Chapter: Basic & Clinical Pharmacology : Dermatologic Pharmacology
Dermatologic Pharmacology
Dermatologic Pharmacology
Diseases of the skin offer special opportunities to the clinician. In particular, the topical administration route is especially appropriate for skin diseases, although some dermatologic diseases respond as well or better to drugs administered systemically.
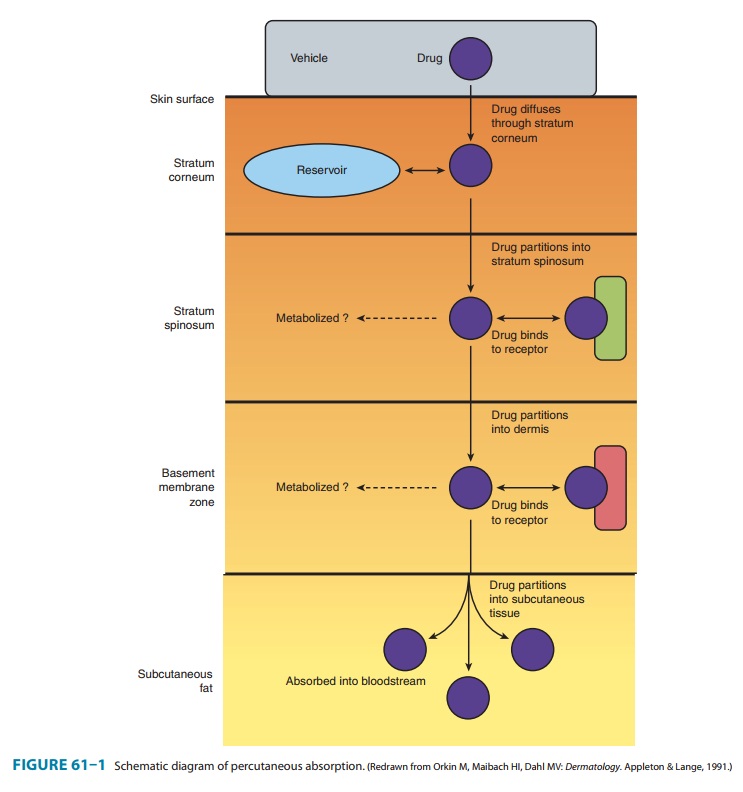
The
general pharmacokinetic principles governing the use of drugs applied to the
skin are the same as those involved in other routes of administration. Although
often depicted as a simple three-layered structure (Figure 61–1), human skin is
a complex series of diffusion barriers. Quantitation of the flux of drugs and
drug vehicles through these barriers is the basis for pharmacokinetic analysis
of dermatologic therapy, and tech-niques for making such measurements are
rapidly increasing in number and sensitivity.
Major variables that
determine pharmacologic response to drugs applied to the skin include the
following:
Regional variation in drug
penetration: For example, thescrotum, face, axilla, and scalp are
far more permeable than the forearm and may require less drug for equivalent
effect.
Concentration gradient: Increasing
the concentration gradi-ent increases the mass of drug transferred per unit
time, just as in the case of diffusion across other barriers . Thus, resistance
to topical corticosteroids can sometimes be overcome by use of higher
concentrations of drug.
Dosing schedule: Because of its physical properties, the skinacts as a reservoir
for many drugs. As a result, the “local half-life” may be long enough to permit
once-daily application of drugs with short systemic half-lives. For example,
once-daily application of corticosteroids appears to be just as effective as
multiple applications in many conditions.
Vehicles
and occlusion: An
appropriate vehicle maximizes theability of the drug to penetrate the outer
layers of the skin. In addition, through their physical properties (moistening
or dry-ing effects), vehicles may themselves have important therapeu-tic
effects. Occlusion (application of a plastic wrap to hold the drug and its
vehicle in close contact with the skin) is extremely effective in maximizing
efficacy.
REACTIONS TO DERMATOLOGIC MEDICATIONS
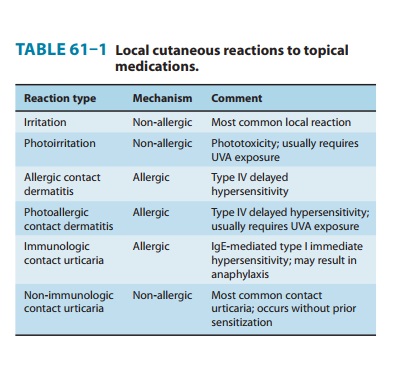
The skin reacts to
many systemic medications with a variety of symptom-generating responses. In
addition, some dermatologic medications themselves cause skin reactions. The
major types of reactions are summarized in Table 61–1.
CASE STUDY
A 22-year-old woman presents with a complaint of worsen-ing psoriasis. She has a strong family history of the disease and has had lesions on her scalp and elbows for several years. She recently noted new lesions developing on her knees andthe soles of her feet. She has been using topical over-the-counter hydrocortisone cream but admits that this treatment does not seem to help. What therapeutic options are available for the treatment of this chronic disease?
CASE STUDY
A
21-year-old woman comes with her parents to discuss therapeutic options for her
Crohn’s disease. She was diag-nosed with Crohn’s disease 2 years ago, and it
involves her terminal ileum and proximal colon, as confirmed by colonos-copy
and small bowel radiography. She was initially treated with mesalamine and
budesonide with good response, but over the last 2 months, she has had a
relapse of her symp-toms. She is experiencing fatigue, cramping, abdominal
pains, and nonbloody diarrhea up to 10 times daily, and she has had a 15-lb
weight loss.She has no other significant medical or surgical history. Her
current medications are mesalamine 2.4 g/d and budes-onide 9 mg/d. She appears
thin and tired. Abdominal exam-ination reveals tenderness without guarding in
the right lower quadrant; no masses are palpable. On perianal exami-nation,
there is no tenderness, fissure, or fistula. Her labora-tory data are notable
for anemia and elevated C-reactive protein. What are the options for immediate
control of her symptoms and disease? What are the long-term management options?
Related Topics