Chapter: Basic & Clinical Pharmacology : Dermatologic Pharmacology
Acne Preparations
ACNE PREPARATIONS
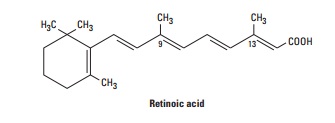
RETINOIC ACID & DERIVATIVES
Retinoic
acid, also known as tretinoin or all-trans-retinoic acid, is the acid
form of vitamin A. It is an effective topical treatment for acne vulgaris.
Several analogs of vitamin A, eg, 13-cis-retinoic
acid (isotretinoin), have been shown to be effective in various dermato-logic
diseases when given orally. Vitamin A alcohol is the physio-logic form of
vitamin A. The topical therapeutic agent, retinoicacid,
is formed by the oxidation of the alcohol group, with all fourdouble bonds
in the side chain in the trans
configuration as shown.
Retinoic acid is
insoluble in water but soluble in many organic solvents. Topically applied
retinoic acid remains chiefly in the epi-dermis, with less than 10% absorption
into the circulation. The small quantities of retinoic acid absorbed following
topical applica-tion are metabolized by the liver and excreted in bile and
urine.
Retinoic
acid has several effects on epithelial tissues. It stabi-lizes lysosomes,
increases ribonucleic acid polymerase activity, increases prostaglandin E2,
cAMP, and cGMP levels, and increases the incorporation of thymidine into DNA.
Its action in acne has been attributed to decreased cohesion between epidermal
cells and increased epidermal cell turnover. This is thought to result in the
expulsion of open comedones and the transformation of closed comedones into
open ones.
Topical retinoic acid
is applied initially in a concentration suf-ficient to induce slight erythema
with mild peeling. The concen-tration or frequency of application may be
decreased if too much irritation occurs. Topical retinoic acid should be
applied to dry skin only, and care should be taken to avoid contact with the
corners of the nose, eyes, mouth, and mucous membranes. During the first 4–6
weeks of therapy, comedones not previously evident may appear and give the
impression that the acne has been aggra-vated by the retinoic acid. However,
with continued therapy, the lesions will clear, and in 8–12 weeks optimal
clinical improvement should occur. A timed-release formulation of tretinoin
containing microspheres (Retin-A Micro) delivers the medication over time and
may be less irritating for sensitive patients.
The effects of
tretinoin on keratinization and desquamation offer benefits for patients with
photo damaged skin. Prolonged use of tretinoin promotes dermal collagen
synthesis, new blood vessel formation, and thickening of the epidermis, which
helps diminish fine lines and wrinkles. Specially formulated moisturizing 0.05%
cream (Renova, Refissa) is marketed for this purpose.
The
most common adverse effects of topical retinoic acid are ery-thema and dryness
that occur in the first few weeks of use, but these can be expected to resolve
with continued therapy. Animal studies suggest that this drug may increase the
tumorigenic potential of ultra-violet radiation. In light of this, patients
using retinoic acid should be advised to avoid or minimize sun exposure and use
a protective sun-screen. Allergic contact dermatitis to topical retinoic acid
is rare.
Adapalene (Differin)
is a derivative of naphthoic acid that resem-bles retinoic acid in structure
and effects. It is available for daily appli-cation as a 0.1% gel, cream, or
lotion and a 0.3% gel. Unlike tretinoin, adapalene is photochemically stable
and shows little decrease in efficacy when used in combination with benzoyl
peroxide. Adapalene is less irritating than tretinoin and is most effective in
patients with mild to moderate acne vulgaris. Adapalene is also available in a
fixed-dose combination gel with benzoyl peroxide (Epiduo).
Tazarotene (Tazorac) is an acetylenic retinoid that is availableas a 0.1% gel
and cream for the treatment of mild to moderately severe facial acne. Topical
tazarotene should be used by women of childbearing age only after contraceptive
counseling. It is recom-mended that tazarotene should not be used by pregnant
women.
ISOTRETINOIN
Isotretinoin is a
synthetic retinoid currently restricted to the oral treatment of severe cystic
acne that is recalcitrant to standard therapies. The precise mechanism of
action of isotretinoin in cys-tic acne is not known, although it appears to act
by inhibiting sebaceous gland size and function. The drug is well absorbed,
extensively bound to plasma albumin, and has an elimination half-life of 10–20
hours.
Most patients with
cystic acne respond to 1–2 mg/kg, given in two divided doses daily for 4–5 months.
If severe cystic acne per-sists following this initial treatment, after a
period of 2 months, a second course of therapy may be initiated. Common adverse
effects resemble hypervitaminosis A and include dryness and itch-ing of the
skin and mucous membranes. Less common side effects are headache, corneal
opacities, pseudotumor cerebri, inflamma-tory bowel disease, anorexia,
alopecia, and muscle and joint pains. These effects are all reversible on
discontinuance of therapy. Skeletal hyperostosis has been observed in patients
receiving iso-tretinoin with premature closure of epiphyses noted in children
treated with this medication. Lipid abnormalities (triglycerides, high-density
lipoproteins) are frequent; their clinical relevance is unknown at present.
Teratogenicity is a
significant risk in patients taking isotretin-oin; therefore, women of
childbearing potential must use an
effec-tive form of contraception for at least 1 month before, throughout
isotretinoin therapy, and for one or more menstrual cycles follow-ing
discontinuance of treatment. A negative serum pregnancy test must be obtained within 2 weeks before
starting therapy in thesepatients, and therapy should be initiated only on the
second or third day of the next normal menstrual period. In the USA, health
care professionals, pharmacists, and patients must utilize the man-datory
iPLEDGE registration and follow-up system.
BENZOYL PEROXIDE
Benzoyl
peroxide is an effective topical agent in the treatment of acne vulgaris. It
penetrates the stratum corneum or follicular openings unchanged and is
converted metabolically to benzoic acid within the epidermis and dermis. Less
than 5% of an applied dose is absorbed from the skin in an 8-hour period. It
has been postulated that the mechanism of action of benzoyl peroxide in acne is
related to its antimicrobial activity against P acnes and to its peeling and comedolytic effects.
To decrease the
likelihood of irritation, application should be limited to a low concentration
(2.5%) once daily for the first week of therapy and increased in frequency and
strength if the prepara-tion is well tolerated. Fixed-combination formulations
of 5% benzoyl peroxide with 3% erythromycin base (Benzamycin) or 1% clindamycin
(BenzaClin, Duac), and 2.5% benzoyl peroxide with 1.2% clindamycin (Acanya) or
0.1% adapalene (Epiduo) appear to be more effective than individual agents
alone.
Benzoyl peroxide is a
potent contact sensitizer in experimental studies, and this adverse effect may
occur in up to 1% of acne patients. Care should be taken to avoid contact with
the eyes and mucous membranes. Benzoyl peroxide is an oxidant and may rarely
cause bleaching of the hair or colored fabrics.
AZELAIC ACID
Azelaic
acid is a straight-chain saturated dicarboxylic acid that is effective in the
treatment of acne vulgaris (in the form of Azelex) and acne rosacea (Finacea).
Its mechanism of action has not been fully determined, but preliminary studies
demonstrate antimicro-bial activity against P
acnes as well as in vitro inhibitory effects on the conversion of
testosterone to dihydrotestosterone. Initial therapy is begun with once-daily
applications of the 20% cream or 15% gel to the affected areas for 1 week and
twice-daily applications thereafter. Most patients experience mild irritation
with redness and drynessof the skin during the first week of treatment.
Clinical improvement is noted in 6–8 weeks of continuous therapy.
Related Topics