Chapter: Basic & Clinical Pharmacology : Dermatologic Pharmacology
Keratolytic & Destructive Agents
KERATOLYTIC & DESTRUCTIVE AGENTS
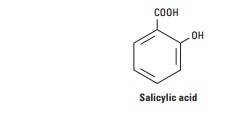
SALICYLIC ACID
Salicylic acid has
been extensively used in dermatologic therapy as a keratolytic agent. The
mechanism by which it produces its kera-tolytic and other therapeutic effects
is poorly understood. The drug may solubilize cell surface proteins that keep
the stratum corneum intact, thereby resulting in desquamation of keratotic
debris. Salicylic acid is keratolytic in concentrations of 3–6%. In
concentrations greater than 6%, it can be destructive to tissues.
Salicylism and death
have occurred following topical applica-tion. In an adult, 1 g of a topically
applied 6% salicylic acid preparation will raise the serum salicylate level not
more than 0.5 mg/dL of plasma; the threshold for toxicity is 30–50 mg/dL.
Higher serum levels are possible in children, who are therefore at a greater
risk for salicylism. In cases of severe intoxication, hemo-dialysis is the
treatment of choice . It is advisable to limit both the total amount of
salicylic acid applied and the frequency of application.
Urticarial, anaphylactic, and erythema multiforme reactions may occur in
patients who are allergic to salicylates. Topical use may be associated with local
irritation, acute inflammation, and even ulceration with the use of high
concentrations of salicylic acid. Particular care must be exercised when using
the drug on the extremities of patients with diabetes or peripheral vascular
disease.
PROPYLENE GLYCOL
Propylene glycol is
used extensively in topical preparations because it is an excellent vehicle for
organic compounds. It has been used alone as a keratolytic agent in 40–70%
concentrations, with plas-tic occlusion, or in gel with 6% salicylic acid.
Only minimal amounts
of a topically applied dose are absorbed through normal stratum corneum.
Percutaneously absorbed pro-pylene glycol is oxidized by the liver to lactic
acid and pyruvic acid, with subsequent utilization in general body metabolism.
Approximately 12–45% of the absorbed agent is excreted unchanged in the urine.
Propylene
glycol is an effective keratolytic agent for the removal of hyperkeratotic
debris. It is also an effective humectant and increases the water content of
the stratum corneum. The hygro-scopic characteristics of propylene glycol may
help it to develop an osmotic gradient through the stratum corneum, thereby
increas-ing hydration of the outermost layers by drawing water out from the
inner layers of the skin.
Propylene glycol is
used under polyethylene occlusion or with 6% salicylic acid for the treatment
of ichthyosis, palmar and plan-tar keratodermas, psoriasis, pityriasis rubra
pilaris, keratosis pilaris, and hypertrophic lichen planus.
In
concentrations greater than 10%, propylene glycol may act as an irritant in
some patients; those with eczematous dermatitis may be more sensitive. Allergic
contact dermatitis occurs with propylene glycol, and a 4% aqueous propylene
glycol solution is recommended for the purpose of patch testing.
UREA
Urea in a compatible
cream vehicle or ointment base has a soft-ening and moisturizing effect on the
stratum corneum. It has the ability to make creams and lotions feel less
greasy, and this has been utilized in dermatologic preparations to decrease the
oily feel of a preparation that otherwise might feel unpleasant. It is a white
crystalline powder with a slight ammonia odor when moist.
Urea is absorbed
percutaneously, although the amount absorbed is minimal. It is distributed
predominantly in the extracellular space and excreted in urine. Urea is a
natural product of metabo-lism, and systemic toxicities with topical
application do not occur.
Urea increases the
water content of the stratum corneum, pre-sumably as a result of the
hygroscopic characteristics of this natu-rally occurring molecule. Urea is also
keratolytic. The mechanism of action appears to involve alterations in
prekeratin and keratin, leading to increased solubilization. In addition, urea
may break hydrogen bonds that keep the stratum corneum intact.
As a humectant, urea
is used in concentrations of 2–20% in creams and lotions. As a keratolytic
agent, it is used in 20% con-centration in diseases such as ichthyosis
vulgaris, hyperkeratosis of palms and soles, xerosis, and keratosis pilaris.
Concentrations of 30–50% applied to the nail plate have been useful in
softening the nail prior to avulsion.
PODOPHYLLUM RESIN & PODOFILOX
Podophyllum resin, an alcoholic extract of Podophyllum peltatum, commonly known as mandrake root or May apple,
is used in the treatment of condyloma acuminatum and other verrucae. It is a
mixture of podophyllotoxin, α and β peltatin, desoxypodophyl-lotoxin,
dehydropodophyllotoxin, and other compounds. It is soluble in alcohol, ether,
chloroform, and compound tincture of benzoin.
Percutaneous
absorption of podophyllum resin occurs, par-ticularly in intertriginous areas
and from applications to large moist condylomas. It is soluble in lipids and
therefore is distrib-uted widely throughout the body, including the central
nervous system.
