Chapter: Medical Physiology: Muscle Blood Flow and Cardiac Output During Exercise; the Coronary Circulation and schemic Heart Disease
Ischemic Heart Disease
Ischemic Heart Disease
The most common cause of death in Western culture is ischemic heart disease, which results from insufficient coronary blood flow. About 35 per cent of people in the United States die of this cause. Some deaths occur suddenly as a result of acute coronary occlusion or fibrillation of the heart, whereas other deaths occur slowly over a period of weeks to years as a result of progressive weakening of the heart pumping process. We discuss acute coronary ischemia caused by acute coronary occlusion and myocardialinfarction. We will discuss congestive heart failure, the most frequent cause of which is slowlyincreasing coronary ischemia and weakening of the cardiac muscle.
Atherosclerosis as a Cause of Ischemic Heart Disease. Themost frequent cause of diminished coronary blood flow is atherosclerosis. The atherosclerotic process is discussed in connection with lipid metabolism. Briefly, this process is the following.
In people who have genetic predisposition to ath-erosclerosis, or in people who eat excessive quantities of cholesterol and have a sedentary lifestyle, large quantities of cholesterol gradually become deposited beneath the endothelium at many points in arteries throughout the body. Gradually, these areas of deposit are invaded by fibrous tissue and frequently become calcified. The net result is the development of athero-sclerotic plaques that actually protrude into the vessellumens and either block or partially block blood flow. A common site for development of atherosclerotic plaques is the first few centimeters of the major coro-nary arteries.
Acute Coronary Occlusion
Acute occlusion of a coronary artery most frequently occurs in a person who already has underlying ath-erosclerotic coronary heart disease but almost never in a person with a normal coronary circulation. Acute occlusion can result from any one of several effects, two of which are the following:
1. The atherosclerotic plaque can cause a local blood clot called a thrombus, which in turn occludes the artery. The thrombus usually occurs where the arteriosclerotic plaque has broken through the endothelium, thus coming in direct contact with the flowing blood. Because the plaque presents an unsmooth surface, blood platelets adhere to it, fibrin is deposited, and red blood cells become entrapped to form a blood clot that grows until it occludes the vessel. Or, occasionally, the clot breaks away from its attachment on the atherosclerotic plaque and flows to a more peripheral branch of the coronary arterial tree, where it blocks the artery at that point. A thrombus that flows along the artery in this way and occludes the vessel more distally is called a coronary embolus.
2. Many clinicians believe that local muscular spasm of a coronary artery also can occur. The spasm might result from direct irritation of the smooth muscle of the arterial wall by the edges of an arteriosclerotic plaque, or it might result from local nervous reflexes that cause excess coronary vascular wall contraction. The spasm may then lead to secondary thrombosis of the vessel.
Lifesaving Value of Collateral Circulation in the Heart. Thedegree of damage to the heart muscle caused either by slowly developing atherosclerotic constriction of the coronary arteries or by sudden coronary occlusion is determined to a great extent by the degree of collat-eral circulation that has already developed or that can open within minutes after the occlusion.
In a normal heart, almost no large communications exist among the larger coronary arteries. But many anastomoses do exist among the smaller arteries sized 20 to 250 micrometers in diameter, as shown in Figure 21–6.
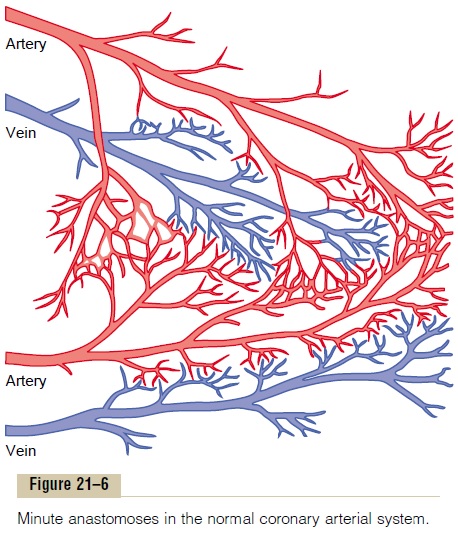
When a sudden occlusion occurs in one of the larger coronary arteries, the small anastomoses begin to dilate within seconds. But the blood flow through these minute collaterals is usually less than one half that needed to keep alive most of the cardiac muscle that they now supply; the diameters of the collateral vessels do not enlarge much more for the next 8 to 24 hours. But then collateral flow does begin to increase, dou-bling by the second or third day and often reaching normal or almost normal coronary flow within about 1 month. Because of these developing collateral chan-nels, many patients recover almost completely from various degrees of coronary occlusion when the area of muscle involved is not too great.
When atherosclerosis constricts the coronary arter-ies slowly over a period of many years rather than suddenly, collateral vessels can develop at the same time while the atherosclerosis becomes more and more severe. Therefore, the person may never experi-ence an acute episode of cardiac dysfunction. But, eventually, the sclerotic process develops beyond the limits of even the collateral blood supply to provide the needed blood flow, and sometimes the collateral blood vessels themselves develop atherosclerosis. When this occurs, the heart muscle becomes severely limited in its work output, often so much so that the heart cannot pump even normally required amounts of blood flow. This is one of the most common causes of the cardiac failure that occurs in vast numbers of older people.
Myocardial Infarction
Immediately after an acute coronary occlusion, blood flow ceases in the coronary vessels beyond the occlu-sion except for small amounts of collateral flow from surrounding vessels. The area of muscle that has either zero flow or so little flow that it cannot sustain cardiac muscle function is said to be infarcted. The overall process is called a myocardial infarction.
Soon after the onset of the infarction, small amounts of collateral blood begin to seep into the infarcted area, and this, combined with progressive dilation of local blood vessels, causes the area to become overfilled with stagnant blood. Simultaneously the muscle fibers use the last vestiges of the oxygen in the blood, causing the hemoglobin to become totally de-oxygenated. Therefore, the infarcted area takes on a bluish-brown hue, and the blood vessels of the area appear to be engorged despite lack of blood flow. In later stages, the vessel walls become highly permeable and leak fluid; the local muscle tissue becomes edematous, and the cardiac muscle cells begin to swell because of dimin-ished cellular metabolism.Within a few hours of almost no blood supply, the cardiac muscle cells die.
Cardiac muscle requires about 1.3 milliliters of oxygen per 100 grams of muscle tissue per minute just to remain alive. This is in comparison with about 8 mil-liliters of oxygen per 100 grams delivered to the normal resting left ventricle each minute. Therefore, if there is even 15 to 30 per cent of normal resting coronary blood flow, the muscle will not die. In the central portion of a large infarct, however, where there is almost no collateral blood flow, the muscle does die.
Subendocardial Infarction. The subendocardial musclefrequently becomes infarcted even when there is no evidence of infarction in the outer surface portions of the heart. The reason for this is that the subendocar-dial muscle has extra difficulty obtaining adequate blood flow because the blood vessels in the subendo-cardium are intensely compressed by systolic contrac-tion of the heart, as explained earlier. Therefore, any condition that compromises blood flow to any area of the heart usually causes damage first in the subendo-cardial regions, and the damage then spreads outward toward the epicardium.
Related Topics