest an efficacy similar to that of ACE inhibitors.
VASODILATORS
Vasodilators
are effective in acute heart failure because they pro-vide a reduction in
preload (through venodilation), or reduction in afterload (through arteriolar
dilation), or both. Some evidence suggests that long-term use of hydralazine
and isosorbide dinitrate can also reduce damaging remodeling of the heart.
A
synthetic form of the endogenous peptide brain natriuretic peptide (BNP) is
approved for use in acute (not chronic) cardiac failure as nesiritide. This recombinant product increases cGMP in smooth
muscle cells and reduces venous and arteriolar tone in experimental
preparations. It also causes diuresis. The peptide has a short half-life of
about 18 minutes and is administered as a bolusintravenous dose followed by
continuous infusion. Excessive hypotension is the most common adverse effect.
Reports of sig-nificant renal damage and deaths have resulted in extra warnings
regarding this agent, and it should be used with great caution.
Plasma
concentrations of endogenous BNP rise
in most patients with heart failure and are correlated with severity.
Measurement of plasma BNP has become a useful diagnostic or prognostic test in
some centers.
Related
peptides include atrial natriuretic peptide (ANP) and urodilatin, a similar
peptide produced in the kidney. Carperitide
and ularitide, respectively, are
investigational synthetic analogs of theseendogenous peptides and are in
clinical trials .
Bosentan and
tezosentan, orally active competitive inhibitorsof endothelin , have been
shown to have some benefits in experimental animal models with heart failure,
but results in human trials have been disappointing. Bosentan is approved for
use in pulmonary hypertension . It has significant teratogenic and hepatotoxic
effects.
BETA-ADRENOCEPTOR BLOCKERS
Most
patients with chronic heart failure respond favorably to cer-tain β blockers in spite of
the fact that these drugs can precipitate acute decompensation of cardiac
function . Studies with bisoprolol,
carvedilol, metoprolol, and nebivolol
showed a reduction in mortality in patients with stable severe heart failure,
but this effect was not observed with another β blocker, bucindolol. A full understanding of
the beneficial action of β blockade is lacking, but suggested mechanisms
include attenuation of the adverse effects of high concentrations of
cate-cholamines (including apoptosis), up-regulation of β receptors, decreased
heart rate, and reduced remodeling through inhibition of the mitogenic activity
of catecholamines.
Related Topics