Chapter: Basic & Clinical Pharmacology : The Alcohols
Management of Alcohol Withdrawal Syndrome
MANAGEMENT OF ALCOHOL WITHDRAWAL SYNDROME
Abrupt
alcohol discontinuation in an individual with alcohol dependence leads to a
characteristic syndrome of motor agitation, anxiety, insomnia, and reduction of
seizure threshold. The severity of the syndrome is usually proportionate to the
degree and dura-tion of alcohol abuse. However, this can be greatly modified by
the use of other sedatives as well as by associated factors (eg, diabetes,
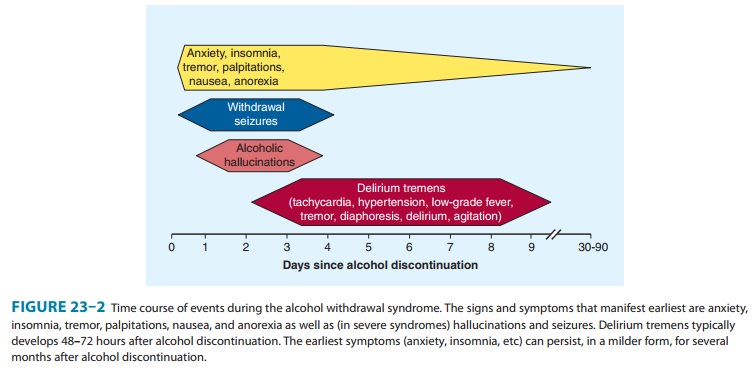
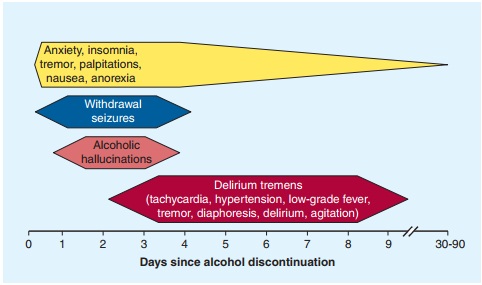
In its mildest form, the alcohol withdrawal syndrome of increased pulse and
blood pressure, tremor, anxiety, and insomnia occurs 6–8 hours after alcohol
consumption is stopped (Figure 23–2). These effects usually lessen in 1–2 days,
although some such as anxiety and sleep disturbances can be seen at decreasing
levels for several months. In some patients, more severe acute reactions occur,
with patients at risk of withdrawal seizures or alcoholic hal-lucinations
during the first 1–5 days of withdrawal. Alcohol with-drawal is one of the most
common causes of seizures in adults. Several days later, individuals can
develop the syndrome of delirium tremens, which is characterized by delirium,
agitation, autonomic nervous system instability, low-grade fever, and
diaphoresis.The major objective of drug therapy in the alcohol withdrawal
period is prevention of seizures, delirium, and arrhythmias. Potassium,
magnesium, and phosphate balance should be restored as rapidly as is consistent
with renal function. Thiamine therapy is initiated in all cases. Individuals in
mild alcohol withdrawal do not need any other pharmacologic assistance.Specific
drug treatment for detoxification in more severe cases involves two basic
principles: substituting a long-acting sedative-hypnotic drug for alcohol and
then gradually reducing (“taper-ing”) the dose of the long-acting drug. Because
of their wide margin of safety, benzodiazepines are preferred. The choice of a
specific agent in this class is generally based on pharmacokinetic or economic
considerations. Long-acting benzodiazepines, includ-ing chlordiazepoxide and
diazepam, have the advantage of requir-ing less frequent dosing. Since their
pharmacologically active metabolites are eliminated slowly, the long-acting
drugs provide a built-in tapering effect. A disadvantage of the long-acting
drugs is that they and their active metabolites may accumulate, especially in
patients with compromised liver function. Short-acting drugs such as lorazepam
and oxazepam are rapidly converted to inactive water-soluble metabolites that
will not accumulate, and for thisreason the short-acting drugs are especially
useful in alcoholic patients with liver disease. Benzodiazepines can be
administered orally in mild or moderate cases, or parenterally for patients
with more severe withdrawal reactions.After the alcohol withdrawal syndrome has
been treated acutely, sedative-hypnotic medications must be tapered slowly over
several weeks. Complete detoxification is not achieved with just a few days of
alcohol abstinence. Several months may be required for restoration of normal
nervous system function, espe-cially sleep.
Related Topics