The major use of
podophyllum resin is in the treatment of condyloma acuminatum. Podophyllotoxin
and its derivatives are active cytotoxic agents with specific affinity for the
microtubule protein of the mitotic spindle. Normal assembly of the spindle is
prevented, and epidermal mitoses are arrested in metaphase. A 25% concentration
of podophyllum resin in compound tincture of benzoin is recommended for the
treatment of condyloma acuminatum. Application should be restricted to wart tissue
only, to limit the total amount of medication used and to prevent severe
erosive changes in adjacent tissue. In treating cases of large condy-lomas, it
is advisable to limit application to sections of the affected area to minimize
systemic absorption. The patient is instructed to wash off the preparation 2–3
hours after the initial application, because the irritant reaction is variable.
Depending on the indi-vidual patient’s reaction, this period can be extended to
6–8 hours on subsequent applications. If three to five applications have not
resulted in significant resolution, other methods of treatment should be
considered.
Toxic
symptoms associated with excessively large applications include nausea,
vomiting, alterations in sensorium, muscle weak-ness, neuropathy with
diminished tendon reflexes, coma, and even death. Local irritation is common,
and inadvertent contact with the eye may cause severe conjunctivitis. Use
during preg-nancy is contraindicated in view of possible cytotoxic effects on
the fetus.
Pure podophyllotoxin
(podofilox) is approved for use as either a 0.5% solution or gel (Condylox) for
application by the patient in the treatment of genital condylomas. The low
concentration of podofilox significantly reduces the potential for systemic toxicity.
Most men with penile warts may be treated with less than 70 μL per application.
At this dose, podofilox is not routinely detectedin the serum. Treatment is
self-administered in treatment cycles of twice-daily application for 3
consecutive days followed by a 4-day drug-free period. Local adverse effects
include inflammation, ero-sions, burning pain, and itching.
SINECATECHINS
Sinecatechins 15%
ointment (Veregen) is a prescription botanical drug product of a partially
purified fraction of the water extract of green tea leaves from Camellia sinensis containing a mixture
of catechins. Sinecatechins ointment is indicated for the topical treat-ment of
external genital and perianal warts in immunocompetent patients 18 years and
older. The mechanism of action is unknown. Sinecatechins ointment should be
applied three times daily to the warts until complete clearance, not to exceed
16 weeks of therapy.
FLUOROURACIL
Fluorouracil is a
fluorinated pyrimidine antimetabolite that resembles uracil, with a fluorine atom
substituted for the 5-methyl group. Fluorouracil is used topically for the
treatment of multiple actinic keratoses.
Approximately
6% of a topically applied dose is absorbed—an amount insufficient to produce
adverse systemic effects. Most of the absorbed drug is metabolized and excreted
as carbon dioxide, urea, and α-fluoro-β-alanine. A small percentage is
eliminated unchanged in the urine. Fluorouracil inhibits thymidylate
syn-thetase activity, interfering with the synthesis of DNA and, to a lesser
extent, RNA. These effects are most marked in atypical, rapidly proliferating
cells.
Fluorouracil is
available in multiple formulations containing 0.5%, 1%, 2%, and 5%
concentrations. The response to treatment begins with erythema and progresses
through vesiculation, erosion, superficial ulceration, necrosis, and finally
reepithelialization. Fluorouracil should be continued until the inflammatory
reaction reaches the stage of ulceration and necrosis, usually in 3–4 weeks, at
which time treatment should be terminated. The healing process may continue for
1–2 months after therapy is discontinued. Local adverse reactions may include
pain, pruritus, a burning sensation, tenderness, and residual postinflammatory
hyperpigmentation. Excessive exposure to sunlight during treatment may increase
the intensity of the reaction and should be avoided. Allergic contact
dermatitis to fluorouracil has been reported, and its use is contrain-dicated
in patients with known hypersensitivity.
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
A topical 3% gel
formulation of the nonsteroidal anti-inflamma-tory drug diclofenac (Solaraze)
has shown moderate effectiveness in the treatment of actinic keratoses. The
mechanism of action isunknown. As with other NSAIDs, anaphylactoid reactions
may occur with diclofenac, and it should be given with caution to patients with
known aspirin hypersensitivity .
AMINOLEVULINIC ACIDS
Aminolevulinic acid
(ALA) is an endogenous precursor of photo-sensitizing porphyrin metabolites.
When exogenous ALA is pro-vided to the cell through topical applications,
protoporphyrin IX (PpIX) accumulates in the cell. When exposed to light of
appro-priate wavelength and energy, the accumulated PpIX produces a
photodynamic reaction resulting in the formation of cytotoxic superoxide and
hydroxyl radicals. Photosensitization of actinic keratoses using ALA (Levulan
Kerastick) and illumination with a blue light photodynamic therapy illuminator
(BLU-U) is the basis for ALA photodynamic therapy.
Treatment
consists of applying ALA 20% topical solution to individual actinic keratoses
followed by blue light photodynamic illumination 14–18 hours later. Transient
stinging or burning at the treatment site occurs during the period of light
exposure. Patients must avoid
exposure to sunlight or bright indoor lights for at least 40 hours after ALA
application. Redness, swelling, and crusting of the actinic keratoses will
occur and gradually resolve over a 3- to 4-week time course. Allergic contact
dermatitis to methyl ester may occur.
Related Topics